Sudden unexpected death in epilepsy (SUDEP) is a major cause of mortality in young epileptic patients. The objective of the work is to analyse its frequency and clinical–pathological characteristics as a cause of sudden death in epileptics under 35 years of age.
MethodsRetrospective population study of all SUDEP in people aged 1–35 years in Bizkaia (period 1991–2021) and Seville (2004–2021) investigated in the Forensic Pathology Services (FPS). In each case, a complete autopsy was carried out with histopathological and toxicological studies, and review of clinical and circumstantial data. Data from the Mortality Registry for deaths by epilepsy were examined.
Results101 deaths due to epilepsy were registered in the Mortality Registries and 46 SUDEP cases in the FPS, representing 6% of forensic sudden deaths in this age population. A high frequency of post-traumatic epilepsy cases (n=5), brain abnormalities (n=5), or epilepsy associated to developmental disorders (n=4) or mental retardation (n=3) was observed. The toxicological analysis was positive in 75%, highlighting the presence of antiepileptic drugs (n=26). Illegal drugs were detected in 5 young people, mainly cocaine (n=3). Death was unwitnessed in most subjects (85%) and occurred at night (n=63%) while sleeping.
ConclusionsSUDEP in children and young people is infrequent, however, it is an important cause of mortality in epileptics. Although the mechanisms are not well understood, it is recommended to strengthen the medical control of epilepsy in youth, mainly in patients with post-traumatic or post-surgical epilepsy or in those who have associated developmental disorders or mental retardation.
La muerte súbita inexplicada en la epilepsia (MSIEP) es una causa importante de mortalidad en pacientes epilépticos jóvenes. Sin embargo, su existencia es poco conocida en el ámbito forense. El objetivo del trabajo es analizar la frecuencia y características clínico-patológicas de la MSIEP en epilépticos menores de 35 años.
MétodosEstudio observacional de todas MSIEP ocurridas en personas de 1–35 años en Bizkaia (periodo 1991–2021) y Sevilla (2004–2021) investigadas en los Servicios de Patología Forense (SPF). Además, se examinaron las muertes por epilepsia de los Registro de Mortalidad.
ResultadosSe registraron 101 muertes por epilepsia en los Registros de Mortalidad y 46 MSIEP en los SPF, representado el 6% de las muertes súbitas en esta edad. Se registró una alta frecuencia de casos de epilepsia postraumática (n = 5), o con anomalías cerebrales (n = 5) o asociadas a trastornos del desarrollo (n = 4) o retraso mental (n = 3). El estudio toxicológico fue positivo en el 75%, destacando la presencia de fármacos antiepilépticos (n = 26). Se detectaron drogas ilegales en 5 jóvenes, principalmente cocaína (n = 3). La muerte fue no presenciada en la mayoría de los sujetos (85%) y sucedió por la noche (n = 63%) durante el sueño.
ConclusionesLa MSIEP en niños y jóvenes es infrecuente, pero constituye una causa importante de mortalidad en epilépticos. Aunque los mecanismos de la MSIEP no son bien conocidos, se recomienda reforzar el control médico de la epilepsia en la juventud, principalmente en pacientes con epilepsia postraumática o post-quirúrgica o en aquellos con trastornos del desarrollo o retraso mental asociados.
Epilepsy is one of the most prevalent neurological diseases. Epilepsy patients, both children and adults, have a higher mortality rate than the general population. Deaths related to epilepsy can be due to different causes such as accidents, submergence, status epilepticus, or sudden unexplained death in epilepsy, the latter being one of the main causes of death due to the disease itself.1–5 In international terminology, this entity is known by the acronym “SUDEP”.
For the correct diagnosis of SUDEP, compliance with strict criteria is required, requiring a complete autopsy study that excludes any anatomical and toxicological cause of death. In forensic pathology, it has great significance due to its diagnostic difficulty and because it constitutes one of the main causes of sudden death (SD) in adolescents and young people.5
During the last 2 decades, multiple investigations have been carried out focused mainly on epidemiology and knowledge of the pathophysiological mechanisms of this entity and its risk factors. Although epilepsy is associated with a significantly increased risk of SD in children and adults, it is important to note that the absolute risk of SUDEP is low, and the majority of epileptic patients will not experience this complication.1,6–8 Guidelines from some scientific societies recommend that physicians report that the annual incidence of SUDEP is 0.2 per 1000 in children with epilepsy and 1.2 per 1000 per year in adults with epilepsy.8 However, the real incidence of SUDEP is uncertain and is probably underestimated since sometimes (due to lack of knowledge or due to its diagnostic difficulty), it is not adequately coded as the cause of death.
