Suicide remains one of the leading causes of death worldwide. Due to the relationship between suicidal behaviour and mental disorder, our aim is to determine the number of people who received care by the Mental Health Network among the total number of suicides consummated between 2017 and 2022 in Gran Canaria, as well as the characteristics of that population and the care received.
Material and methodsLongitudinal observational retrospective study in which the study population was extracted from the total number of suicides in the database of the Legal Medicine Institute. Subsequently, the data were cross-checked by the Mental Health Network databases. Finally, a univariate statistical analysis was carried out and the results were compared according to sex and care in the Community Mental Health Unit.
ResultsOnly 39.4% had received care at the Mental Health Unit, the majority being women (55.3% vs. 34.6%), with a mean age of 50.9 years for both sexes. History of previous attempts was much more frequent in the population receiving care (45.4% vs. 7%), as well as emergency care (42% vs. 5.7%) and hospital admissions (25.3% vs. 0.7%).
ConclusionLess than half of the deceased persons had contact with a Community Mental Health Unit. In addition, care by this unit was higher among those with previous attempts and among the female sex, with the most frequent diagnosis being monopolar affective disorders.
El suicidio sigue siendo una de las principales causas de muerte en todo el mundo. Debido a la relación entre conducta suicida y trastorno mental, nuestro objetivo es determinar el número de personas que recibían atención por la Red de Salud Mental entre el total de suicidios consumados entre 2017 y 2022 en Gran Canaria, así como las características de dicha población y de la atención recibida.
Material y métodosEstudio longitudinal observacional retrospectivo en el que la población de estudio fue extraída del total de suicidios de la base de datos del Instituto de Medicina Legal. Posteriormente, los datos fueron cotejados por las bases de datos de la Red de Salud Mental. Por último, se realizó un análisis estadístico univariante y los resultados fueron comparados en función del sexo y la atención en la Unidad de Salud Mental Comunitaria.
ResultadosSolo un 39,4% había recibido atención por parte de la Unidad de Salud Mental, siendo la mayoría mujeres (55.3% vs. 34.6%), con una media de edad de 50,9 años para ambos sexos. Los antecedentes de intentos previos fueron mucho más frecuentes en la población que recibía atención (45,4% vs. 7%), así como la atención en urgencias (42% vs. 5,7%) y los ingresos hospitalarios (25,3% vs. 0,7%).
ConclusiónMenos de la mitad de las personas fallecidas tuvieron contacto con una Unidad de Salud Mental Comunitaria. Además, la atención por esta es mayor entre aquellas personas con intentos previos y entre el sexo femenino, siendo el diagnóstico más frecuente el de los trastornos afectivos monopolares.
Suicide, understood as “self-inflicted death with implicit or explicit evidence that the person intended to kill themself”,1 continues to represent a serious problem for society and a challenge for health professionals. Focusing on Spain, the most recent data is from 2021, where according to the INE, a total of 4003 suicides occurred. This represents an average of 11 suicides daily, constituting the first cause of unnatural death in Spain.2,3 It also represents a suicide mortality rate of 8.45 people per 100 000 inhabitants on average in Spain in 2021, which in the Canary Islands increases to a rate of 9.56 people per 100 000 inhabitants in 2020 (the 2021 data are not yet available).2–4
One of the main risk factors is previous suicide attempts; in fact, the WHO estimates that for every suicide, 20 suicide attempts are committed.5 Furthermore, in 2019, 77% of suicides were committed in low- and middle-income countries,6 which suggests an important role of socioeconomic aspects in this type of behaviour. Other factors to highlight are sex, since the so-called “paradox of sex” states that women make more attempts, but that men die more by suicide,5–8 and age, observing that adolescents and young adults die more by suicide. However, age-standardised suicide rates are higher at older ages.2,3,6,7
