Thoracic aortic dissection/rupture has a high mortality, constituting 3.9%–5.4% of sudden deaths (SD) in forensic series. Medial histopathological findings associated with these entities have received multiple terms and definitions. In 2016, the European Association for Cardiovascular Pathology and the Society for Cardiovascular Pathology published a consensus document, applied to surgical specimens, to unify criteria. The aim of this work is to assess its application in forensic autopsies. A secondary objective is to study inflammatory changes useful for dating.
Material and methodsAortic histological preparations of the 54 cases of SD due to aortic rupture/dissection studied between 2019 and 2022 were reviewed.
ResultsMedial degeneration was observed in 49 cases (90.8%) (severe in 42.9%). By lesions, the order of frequency was: fragmentation and/or loss of elastic fibres (74.1%), accumulation of extracellular mucoid matrix (61.1%), loss of smooth muscle cell nuclei (48.1%), and collapse of the media (44.4%). Some lesions of the consensus paper could not be assessed. No significant differences were found by age; presence or not of collagenopathies; or bi/tricuspid aortic valves. Granulation tissue or neutrophilic infiltrate was observed in those deceased with pain several days or <24 h before death, respectively.
ConclusionWith the application of the document, lesions in the media are found in >90% of cases and fundamental lesions can be studied. The inflammatory response to rupture/dissection appears to correlate with the timing of dissection/rupture.
La disección/rotura de aorta torácica tiene una alta mortalidad, constituyendo del 3,9-5,4% de las muertes súbitas (MS) en series forenses. Los hallazgos histopatológicos de la media asociados a estas entidades han recibido múltiples términos y definiciones. En 2016, la Asociación Europea de Patología Cardiovascular junto con la Sociedad de Patología Cardiovascular publicaron un documento de consenso, aplicado a muestras quirúrgicas, para unificar criterios. El objetivo de este trabajo es valorar su aplicación en autopsias forenses. Un objetivo secundario es estudiar cambios inflamatorios útiles para la datación.
Material y métodosSe revisaron las preparaciones histológicas de aorta de los 54 casos de MS por rotura/disección aortica estudiados entre 2019–2022.
ResultadosSe observó degeneración de la media en 49 casos (90,8%) (severa en 42,9%). Por lesiones, el orden de frecuencia fue: fragmentación y/o pérdida de las fibras elásticas (74,1%); acúmulo de matriz mucoide extracelular (61,1%); pérdida de núcleos de células musculares lisas (48,1%) y colapso de la media (44,4%). Algunas lesiones del documento no pudieron ser valoradas. No se encontraron diferencias significativas por edad; presencia o no de colagenopatías; o válvulas aórticas bi/tricúspides. Se observó tejido de granulación o infiltrado neutrofílico en fallecidos con dolor varios días o < 24 h antes de la muerte, respectivamente.
ConclusiónCon la aplicación del documento se encuentran lesiones en la media en >90% de los casos y pueden estudiarse las lesiones fundamentales. La respuesta inflamatoria frente a la rotura/disección parece correlacionarse con el momento de la disección/rotura.
Dissection and rupture of the thoracic aorta are medical emergencies with a high mortality rate, estimated at 26% in patients who have undergone surgery and up to 58% in those who have not received surgical treatment,1 and account for between 3.9% and 5.4% of the causes of sudden death in forensic series.2–5 The incidence of acute aortic dissection is estimated at between 2.53 and 15/100 000/year.6
Hypertension (HT) is the main risk factor in older people, but there are other factors such as bicuspid aortic valve (BAV), a history of cardiac surgery, smoking, direct chest trauma, pregnancy, isometric exercise, and cocaine and amphetamine use.5–10 Dissections associated with genetic syndromes such as Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome type IV, or Turner syndrome are noteworthy.7,9,11,12
The description of the histological findings found in aortic rupture and dissection dates back to 1930, when Erdheim described medionecrosis.13 Since then, the medical literature has included multiple terms and definitions such as cystic medial necrosis, cystonecrosis, cystic degeneration, or mucoid degeneration, among others.9 A committee formed by members of the Association for European Cardiovascular Pathology (AECVP) and the Society for Cardiovascular Pathology (SCVP) was formed to unify criteria, and in 2016, they published a consensus document to cover 3 general aspects: 1) to provide a unified nomenclature to the histopathological findings of the non-inflammatory degenerative ascending aorta, 2) to provide a new grading scheme to better classify aortic lesions, and 3) to catalogue the primary medial degenerative diseases of the aorta along with current knowledge regarding mutated genes and known associated histological findings.9
Since then, several studies have been published applying the new criteria to histopathological findings in the aortic wall of patients undergoing surgery for acute aortic syndromes or dilatation of the ascending aorta,1,14–18 but to our knowledge, no study has been published on autopsy samples.