SUDEP occurs at all ages, although young adults between 20 and 40 years of age are at greatest risk.1,9,10 Some studies have shown that the risk of death in young patients with epilepsy is about 5 times higher than in the general population.9 The incidence in paediatric age is lower.8 In relation to sex, it seems that the incidence in men could be slightly increased.10
The main risk factor for SUDEP is the frequency of generalised tonic–clonic seizures. Other factors are refractoriness to treatment, not being seizure-free for years, lack of adequate pharmacological treatment, polytherapy, and early-onset and long-lasting epilepsy. In addition, certain neurological diseases (intellectual disability and structural brain abnormalities) and the use of alcohol or substances of abuse could increase the risk of SUDEP.1,8–12
Current research suggests that there is probably no single aetiology, but rather it is multifactorial and there are different mechanisms that may contribute to death in different patient populations or types of epilepsy. These mechanisms include cardiac arrhythmias, respiratory depression, dysregulation of cerebral circulation, and hormonal and metabolic changes induced during or after seizures.1–4,11,12 Likewise, there is increasingly strong evidence that there are genetic factors that may play an important role in SUDEP. Among them, the detection of several genes previously associated with long QT syndrome stands out.13
The objectives of this study were to analyse the demographic characteristics of global mortality due to epilepsy in children and young people; evaluate the impact of SUDEP in relation to both overall mortality due to epilepsy and total sudden deaths, and describe the clinical and toxicological characteristics of SUDEP in the forensic setting in children and young people. This approach aimed to provide more precise knowledge about the factors associated with these deaths, which could help develop preventive strategies to reduce their incidence.
Material and methodsDefinitionsSD is defined as one that occurs naturally, unexpectedly and in a time interval of less than 1 h from the beginning of the premonitory symptoms in a person with an apparent good state of health and who is carrying out their usual activities at the time of the fatal event. Also included are unwitnessed deaths, but in which the victim was seen alive and in good health in the 24 h prior to death.14
