Corynebacterium tuberculostearicum is a Gram positive bacillus from the skin microbiota. Sometimes it can produce recurrent fistulous mastitis associated with granulomas. Its prevalence is very low. The initial therapeutic approach is important to avoid progression. The histopathological and microbiological study is essential for its diagnosis. Differential diagnosis is made with tumor pathology. There is no established therapeutic scheme to which we can adhere. The initial treatment should be antibiotic therapy adjusted by antibiogram and corticosteroids. The evolution can be torpid despite correct treatment. In these cases, surgical treatment with partial or total resections of the breast can be considered.
We present the case of a 44-year-old woman who came to the consultation with pain and induration in the lower internal quadrants of the left breast with the formation of fistulous tracts of years of evolution despite antibiotic and corticosteroid treatment.
El C. Tuberculostearicum es un Bacilo Gram positivo de la microbiota de la piel. En ocasiones puede producir mastitis fistulosas de repetición asociadas a granulomas. Su prevalencia es muy baja. El abordaje terapeútico inicial es importante para evitar progresión. El estudio histopatológico y microbiológico es fundamental para su diagnóstico. El diagnóstico diferencial se realiza con la patología tumoral. No existe un esquema terapéutico establecido al cual nos podamos ceñir. El tratamiento inicial debe ser antibioterapia ajustada por antibiograma y corticoides. La evolución puede ser tórpida a pesar de un tratamiento correcto. En estos casos, se puede plantear un tratamiento quirúrgico con resecciones parciales, o totales de la mama.