The main objective of this study is to assess the application of the criteria proposed in the AECVP/SCVP consensus document to autopsy specimens of sudden death due to aortic rupture/dissection. A secondary objective is to study reactive inflammatory changes in the media and adventitia useful for dating aortic dissections.
Material and methodsWe conducted a retrospective study of the cases of sudden death due to aortic rupture/dissection studied in our service between 2019 and 2022. Personal and family medical history, symptomatology prior to death, and autopsy findings were collected, as well as the results of toxicological analyses from cases in which they were performed.
The study of the heart was performed following the 2017 guidelines for the investigation of sudden cardiac death.19 Sex, height, and body weight were considered to calculate heart weight.20,21
Histological sections of the ascending aorta were studied in all cases, and of the descending or abdominal arch and aorta when the sample was available. The aortic wall was studied in the area of rupture/dissection zone and in the healthy area as a control. The preparations underwent haematoxylin-eosin, collagen (Masson's trichrome), and elastic fibre (Weigert) staining, and in some cases were stained with Alcian blue for mucopolysaccharides. Following the consensus document on the age at which medial degeneration may be of genetic origin, 9 the cases were divided into 2 groups: ≤49 years and ≥50 years.
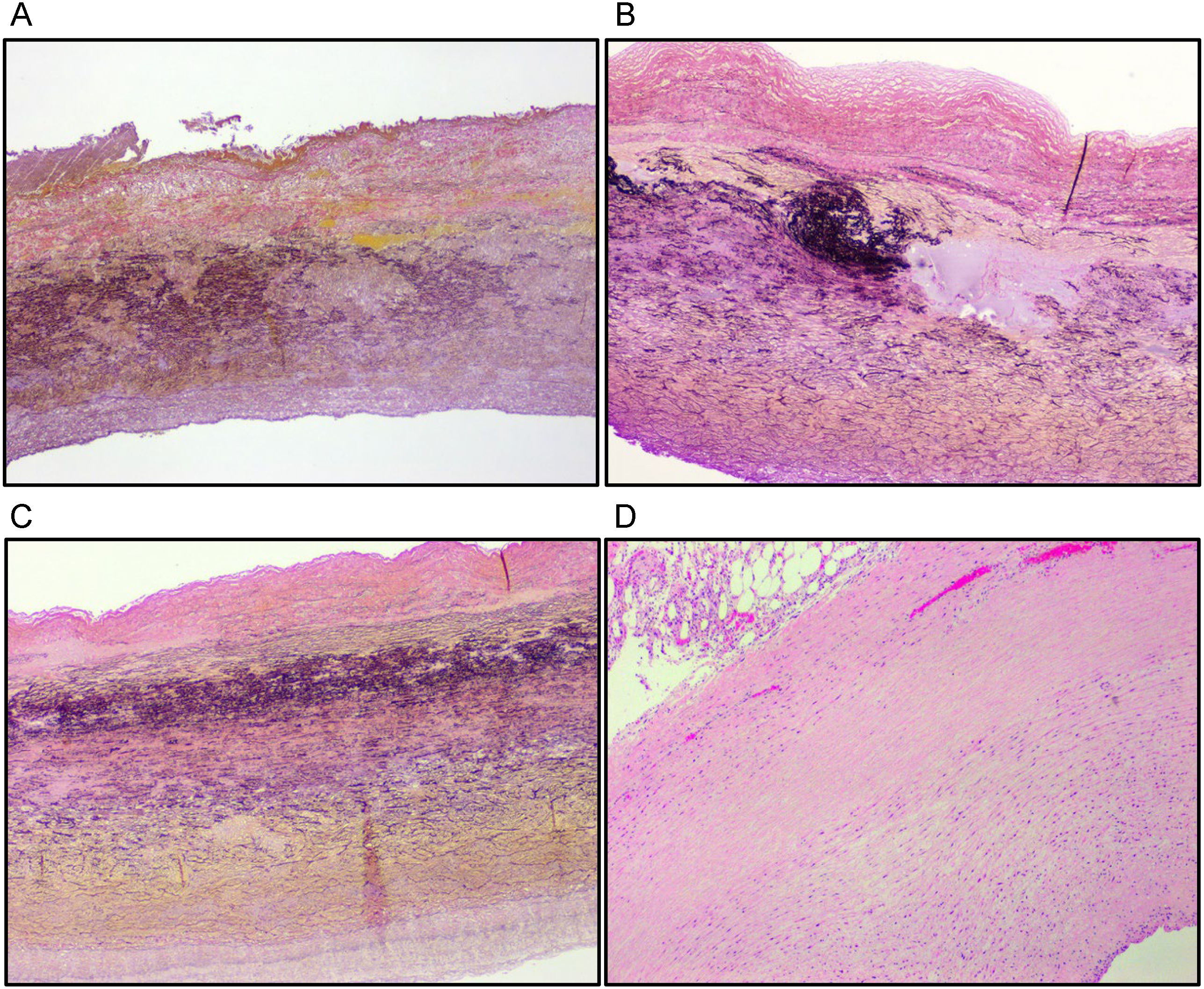
We initially attempted to analyse all the lesions detailed in the consensus document but, given the subjectivity and difficulty in assessing some, such as thinning and disorganisation of elastic fibres, and medial fibrosis, we opted to analyse only those lesions considered highly recommended for adequate assessment of medial degeneration: mucoid extracellular matrix accumulation (MEMA) (intralamellar and translamellar), elastic fibre fragmentation and/or loss (EFF), smooth muscle cell nuclei loss (SMCL), and lamellar medial collapse (LMC)9 (Fig. 1). Three pathologists examined the cases individually and borderline cases were assessed together.
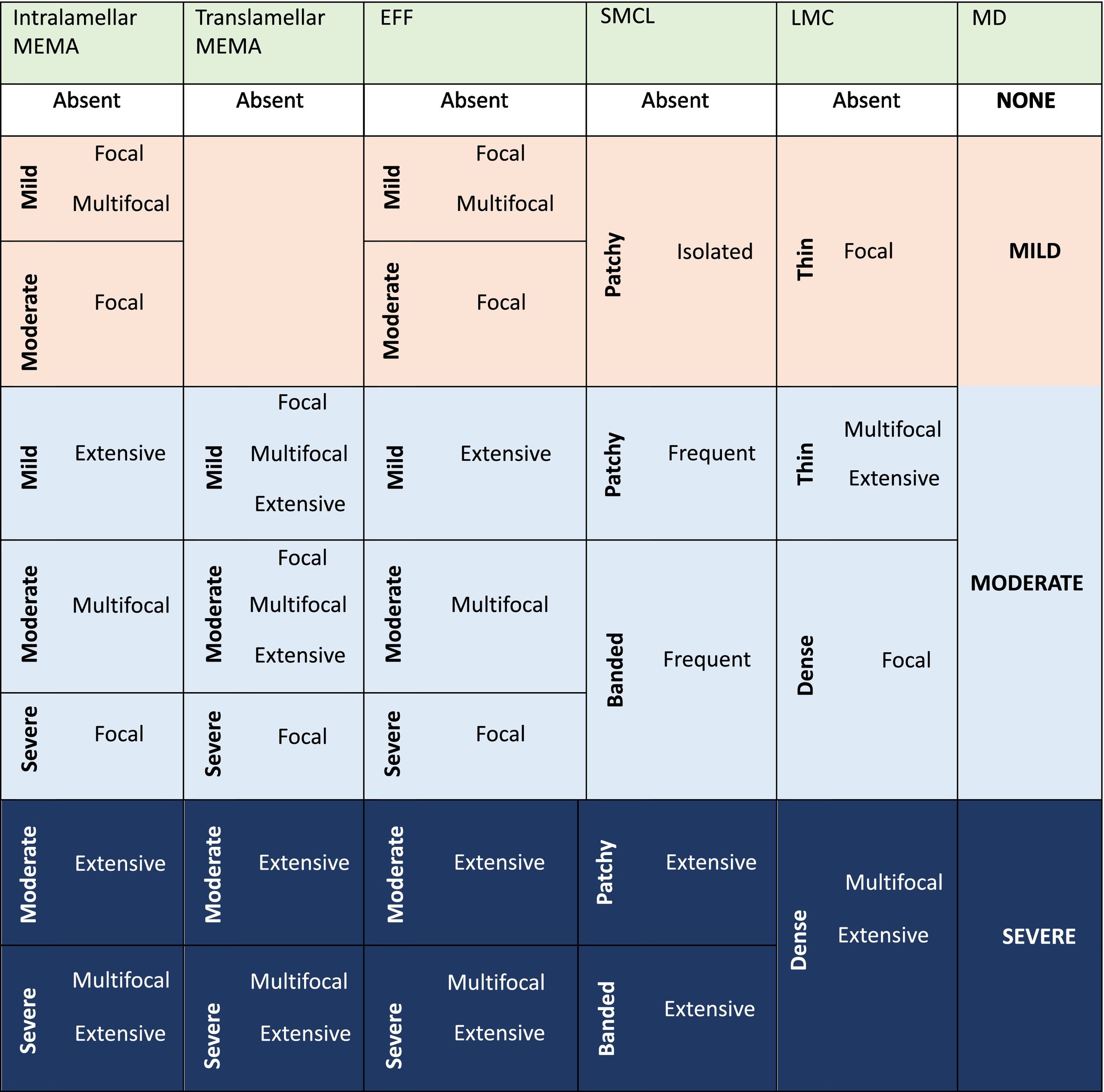
To determine the overall severity of medial degeneration (MD), the lesions were first evaluated individually, determining the grade (mild, moderate, severe) and extent/distribution (focal, multifocal, extensive) according to Fig. 8 in Supplemental File 1 of the guideline.9 Then, following the table in the consensus document (Table 1) they were globally classified as mild, moderate, or severe. In those cases in which the severity of each of the lesions analysed was disparate, we used the case examples (Supplemental File 3 and Figs. 9–12) of the supplement to the consensus document.9 In those cases where it was still not possible to determine the grade of global medial degeneration, the grade given to EFF was considered decisive, on the