SUDEP is defined as sudden unexpected death in a patient diagnosed with epilepsy, in whose autopsy no anatomical or toxicological cause of death is discovered, excluding status epilepticus, traumatic death, and submersion.1,5
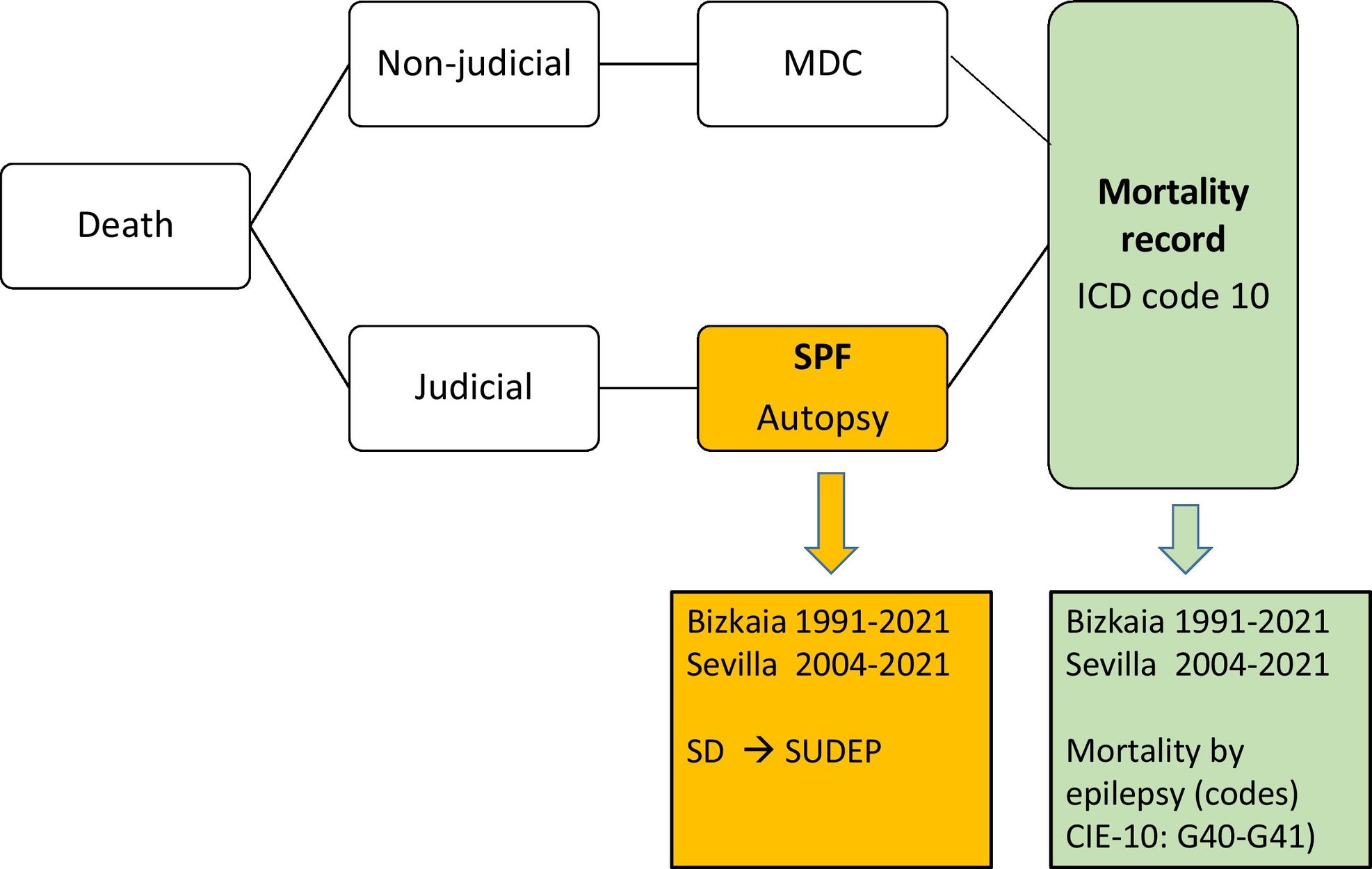
Legislation and procedure for coding causes of death in SpainAccording to Spanish legislation, a forensic autopsy is required for the investigation of violent and criminally suspected deaths, including SD. In the rest of natural deaths, the attending physician must complete the medical death certificate. Subsequently, all the causes of death that appear on the death certificates and in the forensic reports that occurred in a province are coded according to the ICD-10 in the mortality records and are transferred to the National Institute of Statistics (Fig. 1).
Study population and data collection sourcesRetrospective study of mortality due to epilepsy (ICD-10 codes: G40–G41) and SUDEP in people aged 1–35 years in the provinces of Bizkaia and Seville. In Bizkaia, the study period was from 1991 to 2021 (31 years) and in Seville from 2004 to 2021 (18 years).
In this study, 2 data sources were used: (a) mortality records from the Autonomous Community of the Basque Country and Seville; and (b) Forensic pathology services (SPF) of Bizkaia and Seville of the Institutes of Legal Medicine and Forensic Sciences (Fig. 1).
Mortality recordsThe deceased were selected from the mortality records (both from SPF autopsies and from medical death certificates) in the provinces of Bizkaia and Seville in which mortality due to epilepsy was listed as the cause of death (ICD-10 codes): G40–G41. Of these cases, the following variables were analysed: cause of death, age, and sex.
Forensic pathology services in Bizkaia and SevilleThe SPF files were analysed, identifying all cases of SD in people from 1 to 35 years old, and files were selected from these where the cause of death was SUDEP, according to the definition referred to above. The autopsy protocol includes clinical history, circumstances of death, examination of the place of death, and a complete autopsy with macroscopic and microscopic examination of all organs and toxicological analysis. Furthermore, except in people admitted to a hospital for more than 48 h, toxicological screening was requested in all autopsies.
Statistical analysisStatistical analysis was performed using SPSS for Windows version 21.0. Categorical variables were compared using the χ2 test and quantitative variables using non-parametric tests. The significance level chosen was P<.05.