Presentamos el caso de una mujer de 44 años que acude a la consulta con dolor e induración en cuadrantes inferointernos de mama izquierda es con formación de trayectos fistulosos de años de evolución a pesar de tratamiento antibiótico y corticoideo.
Corynebacterium tuberculostearicum is part of the skin microbiota. It is difficult to distinguish between infection, colonization and contamination of this organism. It is a pleomorphic Gram positive bacteria. An association has been seen between Corynebacterium and infections after orthopedic surgery, leprosy-like lesions or mastitis.1 Our goal is to review the treatments that we can offer to a patient with a breast infection due to Corynebacterium tuberculostearicum based on a clinical case.
Clinical case40-year-old patient with no relevant history, a native of Colombia who has lived in Spain for 16 years. She has two children, her last pregnancy was 5 years ago. She breastfed for 8 months. She has been on contraceptive treatment in the last year.
She came to the consultation due to severe pain in the left breast and a mammary tumor with recurrent fistulas with pus draining on two occasions.
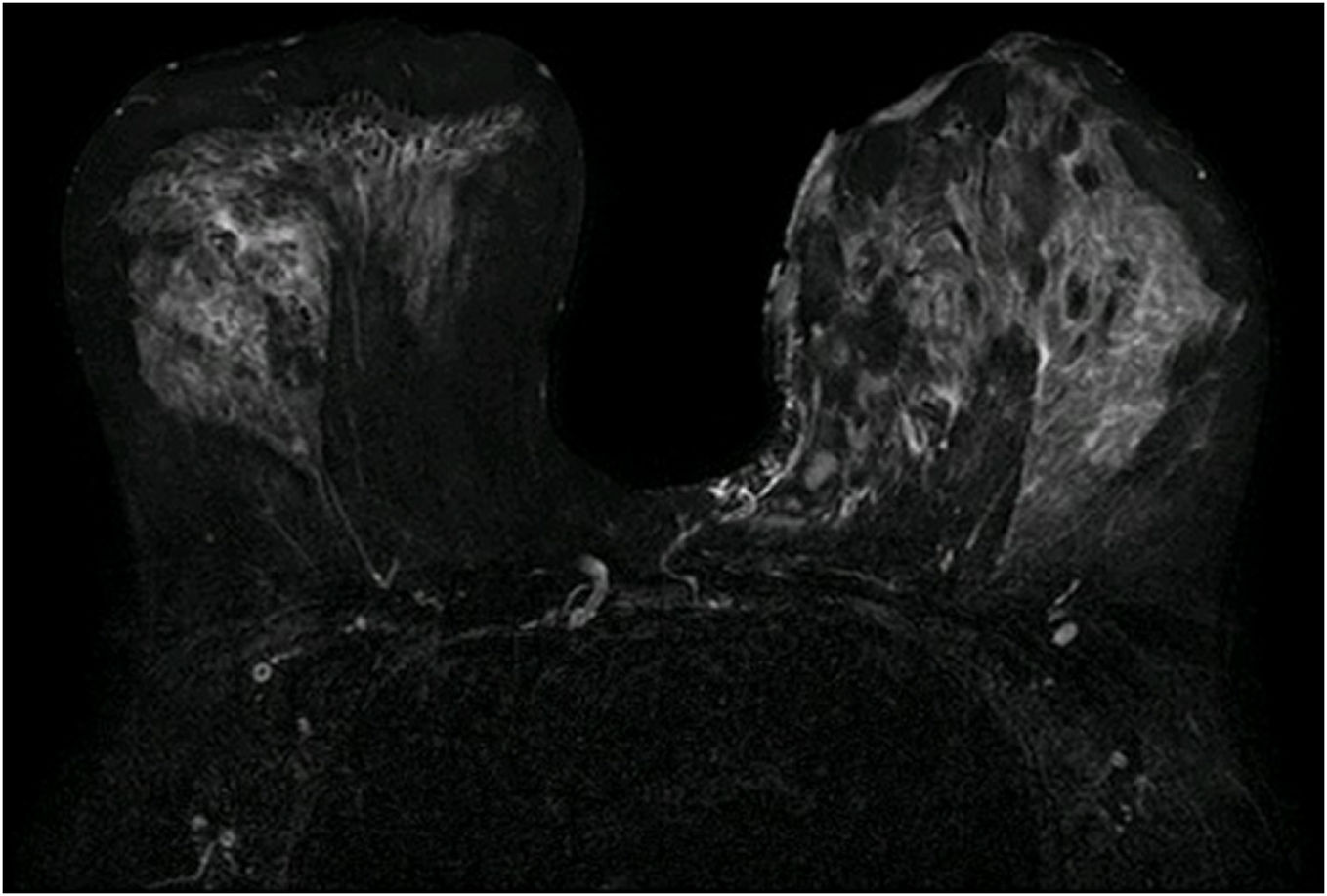
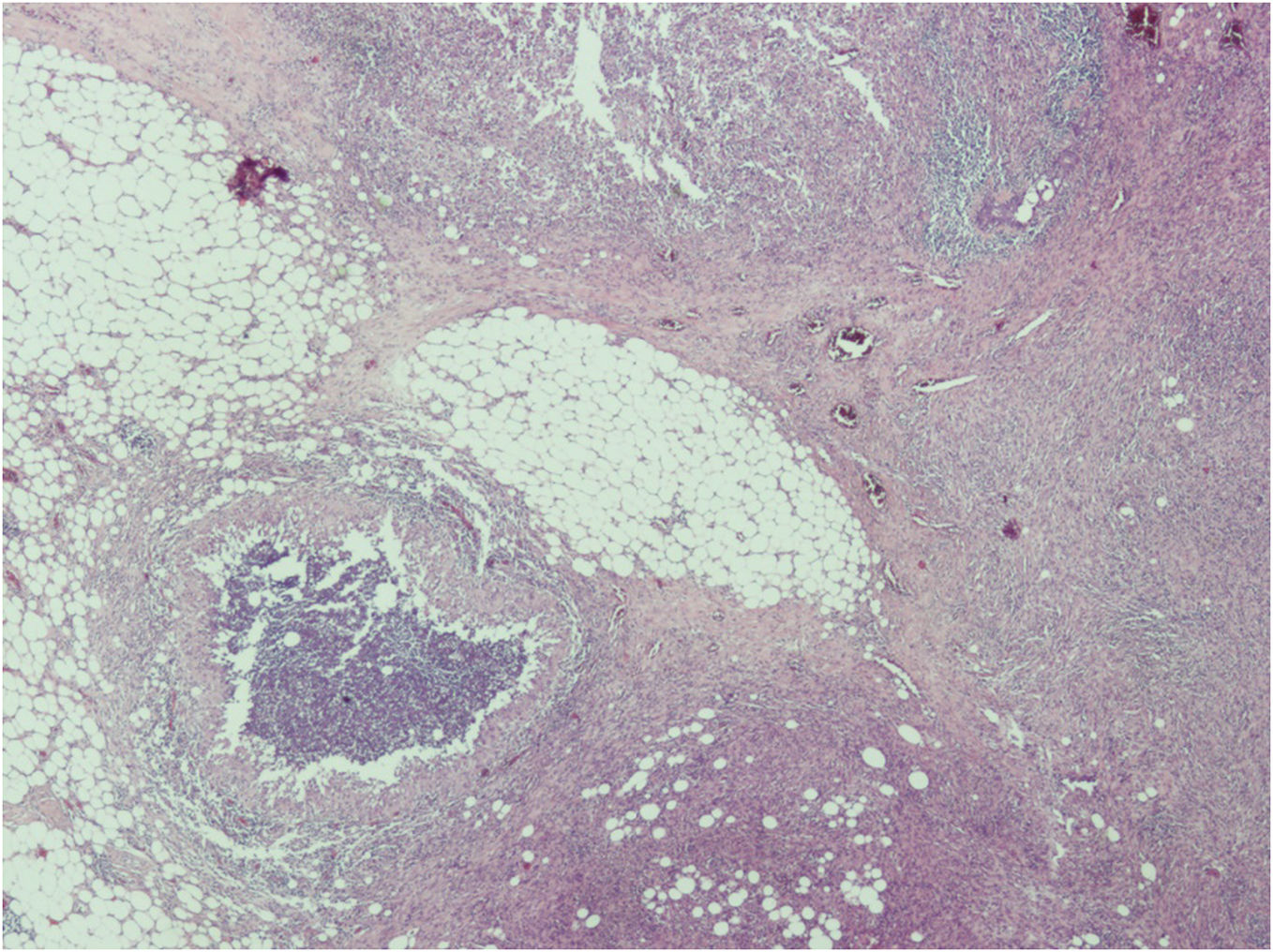
Mammography, ultrasound and MRI revealed areas of increased density and collections with fistulous tracts to the skin (Fig. 1). In the biopsy, there were no cellular alterations. Histologically, the biopsy shows lobular and interlobal inflammation with necrotic and hemorrhagic focus and granulomas (Fig. 2) without the presence of microorganisms. Suggestive of granulomatous lobar mastitis. The microbiological study was only positive for Corynebacterium tuberculestearicum in two of five samples.