The presence of a mental disorder is one of the most significant risk factors, increasing the risk of suicide up to 10 times compared to the general population.7 In fact, there are studies that show that in high-income countries, 90% of people who die by suicide suffered from some type of mental illness, while psychiatric symptoms could be found in the undiagnosed 10%.6 The mental disorders most frequently associated with suicide are depressive disorders, personality disorders (especially borderline personality disorder), and alcohol abuse disorders.6,9-11 Furthermore, alcohol is present in up to 50% of suicidal deaths, with 22% of suicides being attributed to alcohol abuse exclusively and this risk being even greater, especially when related to adjustment disorders and depression.6,7,9 Also, certain studies show that the association between alcohol consumption and suicidal behaviour is greater in women than in men.12 On the other hand, it is estimated that the risk of suicide in people who suffer from pain or chronic diseases is 2–3 times higher than that of the general population.6,13 In patients with cancer, the risk is higher, especially in the first 6 months after diagnosis.14 Likewise, a family history of suicidal death increases the risk of suicidal behaviour and mental disorder,6 with family history being much more common among individuals with multiple suicide attempts.15
Regarding the methods used in suicidal deaths, there are numerous methods and these vary depending on the country and/or whether we are in a rural or urban area.7 If we focus on Spain, in 2020, the most used methods globally were (in order of frequency): hanging, jumping from height, and poisoning from drugs.16 Focusing on the differences by sex, the most used method in men was hanging (49.9%), while in women, it was jumping from height (37.5%).16
Finally, it is essential to determine the role played by the care received from health services in these patients and the effect that this can have on suicidal behaviour, forming the cornerstone of this study. Various studies show that the immediate period after discharge of a patient, especially in those hospitalised for suicidal ideation or behaviour, represents an increase in suicidal risk.17–19 Furthermore, the risk at 1 year is much higher in patients who present some type of mental disorder, the most common diseases being depressive disorder, bipolar disorder, substance abuse, and schizophrenia.17–19 Therefore, the purpose of this study is to know the number of people who received care from the Mental Health Network of Gran Canaria among the total number of suicides in the last 6 years, as well as to determine the characteristics of the care they received and obtain a descriptive profile of people who commit suicide in Gran Canaria. The Mental Health Network of Gran Canaria contemplated in this study is mainly composed of the Community Mental Health Units (USMC for its initials in Spanish) (made up of multidisciplinary teams with doctors, psychologists, nurses, assistants, and social workers) and hospital care in the Doctor Negrín Hospital Psychiatric Service and the Insular Maternal-Child Hospital (reserved for admissions to short-stay, intermediate-stay, and long-stay units).
Material and methodsDesignA retrospective, observational, longitudinal study was conducted which included people who died by suicide on the island of Gran Canaria between the years 2017 and 2022 (both included), obtaining the information through the autopsy reports of the Institute of Legal Medicine of Las Palmas de Gran Canaria notified as “violent death of suicidal aetiology.” Then, the data obtained were collated by the database of mental health patients of the Canarian Health Service at the hospital and outpatient level, without considering primary care.
An initial sample of 551 people was obtained, with the number of suicides per year being: 105 in 2017, 103 in 2018, 122 in 2019, 80 in 2020, 85 in 2021, and 56 in 2022. From this sample, those people whose affiliation data could not be obtained (33 cases) and those for whom information on the variables to be studied was not obtained (25 cases) were excluded. This left us with a final sample of 493 people.
Regarding current regulations on data protection and patient privacy, compliance was ensured in this study since all data was collected individually in the corresponding centres, maintaining at all times the anonymity and confidentiality of the autopsy reports and medical records reviewed. Also, since this was a retrospective study, and since the data obtained would not affect their clinical management, given that the entire sample was based on deceased people, patient anonymity was maintained and it was not necessary to complete an informed consent. Furthermore, the study was evaluated and approved by the Research Ethics Committee of the Doctor Negrín University Hospital of Gran Canaria.
Study variablesThe variables collected for the study may be divided into:
- •
Sociodemographic variables:
- o
Sex: man/woman.
- o
Age: mean and age subgroups: 15–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years, and ≥75 years.
- •
Variables relating to environmental factors: season of the year in which the suicide took place (Spring, Summer, Autumn, and Winter).
- •
Variables relating to risk factors:
- o
Medical history: chronic pain, chronic infection (HIV, HCV), degenerative diseases (dementias, Parkinson's disease, Huntington's chorea, CADASIL, amiotrophic lateral sclerosis, and cancer (active or in remission)).
- o
Number of previous suicide attempts: none, 1, 2 or more, unknown.