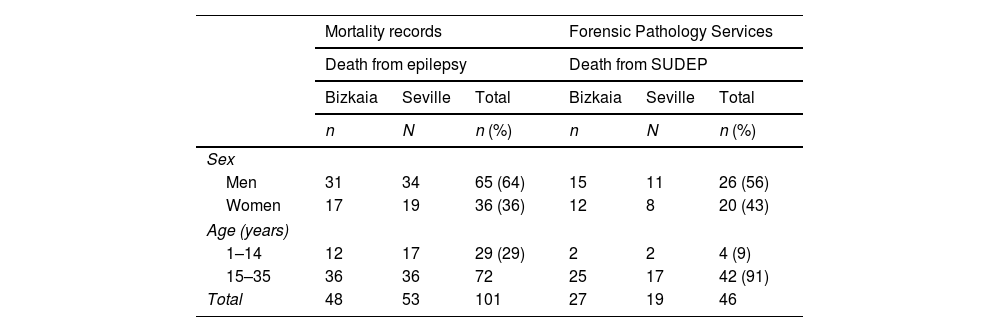
ResultsMagnitude of sudden unexplained death in epilepsy in relation to total mortality due to epilepsyAccording to the data from the mortality records (which include both the deceased in whom a forensic autopsy has been carried out and in which the medical death certificate has been issued) of Bizkaia and Seville, in the period analysed), 101 people were collected from 1 to 35 years old who died from epilepsy (ICD-10 codes: G40–G41). According to the SPF data, the number of SUDEPs was 46 (Table 1); that is, SUDEP represented 46% of the total deaths due to epilepsy. This percentage was 40% for men and 56% for women (P=.14). In relation to age, SUDEP represented only 14% of deaths due to epilepsy in paediatric age, while for young people, this percentage was 58% (P<.001).
Mortality data due to epilepsy and sudden death in epileptic patients (SUDEP).
| Mortality records | Forensic Pathology Services | |||||
|---|---|---|---|---|---|---|
| Death from epilepsy | Death from SUDEP | |||||
| Bizkaia | Seville | Total | Bizkaia | Seville | Total | |
| n | N | n (%) | n | N | n (%) | |
| Sex | ||||||
| Men | 31 | 34 | 65 (64) | 15 | 11 | 26 (56) |
| Women | 17 | 19 | 36 (36) | 12 | 8 | 20 (43) |
| Age (years) | ||||||
| 1–14 | 12 | 17 | 29 (29) | 2 | 2 | 4 (9) |
| 15–35 | 36 | 36 | 72 | 25 | 17 | 42 (91) |
| Total | 48 | 53 | 101 | 27 | 19 | 46 |
Data from the forensic pathology services of Bizkaia and Seville (forensic autopsy).
