Negative symptoms can be grouped into five domains: apathy/avolition, anhedonia, asociality, alogia, and affective flattening. There are few validate self-rated measures that assess these five dimensions. Therefore, this study aimed to validate the Self-Evaluation of Negative Symptoms (SNS) in Spanish patients with schizophrenia.
Material and methodsCross-sectional, validation study in 104 outpatients with schizophrenia evaluated using the Spanish version of the following scales: Clinical Assessment Interview for Negative Symptoms (CAINS), Positive and Negative Syndrome Scale (PANSS), Clinical Global Impression Scale for Schizophrenia (CGI-SCH), Personal and Social Performance (PSP), Motivation and Pleasure Scale – Self-Report (MAP-SR), 36-item Short-Form Health Survey (SF-36) and the Self-Evaluation of Negative Symptoms (SNS).
Results ReliabilityInternal consistency (Cronbach's alpha) was 0.915. Convergent validity: The Pearson correlation coefficient between MAP-SR and SNS Total scores was 0.660 (p<0.001). For PANSS-N, the correlation was 0.437 (p<0.005) and with the CAINS-Total was 0.478 (p<0.005). Divergent validity: The Pearson correlation coefficient between SNS and PSP was r=−0.372 (p≤0.001), and with SF-36 Physical and Mental Summary Component scores were r=−0.213 (p=0.066) and r=−0.144 (p=0.219), respectively. Discriminant validity: SNS Total scores were significantly statistically different according to the severity of the negative symptomatology rated by the CGI-SCH negative scale (p<0.001).
ConclusionThe SNS is a reliable and valid instrument to self-rate the five domains of negative symptoms in patients with schizophrenia and seems to be appropriate for use in everyday clinical practice as a complementary measure to the evaluation performed by the clinician.
Los síntomas negativos pueden agruparse en 5 dominios: apatía/abulia, anhedonia, conductas asociales, afasia y aplanamiento afectivo. Existen pocas medidas validadas autocalificadas que evalúen estas 5 dimensiones. Por tanto, el objetivo de este estudio fue validar la herramienta Self-Evaluation of Negative Symptoms (SNS, Autoevaluación de síntomas negativos) en pacientes españoles esquizofrénicos.
Material y métodosEstudio transversal de validación en 104 pacientes esquizofrénicos externos, evaluados utilizando la versión española de las escalas siguientes: Clinical Assessment Interview for Negative Symptoms (CAINS), Positive and Negative Syndrome Scale (PANSS), Clinical Global Impression Scale for Schizophrenia (CGI-SCH), Personal and Social Performance (PSP), Motivation and Pleasure Scale-Self-Report (MAP-SR), 36-item Short-Form Health Survey (SF-36) y la SNS.
Resultados Respecto a la fiabilidad,la consistencia interna (α de Cronbach) fue de 0,915. En cuanto a validez convergente, el coeficiente de correlación de Pearson entre las puntuaciones totales de MAP-SR y SNS fue de 0,660 (p < 0,001). Para PANSS-N, la correlación fue de 0,437 (p < 0,005) y de 0,478 (p < 0,005) con CAINS-Total. Respecto a la validez divergente, el coeficiente de correlación de Pearson entre las puntuaciones SNS y PSP fue de r = –0,372 (p ≤ 0,001) y con las puntuaciones de SF-36 Physical and Mental Summary Component fueron de r = −0,213 (p = 0,066) y r = −0,144 (p = 0,219), respectivamente. En la validez discriminante, las puntuaciones totales de SNS fueron diferentes desde un punto de vista estadístico significativo, conforme a la gravedad de la sintomatología negativa calificada por la escala negativa CGI-SCH (p < 0,001).
ConclusiónSNS es un instrumento fiable y válido para autocalificar los 5 dominios de los síntomas negativos en pacientes esquizofrénicos y parece adecuado para utilizarlo en la práctica clínica diaria como medida complementaria a la evaluación realizada por el clínico.