- •
Variables related with suicide itself:
- o
Mechanism of suicide: handing, drowning, jump tin from height, self-inflicted poisoning (from drugs or not), firearms, knife, self-inflicted asphyxiation, explosion.
- o
Type of toxic substances at autopsy: alcohol, cocaine, benzodiazepines, antidepressants, opiates, analgesics, amphetamines, cannabinoids, non-steroidal anti-inflammatory drugs (NSAIDs), ethylene glycol, antipsychotics, beta blockers, methadone, mood stabilisers, and carbon monoxide.
• Variables related to care at the USMC:
- o
Number of contacts.
- o
Diagnosis: no diagnosis, monopolar affective disorders, bipolar disorder, schizophrenia, other specific personality disorders, borderline personality disorder (BPD), substance abuse disorders, anxiety disorders, other diagnoses (conversion disorders, adjustment disorders, or obsessive-compulsive disorder).
- o
Type of pharmacological treatment: antipsychotics, mood stabilisers, benzodiazepines, selective serotonin reuptake inhibitors (SSRIs), other antidepressants, hypnotics, analgesics, tiapride, nalmefene, acamprosate, methadone, disulfiram, methylphenidate, biperiden.
- o
Professional who carried out the follow-up: psychiatrist, clinical psychologist, nurse, nursing assistant, social worker.
• Variables related to hospitalisation:
- o
Number of hospitalizations: none, 1, 2 or more.
- o
Diagnoses: non-diagnostic, monopolar affective disorders, bipolar disorder, schizophrenia, other specific personality disorders, borderline personality disorder, substance abuse disorders, anxiety disorders, other diagnoses (conversion disorders, adjustment disorders, or obsessive compulsive).
- o
Time elapsed from hospital discharge to death (months).
• Variables related to care in psychiatric emergencies:
- o
Attention (yes/no).
- o
Diagnoses: behavioural disorders, suicidal attempt, suicidal ideation, anxiety disorders, substance abuse disorders, depressive episode, other diagnoses.
- o
Time elapsed from discharge from the emergency room to death (months).
A univariate analysis was performed. Categorical variables are expressed as frequencies and percentages and continuous variables as mean and standard deviation (SD) when the data followed a normal distribution, or as median and interquartile range (IQR=25th–75th percentile) when the distribution deviated from normality. Percentages were compared, as appropriate, using the Chi square test (×2) or Fisher's exact test; means using the t test, and medians using the Wilcoxon test for independent data. In the case of binary factors associated with the outcome, the corresponding odds-ratio was estimated using a 95% confidence interval. Statistical significance was set at P<.05. The data were analysed with the R package, version 4.2.1 (R Development Core Team, 2022).20
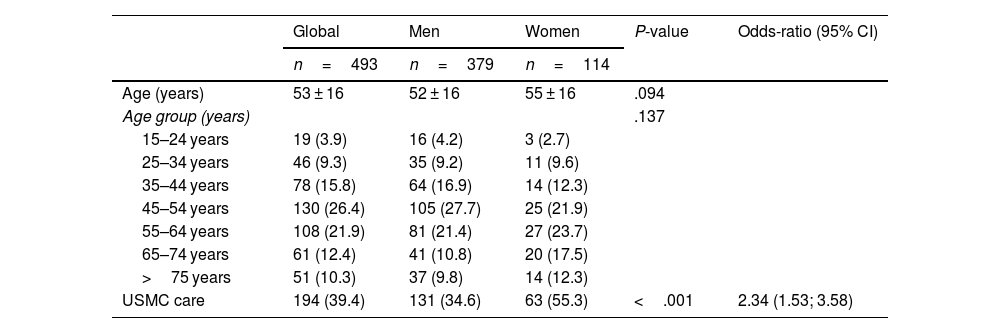
ResultsStudy population characteristicsThe study population characteristics according to sex are contained in Table 1.