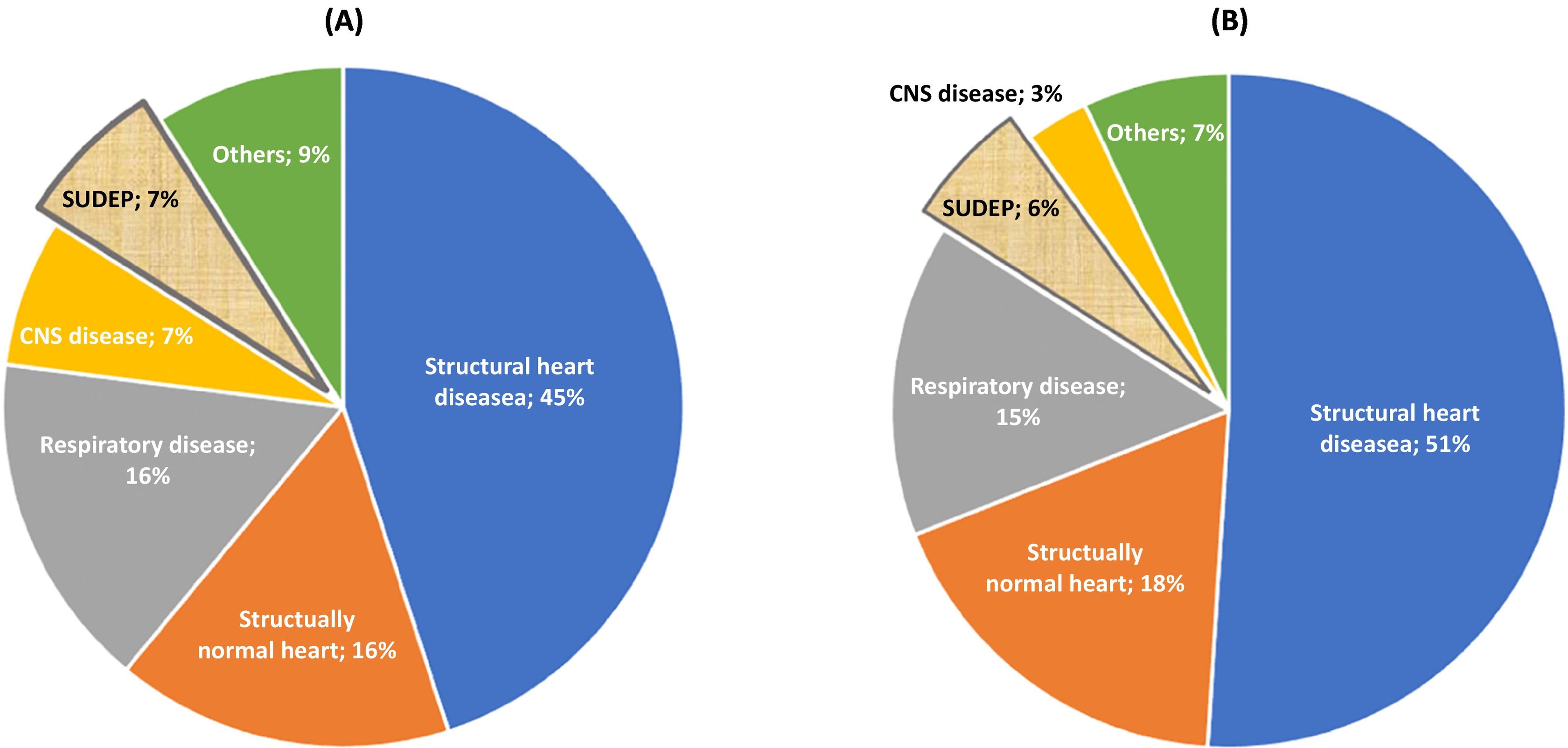
In the SPF of Bizkaia, 410 cases of SD were recorded in people between 1 and 35 years of age and in Seville, this figure was 339. The causes of SD in each province is represented in Fig. 2. The SUDEP (n=46) accounted for 6% of SD. The SUDEP percentage compared with the total of SD was slightly higher in women than in men (9% vs. 5%; P=.299). Regarding age, this percentage was slightly higher, but without any statistically significant differences, among young people (6%) than among children (5%).
Demographic and clinical data of sudden unexplained death in epilepsyOf the 46 SUDEP, 26 were men (56.5%). The median age was 27 years (25th percentile=21.75 and 75th percentile=29.25). The mean age was 25±6.7 years.
In relation to the history related to epilepsy, it should be noted that in 5 cases, the epilepsy was of post-traumatic origin, in 5, it was associated with brain anomalies (2 after surgery for aneurysm of the circle of Willis, 1 with lobectomy, another with a history of pituitary cyst, and another with a history of stroke). In addition, there were 7 subjects with relevant history related to developmental or similar disorders: autism (n=1), West syndrome (n=1), psychomotor delay (n=1), maturational delay (n=1); and 3 other cases of intellectual disability, one of them associated with a character disorder and another with pseudohypoparathyroidism. In total, 17 people (37%) had a history relevant to epilepsy.