The negative symptoms of schizophrenia, defined as the absence or diminution of normal behaviors and functions, have been recognized since the beginning of the XX century.1 These symptoms account for much of the long-term morbidity2 and there is increasing evidence of their negative impact on social functioning and quality of life of patients with schizophrenia.3,4 All of this has fostered a consensus about their status as a distinct and important therapeutic domain.5
An adequate evaluation of negative symptoms is essential to perform a specific and personalized treatment. Nowadays, their assessment is challenging due to the low inter-rater reliability and the interrelations with other dimensions, such as depression, extrapyramidal symptoms, social withdrawal secondary to positive symptoms, and institutionalization.6,7 Moreover, the principal psychometric tools used are scales based on the evaluation carried out by an independent observer. In them, the result can be significantly affected by researchers’ experience and subjective assessment.8
In the last years, the use of patient-reported outcome measures (PROMs) is expanding in clinical medicine as they place patients at the center of the decision-making process.9,10 Also, self-assessment is a time-efficient method for the identification of negative symptoms and could be useful for detecting negative symptoms in the early stages of schizophrenic disease.11
Examples of second-generation disease-specific PROMs for the negative symptoms of schizophrenia are the Motivation and Pleasure Scale – Self-Report (MAP-SR),12 an 18-item self-report version of the CAINS Motivation and Pleasure subscale and the Self-Evaluation of Negative Symptoms (SNS).14 Lincoln et al.11 analyzed the self-reported measures of negative symptoms and point out that one of the advantages presented by the SNS over the other self-report measures is the coverage of the five negative dimensions required by the consensus conference: apathy/avolition, anhedonia, asociality, alogia, and affective flattening.5 Also, patients with schizophrenia and schizoaffective disorder have demonstrated the ability to complete the SNS reliably and consistently.8,14,15
Therefore, the purpose of this study was to adapt and validate the SNS into European Spanish and assess its psychometric properties (including floor and ceiling effects, reliability, construct and discriminant validity) in Spanish patients with schizophrenia.
Material and methodsStudy designThis is a cross-sectional, naturalistic study designed to validate the Spanish version of a new self-report instrument, the SNS, for assessing the five dimensions of negative symptoms. It was approved by the Ethics Committee for Clinical Research of the Hospital Universitario Central de Asturias, Oviedo, Spain (ref. n° 140/15), and was conducted following the ethical principles of the Declaration of Helsinki and Good Clinical Practice.
ParticipantsA sample of 104 subjects who completed the SNS was analyzed. Inclusion criteria were (1) outpatients with a diagnosis of schizophrenia according to ICD-10 criteria; (2) older than 17 years of age; (3) currently in treatment; and (4) written informed consent to participate in the study. Exclusion criteria were designed to be minimal, due to the nature of the study, and only persons with intellectual developmental disorder, acquired brain injury, or who refused to participate in the study were excluded.
Psychometric measuresClinician-reported outcome measures (CROMs)Participants were assessed by trained clinicians. The assessment included an ad hoc questionnaire for collecting demographic and clinical information and the Spanish versions of the following instruments: The Clinical Assessment Interview for Negative Symptoms (CAINS),15 the Positive and Negative Syndrome Scale (PANSS),16 and the Clinical Global Impression scale for Schizophrenia (CGI-SCH)17 were administered to assess the level of psychopathology, and specifically the presence and severity of negative symptoms of schizophrenia. Besides, we used the Personal and Social Performance scale (PSP)18 for assessing the level of functioning.
Regarding the PANSS scale, we use both the negative scale (PANSS-N) and the Marder negative factor (PANSS-MNF).19 The PANSS-MNF consists of 7 items and includes the symptoms of the PANSS-N, except for the difficulty in abstract thinking and stereotyped thinking, plus two on the PANSS General Psychopathology scale, motor retardation and active social avoidance.
Patient-reported outcome measures (PROMs)The Self-Evaluation of Negative Symptoms (SNS)13 was developed to self-rate the five domains of the negative syndrome. It provides a separate score for each domain as well as a total score for negative symptoms and signs. It consists of 20 items organized into the following five subscales: social withdrawal (items 1–4), diminished emotional range (items 5–8), alogia (items 9–12), abulia (items 13–16), and anhedonia (items 17–20). The total score is the sum of the scores on all the items, ranging from 0 to 40, where the higher the score, the greater the severity of the self-rated negative symptoms. The five domain scores are obtained by adding the scores on the items of each domain, and in the five domains, they range between 0 and 8.