Study population characteristics according to sex.
| Global | Men | Women | P-value | Odds-ratio (95% CI) | |
|---|---|---|---|---|---|
| n=493 | n=379 | n=114 | |||
| Age (years) | 53 ± 16 | 52 ± 16 | 55 ± 16 | .094 | |
| Age group (years) | .137 | ||||
| 15–24 years | 19 (3.9) | 16 (4.2) | 3 (2.7) | ||
| 25–34 years | 46 (9.3) | 35 (9.2) | 11 (9.6) | ||
| 35–44 years | 78 (15.8) | 64 (16.9) | 14 (12.3) | ||
| 45–54 years | 130 (26.4) | 105 (27.7) | 25 (21.9) | ||
| 55–64 years | 108 (21.9) | 81 (21.4) | 27 (23.7) | ||
| 65–74 years | 61 (12.4) | 41 (10.8) | 20 (17.5) | ||
| >75 years | 51 (10.3) | 37 (9.8) | 14 (12.3) | ||
| USMC care | 194 (39.4) | 131 (34.6) | 63 (55.3) | <.001 | 2.34 (1.53; 3.58) |
Data are: mean±SD frequencies (%) and medians (IQR).
USMC: Community Mental Health Unit.
Of the total number of people who died by suicide included in the study, the majority were men (76.9%) with an average age for both sexes of 53 years. Of the total, only 39.4% received care from the USMC, the majority being women (55.3% vs. 34.6%, P<.001).
Risk factors and suicidal behaviourThe most used mechanisms, in order of frequency, were been hanging (48.9%), jumping from height (31%), and intoxication (medicated or not) (11.6%) (P<.001). However, if we stratify by sex, the methods most used in men are hanging (55.1%) and jumping from height (26.6%); while for women, the most used method is precipitation (45.6%), followed by hanging (28.1%) and poisoning (20.2%).
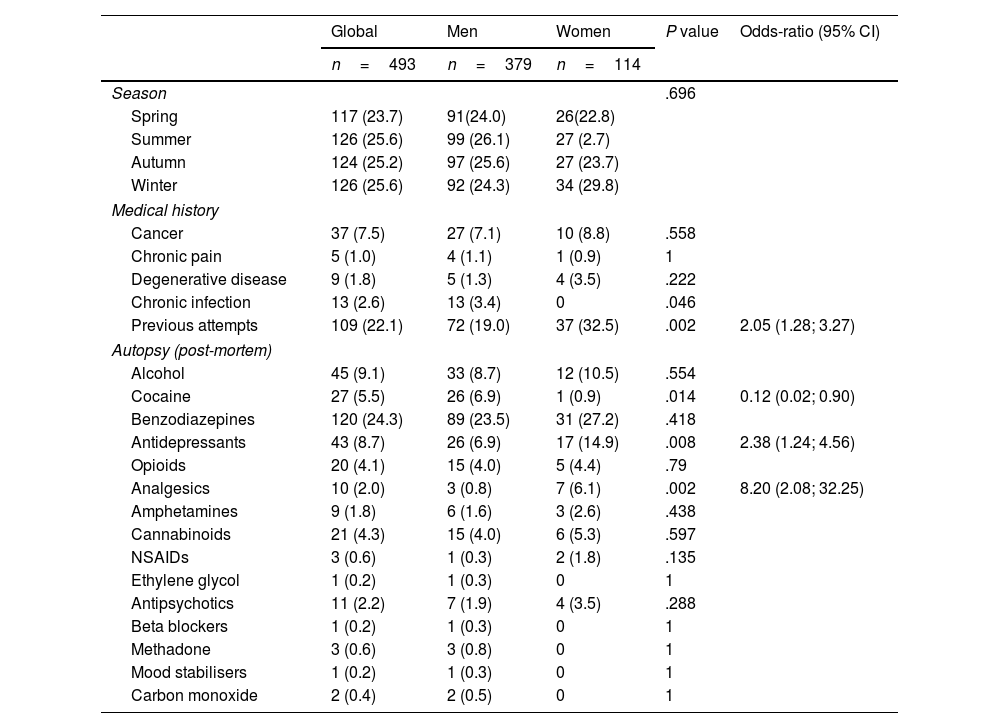
The environmental factors and risk factors according to sex are shown in Table 2.