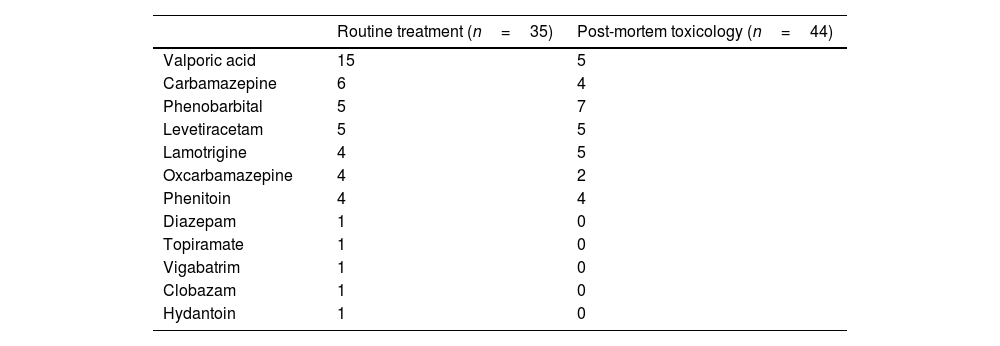
The pharmacological treatment prescribed against epilepsy, which was known in 35 people, is shown in Table 2. Eleven patients were being treated with more than one drug.
Routine treatment of patients with known medical history and post-mortem toxicology results in relation to antiepileptic drugs.
| Routine treatment (n=35) | Post-mortem toxicology (n=44) | |
|---|---|---|
| Valporic acid | 15 | 5 |
| Carbamazepine | 6 | 4 |
| Phenobarbital | 5 | 7 |
| Levetiracetam | 5 | 5 |
| Lamotrigine | 4 | 5 |
| Oxcarbamazepine | 4 | 2 |
| Phenitoin | 4 | 4 |
| Diazepam | 1 | 0 |
| Topiramate | 1 | 0 |
| Vigabatrim | 1 | 0 |
| Clobazam | 1 | 0 |
| Hydantoin | 1 | 0 |
The toxicological study was positive in 75% of the 44 cases in which it was carried out (2 young people died in the hospital of brain death after a recovered cardiorespiratory arrest), highlighting the presence of drugs indicated for epilepsy in 26 cases (Table 2). Other types of drugs were detected in another 4 subjects. The presence of illegal drugs was positive in 5 young people: cocaine (n=3) and/or cannabis (n=3). There were no cases with a blood alcohol level greater than 0.5 g/l.
Circumstances of deathDeath was unwitnessed in the majority of subjects (85%) and in cases where it was witnessed, it was preceded by a seizure. 63% of the events occurred at night, with the bed being the most frequent place of death (61% among those for whom this information was known).
DiscussionSUDEP is the main cause of premature mortality related to epilepsy, especially in the young population.1,9,10 The percentage of SUDEP in relation to total mortality due to epilepsy is around 10%–30%.3,6,7 This percentage is higher in younger epileptics, as observed in our study, with a percentage of 46%. However, these data must be evaluated with caution since the figures vary depending on the population analysed, the study design, the type of epileptic patients included, age, the criteria used to define and diagnose SUDEP cases, and the cause of death coding system.
However, it should not be forgotten that, in absolute terms, the incidence of SUDEP in the general population is very low, mainly in paediatric age. The findings of the present study that analysed the frequency of SUDEP in 2 provinces are in line with these observations since in Bizkaia (population of approximately 1 million inhabitants analysed over 31 years) and in Seville (population of almost 2 million inhabitants analysed for 18 years), only 46 cases were recorded.
Our study shows that the impact of SUDEP in relation to total mortality from epilepsy is higher in young people than in children (58% vs. 14%; P<.001). In paediatric age, mortality due to epilepsy mainly affects high-risk patients with significant neurological damage or injury.11 In our context, it is expected that the deaths of these epileptic children with severe neurological disease will not be the subject of a forensic study, but rather that their paediatrician will issue the medical death certificate. This fact would explain, in part, these differences detected between children and young people. Another factor involved in explaining the greater impact of SUDEP on young people than on children is that the person goes from a protected and supervised family environment to an environment of relative independence, which results in poor compliance with medical prescriptions.1–4,10,11
In the main series of SD in children and young people, including the present one, the frequency of SUDEP ranged between 6% and 15%, constituting one of the main causes.15,16.