Two independent Spanish clinicians who are fluent French (TBB and AP) first translated the original instrument into Spanish. Then, a French psychiatrist (PC) fluent in Spanish back-translated the Spanish version, and finally, the original authors approved it.
The Spanish version of the Motivation and Pleasure Scale – Self-Report (MAP-SR)20 was used to self-rate the severity of their anhedonia and avolition. Finally, to assess their self-perceived health status, patients completed the Spanish version of the MOS 36-item Short-Form Health Survey (SF-36).21
Statistical analysisThe statistical analysis was done using the IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp, Released 2016). All analyses were two-tailed, and the level of significance was set at p<0.05.
Firstly, a descriptive analysis of the SNS distribution scores was performed, including mean and standard deviation, kurtosis, skewness, floor and ceiling effects, and Kolmogorov-Smirnov test. The internal consistency of the SNS was calculated using the Cronbach's alpha coefficient at the item level.
To calculate convergent and divergent validities, we used the Pearson correlation coefficient between PROMs to avoid the “rater confounder factor” seen in other studies, since it was clinicians and not patients themselves who did the ratings. Thus, for determining their convergent validity, we performed bivariate correlations between the Spanish versions of the SNS and MAP-SR, in addition to PANSS and CAINS. On the other hand, to calculate the divergent validity, we did the same analysis between the SNS scores and the PSP and SF-36 scores. Furthermore, the ability of the SNS to discriminate between the different levels of the negative symptoms identified by the CGI-N subscale was determined using the ANOVA test (Duncan post-hoc).
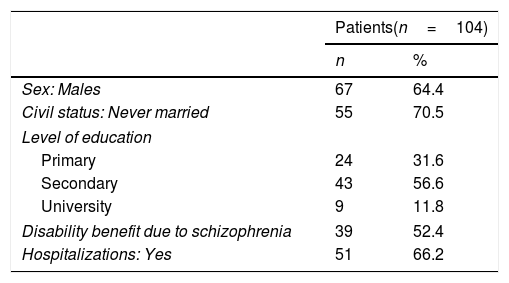
ResultsThe mean age of the patients was 40.1 (sd=13.9), 64.4% were males, and the mean of years of disease evolution was 11.8 (sd=12.1). Table 1 shows demographic and clinical characteristics for patients.
Demographic and clinical characteristics of participants.
| Patients(n=104) | ||
|---|---|---|
| n | % | |
| Sex: Males | 67 | 64.4 |
| Civil status: Never married | 55 | 70.5 |
| Level of education | ||
| Primary | 24 | 31.6 |
| Secondary | 43 | 56.6 |
| University | 9 | 11.8 |
| Disability benefit due to schizophrenia | 39 | 52.4 |
| Hospitalizations: Yes | 51 | 66.2 |
| Mean | Sd | |
|---|---|---|
| Age | 40.1 | 13.9 |
| Level of education | ||
| Years of education | 13.0 | 4.2 |
| Years repeated | 1.5 | 0.7 |
| Length of illness | 11.8 | 12.1 |
| Number of hospitalizations | 2.1 | 1.7 |
| Psychometric evaluation scores | ||
| CAINS-Total | 29.5 | 12.0 |
| CAINS-MAP | 21.9 | 9.0 |
| CAINS-EXP | 7.6 | 3.9 |
| PANSS-Positive | 13.2 | 5.6 |
| PANSS-Negative | 19.2 | 5.0 |
| PANSS-Marder negative factor | 19.1 | 5.6 |
| PANSS-General psychopathology | 29.9 | 7.4 |
| CGI-SCH Globala | 4.3 | 0.9 |
| CGI-SCH Positive | 3.0 | 1.5 |
| CGI-SCH Negative | 3.9 | 1.0 |
| CGI-SCH Depressive | 2.0 | 1.1 |
| CGI-SCH Cognitive | 3.3 | 1.3 |
| PSP-Totala | 51.1 | 17.7 |
| SF-36 Physical functioning | 68.0 | 26.0 |
| SF-36 Physical role functioning | 49.7 | 40.0 |
| SF-36 Bodily pain | 45.4 | 14.0 |
| SF-36 General health perceptions | 60.6 | 11.6 |
| SF-36 Vitality | 61.0 | 13.5 |
| SF-36 Social functioning | 47.7 | 14.4 |
| SF-36 Emotional role functioning | 58.4 | 42.7 |
| SF-36 Mental health | 60.2 | 13.2 |
| SF-36 Physical component summary | 43.3 | 7.1 |
| SF-36 Mental component summary | 39.7 | 7.0 |
| MAP-SR | 29.7 | 11.2 |
| SNS-Total | 16.1 | 9.3 |
| SNS-Social withdrawal | 2.8 | 2.2 |
| SNS-Diminished emotional range | 3.0 | 2.2 |
| SNS-Alogia | 3.8 | 2.6 |
| SNS-Avolition | 3.8 | 2.3 |
| SNS-Anhedonia | 2.6 | 2.3 |
sd: standard deviation.