Environmental and risk factors according to sex.
| Global | Men | Women | P value | Odds-ratio (95% CI) | |
|---|---|---|---|---|---|
| n=493 | n=379 | n=114 | |||
| Season | .696 | ||||
| Spring | 117 (23.7) | 91(24.0) | 26(22.8) | ||
| Summer | 126 (25.6) | 99 (26.1) | 27 (2.7) | ||
| Autumn | 124 (25.2) | 97 (25.6) | 27 (23.7) | ||
| Winter | 126 (25.6) | 92 (24.3) | 34 (29.8) | ||
| Medical history | |||||
| Cancer | 37 (7.5) | 27 (7.1) | 10 (8.8) | .558 | |
| Chronic pain | 5 (1.0) | 4 (1.1) | 1 (0.9) | 1 | |
| Degenerative disease | 9 (1.8) | 5 (1.3) | 4 (3.5) | .222 | |
| Chronic infection | 13 (2.6) | 13 (3.4) | 0 | .046 | |
| Previous attempts | 109 (22.1) | 72 (19.0) | 37 (32.5) | .002 | 2.05 (1.28; 3.27) |
| Autopsy (post-mortem) | |||||
| Alcohol | 45 (9.1) | 33 (8.7) | 12 (10.5) | .554 | |
| Cocaine | 27 (5.5) | 26 (6.9) | 1 (0.9) | .014 | 0.12 (0.02; 0.90) |
| Benzodiazepines | 120 (24.3) | 89 (23.5) | 31 (27.2) | .418 | |
| Antidepressants | 43 (8.7) | 26 (6.9) | 17 (14.9) | .008 | 2.38 (1.24; 4.56) |
| Opioids | 20 (4.1) | 15 (4.0) | 5 (4.4) | .79 | |
| Analgesics | 10 (2.0) | 3 (0.8) | 7 (6.1) | .002 | 8.20 (2.08; 32.25) |
| Amphetamines | 9 (1.8) | 6 (1.6) | 3 (2.6) | .438 | |
| Cannabinoids | 21 (4.3) | 15 (4.0) | 6 (5.3) | .597 | |
| NSAIDs | 3 (0.6) | 1 (0.3) | 2 (1.8) | .135 | |
| Ethylene glycol | 1 (0.2) | 1 (0.3) | 0 | 1 | |
| Antipsychotics | 11 (2.2) | 7 (1.9) | 4 (3.5) | .288 | |
| Beta blockers | 1 (0.2) | 1 (0.3) | 0 | 1 | |
| Methadone | 3 (0.6) | 3 (0.8) | 0 | 1 | |
| Mood stabilisers | 1 (0.2) | 1 (0.3) | 0 | 1 | |
| Carbon monoxide | 2 (0.4) | 2 (0.5) | 0 | 1 | |
Data are: means±SD, frequencies (%), and medians (IQR).
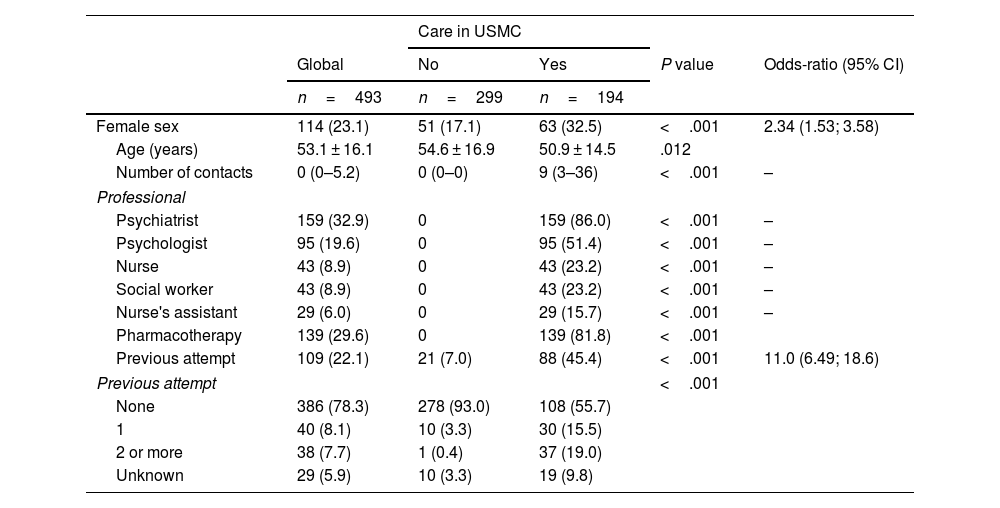
The population characteristics and care received in the USMC are detailed in Table 3.