According to some studies, the frequency of SUDEP seems to be more prevalent in men than in women,10,17 although the reasons for this are not well understood. The percentage observed in our work (56.5%) is similar to that observed in a recent bibliographic review of 385 cases of which 59% were men.10
In the medical literature, a higher incidence of SUDEP has been described in patients with epilepsy secondary to structural brain anomalies or with associated neurological disability compared to patients with idiopathic epilepsy and also in those with more severe or refractory epilepsy.3,18–20 In line with this, our work highlights the high frequency of cases (37%) with relevant antecedents such as post-traumatic epilepsy (n=5), other structural brain anomalies (n=5) and patients with epilepsy associated with developmental disorders or intellectual disability (n=7).
The lack of adequate pharmacological treatment is another risk factor for SUDEP.17,21 In post-mortem toxicological analysis, the most common factor is either not to detect drugs or to find anticonvulsant drugs in the blood at subtherapeutic levels. In this study, no antiepileptic drugs were detected in the post-mortem analysis in 41%, which would suggest the hypothesis that compliance with the pharmacological prescription is poor in these patients.
Alcohol and psychostimulating drug consumption could lower the seizure triggering threshold and be a risk factor for SUDEP.22,23 This may be secondary to the toxic effects of the substance or due to an indirect mechanism by contributing to poorer adherence to pharmacological treatment or by modifying sleep habits. In a series from the United States of 1086 cases of SUDEP,21 the percentage of illegal drugs was lower than ours (5% vs. 11%) but alcohol was detected in up to 13%, while in ours, it was not detected in any cases. This data is relevant for SUDEP prevention strategies. Thus, among the preventive measures recommended is to avoid possible triggers of SUDEP such as excessive consumption of alcohol and illegal drugs.
Regarding circumstantial data, SUDEP episodes occur during the night, which appears to be due to different factors, including the lack of monitoring by caregivers and physiological changes related to the circadian rhythm.24,25 In the study by Lamberts et al.,24 it was observed that 62% of the 154 cases of SUDEP occurred between midnight and noon, and that 58% of the SUDEP cases were related to sleep. The results of this work are very similar with percentages of 63% and 61%, respectively. In view of these circumstantial findings, it has been suggested that routine measures taken during a crisis may confer protection against MS.26–28
LimitationsThe main limitations of the present study are, on the one hand, its retrospective nature, which has made it difficult to exhaustively collect clinical risk factors; and, on the other hand, being a relatively small series. Other limitations are that a genetic analysis or molecular autopsy was not performed and that the neuropathological study did not meet the standards currently recommended by international guidelines for SUDEP research.29 However, we consider that our results can help to better understand the factors involved in this type of death.
Future implicationsForensic pathology is a relevant source of data for public health prevention strategies. To improve the knowledge generated in our forensic field at SUDEP, it would be necessary to develop multicentre forensic studies, the creation of a prospective investigation with a systematised registry that guarantees an adequate collection of all risk factors, the performance of neuropathological studies in accordance with the standards set by experts and the inclusion of genetic studies in post-mortem research, for which the conservation of frozen blood with EDTA is recommended. Finally, and in light of the advances in genetic studies in SUDEP, it is suggested that first-degree relatives be referred to a cardiology service equipped with a family heart disease unit to offer them a correct clinical evaluation.
ConclusionsThe pathophysiological mechanisms that trigger SUDEP remain unknown, and research on this entity therefore needs to be enhanced in order to detect risk factors that help in prevention. However, certain preventive strategies appear to be potentially useful. Based on our findings, adequate night-time supervision, correct adherence to pharmacological treatment and avoiding the use of psychostimulant drugs can be effective measures to reduce the incidence, mainly in young people. Although these measures should be universal for all epileptics, they should be especially promoted in those who suffer from post-traumatic or post-surgical epilepsy or in those who have associated developmental disorders or intellectual disability.
FundingNone.
Declaration of competing interestThe authors have no conflicts of interest to declare.
AcknowledgementsOur thanks to the members of the Forensic Pathology Service of Bilbao and Seville for their cooperation with the study and to Covadonga Audicana and Pedro Olano for their collaboration with the mortality registry data.
PublicationsThe work described herein was previously published within the framework of Klaudia I. Bidaurrazaga's final degree project.
Please cite this article as: Bidaurrazaga KI, Lucena J, Morentin B. Forensic population study of sudden unexplained death in epilepsy in children and young people during the period 1991–2021. Revista Española de Medicina Legal. 2023. https://doi.org/10.1016/j.reml.2023.08.003.