CAINS: Clinical Assessment Interview for Negative Symptoms; CAINS-EXP: Expression subscale; CAINS-MAP: Motivation and Pleasure subscale; MAP-SR: Motivation and Pleasure Scale – Self-Report; PANSS: Positive and Negative Syndrome Scale; SF-36: The 36-Item Short-Form Health Survey questionnaire; SNS: Self-Evaluation of Negative Symptoms
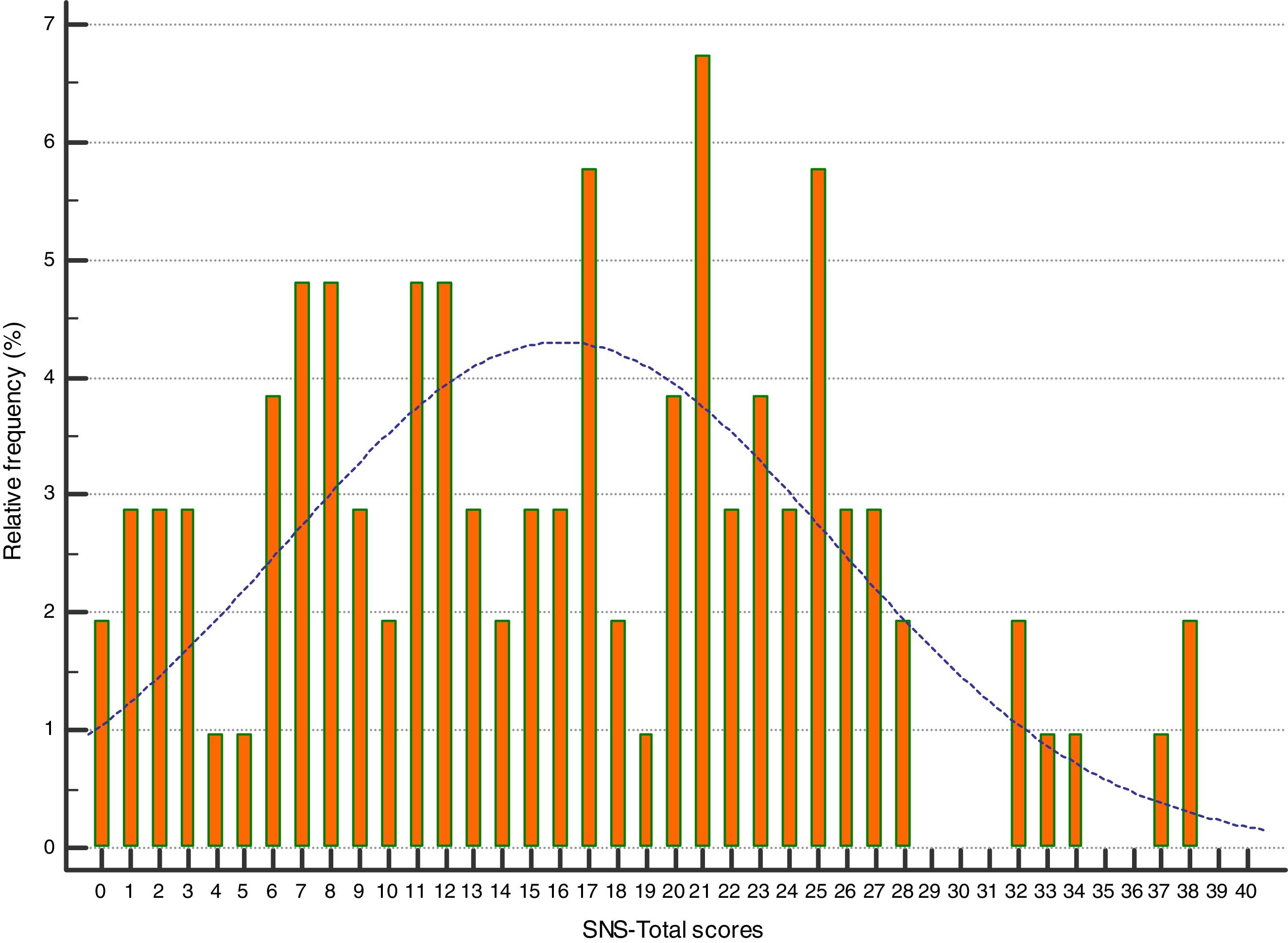
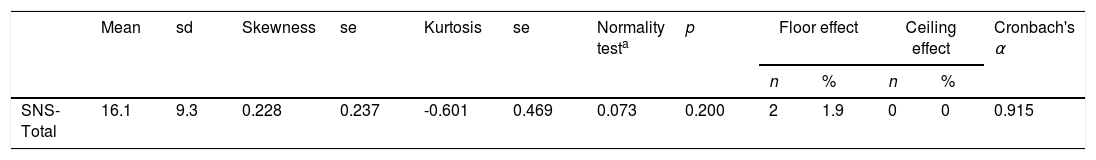
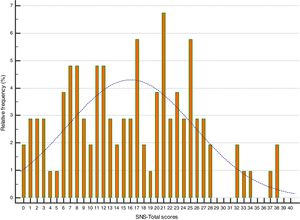
The mean SNS Total score was 16.1 (9.3). It showed a symmetrical, mesokurtic and normal distribution without floor and ceiling effects (see Table 2 and Fig. 1).
Descriptive analysis of the total Self-Evaluation of Negative Symptoms (SNS) score.
| Mean | sd | Skewness | se | Kurtosis | se | Normality testa | p | Floor effect | Ceiling effect | Cronbach's α | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||||||||