In the first episode, she was treated with amoxicillin 875 mg/8 h for a month. After showing no improvement, she was admitted with intravenous corticosteroid treatment and drainage of mammary collections. Once the acute process had been controlled, she was maintained for three months with doxycycline 100 mg/12 h, followed by ciprofloxacin 500 mg/12 h for one month and clindamycin 600 mg/8 h until complete resolution of the condition was achieved. In the second episode, amoxicillin was started again for a month with clinical improvement.
One year after the first episode, she presented the same infectious process in the contralateral breast with new fistulous tracts and intense pain, being the microbiological study only positive for Corynebacterium sensitive to penicillin, ciprofloxacin and linezolid. Treatment was carried out with ciprofloxacin 750 mg/12 h for 15 days. After stopping antibiotics, she developed new infections twice. Maintenance antibiotic treatment was decided until CRP normalization and subsequent surgical treatment. Surgical treatment was decided due to the patient's pain. In this interval, tests are done to rule out lupus, sarcoidosis and tuberculosis. As well as, the patient stopped contraceptives.
Bilateral breast reduction, Thorek-type pattern, was performed, maintaining antibiotics until the intervention. The final anatomy shows exacerbated chronic inflammation without the presence of microorganisms.
One year after the intervention, the patient has not presented new episodes of mastitis.
DiscussionCorynebacteria are implicated in recurrent fistulous mastitis. Cases associated with: Corynebacterium minutissimum, amycolatum, kroppenstedtii, accolens and tuberculostearicum, among others, have been described. The initial approach is important since the delay entails disease progression and limiting physical and psychological discomfort.
Corynebacteria infections can appear to be tumors both clinically and radiologically, so a differential diagnosis must be made.2
Imaging tests such as mammography, ultrasound and MRI can help in the differential diagnosis.3 For the diagnosis, a biopsy with histological and microbiological study is necessary.4
To date, it is unknown whether Corynebacterium infection can be the cause of granulomatous mastitis or superinfection of granulomatous mastitis.
The etiology of granulomatous mastitis is unknown, being considered in many cases ideopathic, they have been related to autoimmune causes,5 contraceptives, secretions, trauma and infections.6
The average age of appearance of granulomatous mastititis is usually 35 years, patients who have had children and have breastfed.7
Histologically, the granulomas of granulomatous mastitis are lobule-centered, can be suppurative, and be associated with microabscesses. They are also associated with cavities due to dissolution of lipids. Granulomas have a specific appearance with an outer sleeve of histiocytes and giant cells surrounding a collection of polymorphonuclear cells with voids due to fatty solutions. These granulomas are also called suppurative lipogranulomas.
Tuberculosis, Wegener's granulomatosis, giant cell arteritis, polyarteritis nodosa, syphilis, sarcoidosis, parasitic and fungal infections should be ruled out.
Wilson and Yau recommend for the management of superinfected granulomatous mastitis:8
1. Initial antibiotic treatment against the susceptibility of the pathogen, the dose and duration being higher when dealing with soft tissues. It may take months to control the disease.
2. Corticosteroid treatment at a dose of 0.6 mg/kg/day.
3. Partial resections or mastectomy in recurrent cases.
Both medical and surgical treatment are usually effective, but monitoring of granulomatous mastitis should be long-term due to the possibility of recurrence, especially in cases with pain and fistulas.9 Corticosteroids can also be useful after relapse after surgical resection.10 Tuli proposes a dose of 0.8 mg/kg/day. Treatment with chronic methotrexate (10 mg/week) or azatrioprine may be a maintenance option for non-superinfected recurrent mastitis.11
FundingThe authors declare that they did not receive any funding for the elaboration of this paper.
Confidentiality of dataThe authors declare that they have followedand the protocols of their Centre on the publication of patient data.