Population characteristics and care received according to the USMC.
| Care in USMC | |||||
|---|---|---|---|---|---|
| Global | No | Yes | P value | Odds-ratio (95% CI) | |
| n=493 | n=299 | n=194 | |||
| Female sex | 114 (23.1) | 51 (17.1) | 63 (32.5) | <.001 | 2.34 (1.53; 3.58) |
| Age (years) | 53.1 ± 16.1 | 54.6 ± 16.9 | 50.9 ± 14.5 | .012 | |
| Number of contacts | 0 (0–5.2) | 0 (0–0) | 9 (3–36) | <.001 | – |
| Professional | |||||
| Psychiatrist | 159 (32.9) | 0 | 159 (86.0) | <.001 | – |
| Psychologist | 95 (19.6) | 0 | 95 (51.4) | <.001 | – |
| Nurse | 43 (8.9) | 0 | 43 (23.2) | <.001 | – |
| Social worker | 43 (8.9) | 0 | 43 (23.2) | <.001 | – |
| Nurse's assistant | 29 (6.0) | 0 | 29 (15.7) | <.001 | – |
| Pharmacotherapy | 139 (29.6) | 0 | 139 (81.8) | <.001 | |
| Previous attempt | 109 (22.1) | 21 (7.0) | 88 (45.4) | <.001 | 11.0 (6.49; 18.6) |
| Previous attempt | <.001 | ||||
| None | 386 (78.3) | 278 (93.0) | 108 (55.7) | ||
| 1 | 40 (8.1) | 10 (3.3) | 30 (15.5) | ||
| 2 or more | 38 (7.7) | 1 (0.4) | 37 (19.0) | ||
| Unknown | 29 (5.9) | 10 (3.3) | 19 (9.8) | ||
Data are means ± SD, frequencies (%) and medians (IQR).
USMC: Community Mental Health Unit.
The most frequent diagnoses among patients who died by suicide are, in order of frequency: monopolar affective disorders (23.1%), other specific personality disorders (11.0%), anxiety disorders (8.8%), schizophrenia (8.8%), substance use disorders (6.6%), bipolar disorder (3.8%), and borderline personality disorder (2.2%). In 8.8% of the cases, no diagnosis was established and 26.9% fell within the group of “other diagnoses” which includes less frequent diseases such as conversion disorders, adaptive disorders, or obsessive-compulsive disorder.
On the other hand, 81.8% of the patients treated by the USMC received pharmacological treatment (P<.001). The most commonly used drugs were benzodiazepines (57.6%, P<.001), antipsychotics (40.8%; P<.001), SSRIs (35.9%; P<.001), antidepressants other than SSRIs (29.4%; P<.001), hypnotics (10.3%; P<.001), and mood stabilisers (6.0%; P<.001).
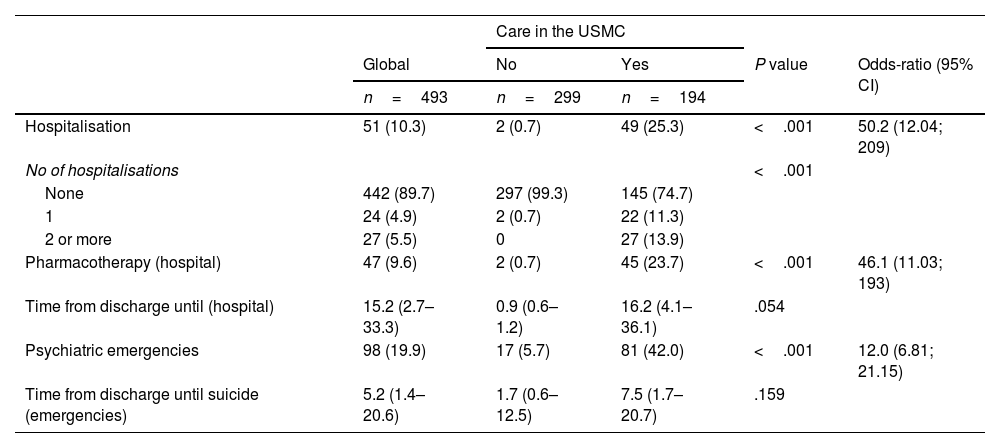
Hospitalisation and psychiatric emergenciesThe results on hospitalisation and care in psychiatric emergencies according to care in the USMC are shown in Table 4.