| SNS-Total | 16.1 | 9.3 | 0.228 | 0.237 | -0.601 | 0.469 | 0.073 | 0.200 | 2 | 1.9 | 0 | 0 | 0.915 |
sd: standard deviation; se: standard error; SNS: Self-Evaluation of Negative Symptoms.
The SNS had good internal consistency for patients with schizophrenia (Cronbach's α=0.915), and all Corrected Item-Total Correlation values were >0.3, ranging between 0.468 for item 11 and 0.729 for item 19.
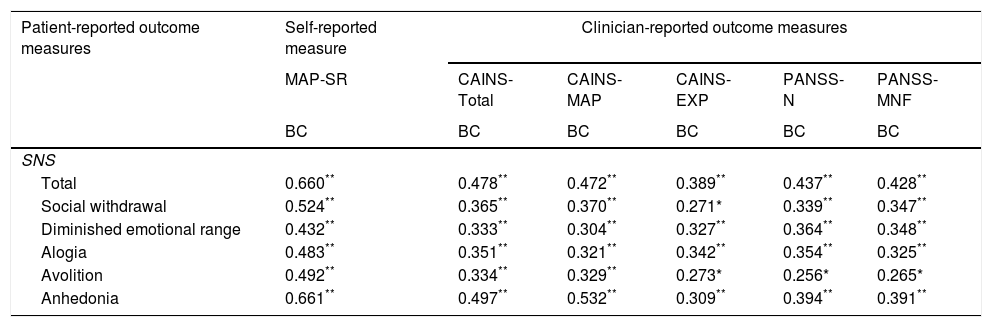
Convergent validityThe results reflect a moderate convergent validity with the other self-rated measure of negative symptoms of schizophrenia, the MAP-SR (r=0.660, p<0.001). The Pearson correlation coefficient was significant between the MAP-SR and all the SNS subscales scores. This correlation was greater with the Anhedonia subscale (r=0.661, p<0.001) and lower with the Diminished Emotional Range subscale (r=0.432, p<0.001).
Furthermore, we analyzed the Pearson correlation between SNS and the CROMs. The coefficients between the SNS and the PANSS-MNF and PANSS-N were 0.428 and 0.437 (p<0.001) respectively (Table 3). In addition, there was a significant positive correlation between SNS and Total CAINS (r=0.478, p<0.001) and its subscales, the CAINS-MAP (r=0.472, p<0.001) and the CAINS-EXP (r=0.389, p<0.001) (Table 3).
Convergent validity between the Self-Evaluation of Negative Symptoms (SNS), the Motivation and Pleasure Scale – Self-Report (MAP-SR), the Clinical Assessment Interview for Negative Symptoms (CAINS), and the Positive and Negative Syndrome Scale (PANSS).
| Patient-reported outcome measures | Self-reported measure | Clinician-reported outcome measures | ||||
|---|---|---|---|---|---|---|
| MAP-SR | CAINS-Total | CAINS-MAP | CAINS-EXP | PANSS-N | PANSS-MNF | |
| BC | BC | BC | BC | BC | BC | |
| SNS | ||||||
| Total | 0.660** | 0.478** | 0.472** | 0.389** | 0.437** | 0.428** |
| Social withdrawal | 0.524** | 0.365** | 0.370** | 0.271* | 0.339** | 0.347** |
| Diminished emotional range | 0.432** | 0.333** | 0.304** | 0.327** | 0.364** | 0.348** |
| Alogia | 0.483** | 0.351** | 0.321** | 0.342** | 0.354** | 0.325** |
| Avolition | 0.492** | 0.334** | 0.329** | 0.273* | 0.256* | 0.265* |
| Anhedonia | 0.661** | 0.497** | 0.532** | 0.309** | 0.394** | 0.391** |
BC: Bivariate correlations (n=94).
CAINS: Clinical Assessment Interview for Negative Symptoms; CAINS-MAP: Motivation and Pleasure subscale; CAINS-EXP: Expression subscale; MAP-SR: Motivation and Pleasure Scale – Self-Report; PANSS: Positive and Negative Syndrome Scale; PANSS-N: Negative scale; PANSS-MNF: Marder negative factor; SNS: Self-Evaluation of Negative Symptoms.
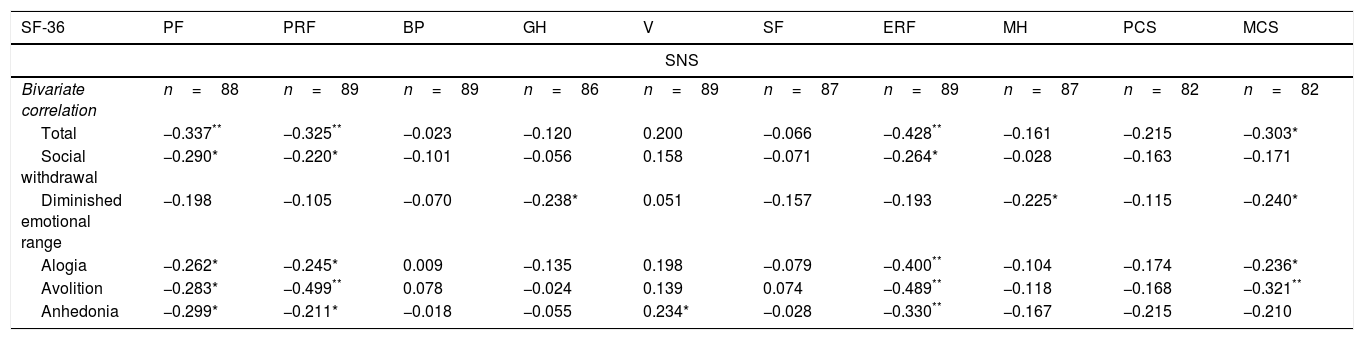
Self-assessment of negative symptomatology (SNS) and clinician-rated functioning (PSP) were found to be moderately positively correlated [r=−0.372 (p<0.001)]. On the other hand, we found very good divergent validity with self-perceived health status evaluated using the SF-36. Specifically, the Pearson correlation coefficients between total SNS and Physical and Mental Summary Components scores of the SF-36 were r=−0.213, (p=0.066) and r=−0.144, (p=0.219), respectively. In Table 4, we show the Pearson correlation coefficients between the SNS and SF-36 subscales.