Hospitalisation and care in psychiatric emergencies according to care in the USMC.
| Care in the USMC | |||||
|---|---|---|---|---|---|
| Global | No | Yes | P value | Odds-ratio (95% CI) | |
| n=493 | n=299 | n=194 | |||
| Hospitalisation | 51 (10.3) | 2 (0.7) | 49 (25.3) | <.001 | 50.2 (12.04; 209) |
| No of hospitalisations | <.001 | ||||
| None | 442 (89.7) | 297 (99.3) | 145 (74.7) | ||
| 1 | 24 (4.9) | 2 (0.7) | 22 (11.3) | ||
| 2 or more | 27 (5.5) | 0 | 27 (13.9) | ||
| Pharmacotherapy (hospital) | 47 (9.6) | 2 (0.7) | 45 (23.7) | <.001 | 46.1 (11.03; 193) |
| Time from discharge until (hospital) | 15.2 (2.7–33.3) | 0.9 (0.6–1.2) | 16.2 (4.1–36.1) | .054 | |
| Psychiatric emergencies | 98 (19.9) | 17 (5.7) | 81 (42.0) | <.001 | 12.0 (6.81; 21.15) |
| Time from discharge until suicide (emergencies) | 5.2 (1.4–20.6) | 1.7 (0.6–12.5) | 7.5 (1.7–20.7) | .159 | |
The data are: means ± SD, frequencies (%), and medians (IQR).
USMC: Community Mental Health Unit.
Of the total study population, 10.3% had been hospitalised in the psychiatry service, with the most frequent hospital diagnoses among patients cared for by the USMC being: schizophrenia (4.7%), monopolar affective disorders (3.6%), and substance abuse disorders (3.6%).
Regarding care in psychiatric emergencies, 19.9% of the total sample was treated in this service. The most frequent diagnoses in this type of care were: suicide attempt (15.6%), suicidal ideation (7.3%), behavioural alteration (4.2%), anxiety disorders (3.6%), and substance use disorders (2.6%).
DiscussionOverall descriptionThe sociodemographic characteristics of the people who died by suicide on the island of Gran Canaria in the indicated period of time coincide, in general, with the data obtained at the national and international level. Most of the suicides were carried out by men.2,5–7 However, the average age differs from that described internationally, where the rate of death by suicide is higher in groups over 70 years old or in those younger than 34,5–7 in our case, 53.1 years for both sexes (age group between 45 and 54 years), and coinciding with other studies at the national level.2,6 Despite the increase in suicide figures both nationally and internationally,2,3,5 on the island of Gran Canaria, a decrease in suicidal deaths has been observed in the last 3 years, which could demonstrate the effectiveness of the Mental Health Plan of the Canary Islands approved in 2019, with a specific strategy plan dedicated to suicide prevention.
Regarding the most frequently used mechanisms, at a general level they are similar to the existing statistics, with the most common global method being hanging, and by sex, hanging in men and jumping from height in women.3,6,7,16
Regarding toxins, these were found in 72.2% of the deceased; There are studies that show a large proportion of subjects who had consumed some type of toxic substance before death,21, constituting an important risk factor for suicidal behaviour.6,12,21
Furthermore, 22.1% had a history of previous suicide attempts, this percentage being higher within the female population, which is confirmed in other series where women have a greater tendency towards both suicidal ideation and attempts.2,6–8
Care in the community mental health unitAbout 39.4% of the sample had received care from the USMC at some point in their lives. According to international studies, people who die by suicide are more frequently seen in primary care than by USMC.22 However, those people with a diagnosed psychiatric disorder tend to make multiple suicide attempts,16 which coincides with our results, given that among the population receiving care from the USMC the percentage of previous attempts was notably higher (45.4% vs. 7%, P<.001).