Divergent validity between the Self-Evaluation of Negative Symptoms (SNS) and the 36-Item Short-Form Health Survey questionnaire.
| SF-36 | PF | PRF | BP | GH | V | SF | ERF | MH | PCS | MCS |
|---|---|---|---|---|---|---|---|---|---|---|
| SNS | ||||||||||
| Bivariate correlation | n=88 | n=89 | n=89 | n=86 | n=89 | n=87 | n=89 | n=87 | n=82 | n=82 |
| Total | −0.337** | −0.325** | −0.023 | −0.120 | 0.200 | −0.066 | −0.428** | −0.161 | −0.215 | −0.303* |
| Social withdrawal | −0.290* | −0.220* | −0.101 | −0.056 | 0.158 | −0.071 | −0.264* | −0.028 | −0.163 | −0.171 |
| Diminished emotional range | −0.198 | −0.105 | −0.070 | −0.238* | 0.051 | −0.157 | −0.193 | −0.225* | −0.115 | −0.240* |
| Alogia | −0.262* | −0.245* | 0.009 | −0.135 | 0.198 | −0.079 | −0.400** | −0.104 | −0.174 | −0.236* |
| Avolition | −0.283* | −0.499** | 0.078 | −0.024 | 0.139 | 0.074 | −0.489** | −0.118 | −0.168 | −0.321** |
| Anhedonia | −0.299* | −0.211* | −0.018 | −0.055 | 0.234* | −0.028 | −0.330** | −0.167 | −0.215 | −0.210 |
SF-36: The 36-Item Short-Form Health Survey questionnaire; PF: Physical Functioning; PRF: Physical Role Functioning; BP: Bodily Pain; GHP: General Health Perceptions; V: Vitality; SF: Social Functioning; ERF: Emotional Role Functioning; MH: Mental Health; PCS: Physical Component Summary; MCS: Mental Component Summary; SNS: Self-Evaluation of Negative Symptoms.
To calculate the discriminant validity of the SNS, we created three levels of severity of negative symptomatology based on the distribution of scores on the CGI-SCH negative subscale in our sample: mild [including scores 2 and 3, n=26 (29.9%)], moderate [score 4, n=37 (42.5%)], and severe [scores 5 and 6, n=24 (27.6%)]. The Spanish version of the SNS was able to discriminate among the 3 groups (F=31.172, p<0.001). Duncan's post-hoc test revealed that the scores in the 3 groups were statistically different from each other [mild level: SNS score=7.9 (6.1); moderate level: SNS=18.9 (7.8); and severe level: SNS score=23.2 (7.3)].
DiscussionThe purpose of this study was to adapt and validate the Spanish version of the SNS in a sample of Spanish outpatients with stable schizophrenia. We demonstrate that the new scale has adequate psychometric properties in this population and therefore, may be used to obtain information on these symptoms from the point of view of the patients.