Psychiatric disorders among people who commit suicide are much more common than in the general population.10,21 The most frequent psychiatric diagnoses in our sample coincide with those of other studies, where major depressive disorder is the most frequent risk factor among the population that dies by suicide.7,23 This is because the risk is up to 20 times higher in people who suffer from depression.23
Pharmacological treatmentOf the patients monitored by the USMC, 81.8% received pharmacological treatment. Benzodiazepines were the most prescribed drug (57.6%), and there are currently several studies that attempt to clarify whether or not there is an association between the use of benzodiazepines in patients with psychiatric disorders and an increased risk of suicide, with an increase found in some of them.24 However, this association could be due to a greater prescription of benzodiazepines in those patients who already have a high suicidal risk per se, an increase in impulsivity or a withdrawal syndrome caused by this drug.24 Furthermore, in our study, benzodiazepines were the substance most frequently found in the toxicological analysis of the autopsy, surpassing alcohol (24.3% vs. 9.1%, respectively), which could also show this association since benzodiazepines can cause poisoning and death due to overdose.24 However, deaths caused solely by overdoses of benzodiazepines are rare, and their presence with other substances, especially SSRIs and alcohol, is common.21
Hospital care and psychiatric emergenciesThe majority of hospital admissions (in short-stay units) occurred among the population that previously received care from the USMC (23.7% vs. 0.7%, P<.001). 11.3% were hospitalised only once, while 13.9% were hospitalised 2 or more times, which coincides with what has been described in the literature to date, given that those patients with a single hospitalisation have a lower risk of suicide than those who re-enter, which may constitute an important risk factor.25 The average time elapsed between the discharge date of the last hospital admission and death is 15.2 months (2.7–33.3 months), which does not coincide with other studies in which the highest risk of suicide occurs in the first 3 months after discharge.17,18
On the other hand, the risk of suicide after hospital discharge was higher in those patients diagnosed with schizophrenia (4.7%), monopolar affective disorder (3.6%), and substance abuse (3.6%), which is consistent with literature.17,18
Regarding psychiatric emergency care, it is important to highlight that the majority of suicide attempts treated in the emergency department came from the sample followed by the USMC (15.6% vs. 2.7%, P<.001). This can be explained because those patients treated by the USMC are those who, for the most part, already have a history of suicide attempts, being prone to retrying and going to the emergency department more frequently. However, the average time elapsed between the date of discharge from the last emergency care and death is 5.2 months (1.4–20.6 months), which represents a longer period than the findings of other studies, where the highest risk of suicide is estimated during the first 30 days after discharge from the emergency department.26 Furthermore, this time is reduced to 1.7 months in those without follow-up by the USMC, which suggests the importance of adequate care and treatment by mental health specialists in the prevention of suicidal behaviour.
Study limitationsThe main limitation is that all the data were obtained only from the peoples' autopsy reports and medical records. Furthermore, since this was a retrospective observational longitudinal study, we were unable to study adherence to pharmacological treatment. Another limitation is the impossibility of recovering all suicide deaths in the indicated time interval due to the difficulty in certifying some deaths. Related to the number of deaths, we also observed that our statistics reflect a different number of suicidal deaths on the island for the indicated period of time compared to other official sources such as the Canary Islands Institute of Statistics (ISTAC for its initials in Spanish). These variations are due to the fact that ISTAC collects suicides of residents in Gran Canaria, carried out both on the island and on any other island/province whilst from the Institute of Legal Medicine and Forensic Sciences, we obtained suicidal deaths that occurred in Gran Canaria, whether the deceased was a resident or not.
Furthermore, it was not possible to evaluate follow-up in primary care either, this being one of the most relevant limitations, given that it would be essential for future studies. Finally, this study is merely descriptive given that there is no comparable control group of patients who did not commit suicide, so an association between the different variables cannot be established.
ConclusionLess than half of the people who died by suicide received care from the USMC, with follow-up being more frequent in women. The most common suicide profile is, however, that of a man between 45 and 54 years old, with hanging being the most common suicide mechanism. If we focus on the follow-up by the USMC, the most frequent diagnosis among patients was monopolar affective disorders. All of this highlights the need to establish prevention measures at a primary and specialised level, improving follow-up strategies in patients who present with risk factors.
Please cite this article as: Löpez de Lamela Suárez M, Rivero Hernández SM, Hernández Fleta JL, Saavedra Santana P, Zaragoza Pérez E. Suicidio consumado en Gran Canaria en el periodo 2017-2022 y su relación con antecedentes de trastorno mental. Revista Española de Medicina Legal. 2023. https://doi.org/10.1016/j.reml.2023.08.002.