The internal consistency of the overall scale was adequate and similar to the previous studies.8,14,15 For convergent validity, we found a significant correlation between the SNS and the other self-reported scale used in this study, the MAP-SR, indicating strong convergent validity. According to Dollfus et al.,13 the evaluation of emotional symptoms is a strength of the SNS. This scale allows patients to express their motivation and pleasure deficit, as well as their loss of emotion regardless of depressed mood.13 Moreover, in contrast with the MAPS-SR, the SNS is an instrument that assesses diminished emotional range, social withdrawal and alogia. Therefore, it may be useful to evaluate the five-factor structure domains underlying negative symptoms proposed by Ahmed et al.22 Similarly, moderate to low correlations were found with the CAINS subscales. Besides, as can be expected, higher coefficients were found between the SNS subscales that evaluate expressive symptoms (alogia and emotional range) and the CAINS-EXP subscale, although the difference is really small. The same result was found for the SNS subscales evaluationg social withdrawall, avolition and anhedonia and the CAINS-MAP subscale. The fact that the highest coefficients were obtained between the SNS subscales assessing motivational aspects and the CAINS-MAP may reflect a greater difficulty for patients to identify their expressive deficits, in congruence with the results of Lincoln et al.11 In fact, the self-rated version of the CAINS-EXP was retired due to its limited psychometric properties. On the other hand, as expected, the correlations between the SNS and the CAINS-Total, PANSS-N, and PANSS-MNF were lower, which indicates a greater convergent validity between self-report measures, eliminating the “confounding factor of the evaluator” seen in other studies. However, it merits to note that the correlation coefficients obtained were very similar (from 0.478 with the CAINS-Total to 0.428 with the PANSS-MNF) independently of the clinician-rated instrument employed. It is true that the highest coefficient was found with the second-generation instrument employed, but the lowest was found with the Marder negative factor which has been proposed as an alternative to the PANSS negative scale to assess negative symptoms.19,23
Divergent validity was calculated against the PSP and the SF-36. A moderate to low correlation coefficient was found between the PSP and the SNS. This result is, to some extent, unexpected since negative symptoms, along with cognitive deficits, are the most consistent predictive variables of real-world functioning found in the literature.23 However, some years ago we argued that the high correlations reported between these two constructs were due in part to the redundancy in their measurement when the PANSS was used to rate negative symptoms, due to its well-known limitations.23 In this study, the negative symptomatology was assessed by the SNS, a self-rated second-generation instrument based on inner experiences rather than in behaviors. This could explain that our correlation coefficient, although statistically significant, is lower than that previously reported and that obtained in this same study between the PSP and the PANSS-N (r=−0.580, p<0.001). Furthermore, the percentage of the variance explained by each instrument in the scores of the other is only 13.8%, which suggests a rather good divergent validity between the SNS and the PSP, demonstrating that both instruments measure different although related constructs. Concerning the divergent validity between SF-36 and SNS, we found low associations indicating robust divergent validity. However, significant associations were found with physical and emotional functioning; these results are consistent with the literature, where negative symptoms and quality of life were negatively related.24 Even Andrianarisoa et al.25 found that psychotic symptoms do not have the same impact on the quality of life, where negative symptoms generated an affectation in more areas compared to positive symptoms.
In spite of the different sources of ratings, we were able to demonstrate that the SNS (patient-rated) has a good discriminant validity to identify the different levels of severity rated by clinicians (CGI-SCH negative subscale). Up to our knowledge, results on this psychometric property has not been reported for the SNS.
Finally, it is important to know that this scale has also been validated in Spanish adolescents as an instrument to evaluate negative symptoms in a general population of adolescents.26 The authors suggest that this scale could be useful for assessing early prodromal symptoms of schizophrenia in adolescents.
The present study has some limitations, the cross-sectional design of the study that does not allow us to obtain information about the ability of the SNS to detect changes in these patients. Another limitation was that all patients were outpatients from the same region of Spain (Asturias), and there was a lack of patients with extremely severe negative symptoms. In spite of these limitations, this study has different strengths, such as the sample size and inclusion criteria. Compared with previous studies, our sample is considerably larger, and all patients included had a diagnosis of schizophrenia, while in the majority of the published studies, patients with schizoaffective disorder were also included.13,14
Our study has shown that the Spanish version of the SNS is a reliable and valid instrument to self-rate the five domains of negative symptoms in patients with schizophrenia. Moreover, this scale has several advantages, is a short and easily understandable scale for patients, and a time-efficient method for the identification of these symptoms. Therefore, the SNS seems to be appropriate for use in everyday clinical practice as a complementary means to obtain patients’ perception of their negative symptoms.
Funding sourceThis work has been financially supported by BICIBERSAM, the Government of the Principality of Asturias PCTI-2018-2022 IDI/2018/235, and Fondos Feder.
Conflict of interestThe authors declare that there is no conflict of interest with the subject of this research. The funding sources had no participation in the development of this study.