understanding that the presence of this severe-grade lesion affected the structure and resistance of the aortic wall very significantly,22 even in the absence of other lesions or with the presence of another mild-grade lesion.
Grading scheme of the consensus to evaluate medial degeneration.
ACTA2: actin alpha 2; EFF: elastic fibre fragmentation and/or loss; LMC: lamellar medial collapse; MEMA-I: intralamellar mucoid extracellular matrix accumulation; MD: medial degeneration; MEMA-T: translamellar mucoid extracellular matrix accumulation; SMCL: sooth muscle cell nuclei loss; TGFBR1: transforming growth factor beta receptor 1.
Categorical variables are expressed as numbers and percentages; continuous variables are expressed as mean±standard deviation. Categorical variables were compared with the χ2 test and Fisher's exact test was used when frequencies were less than 5.
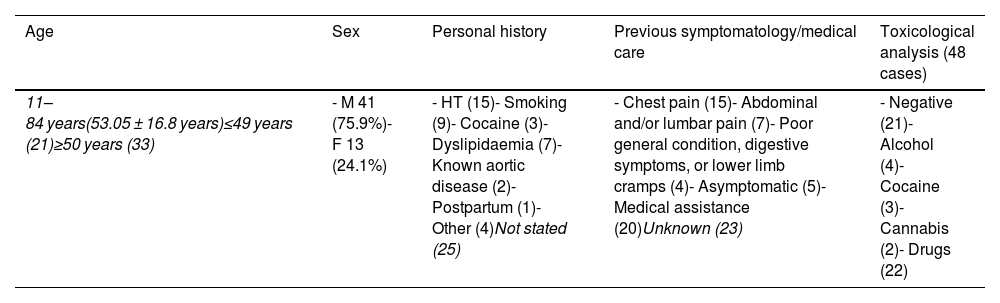
ResultsOf a total of 1675 sudden deaths of cardiovascular origin studied between 2019 and 2022, 54 (3.2%) were due to aortic rupture/dissection: 41 men (75.9%) and 13 women (24.1%) aged between 11 and 84 years (mean age: 53.05±16.8 years) (Table 2). Of the 29 deaths with a known personal history, the most frequent was HT. Only 2 of the deceased had a history of aortic pathology (a 52-year-old man and a 65-year-old woman under follow-up for aortic aneurysm). As previous symptomatology, this information was only available in 31 cases, with chest or abdominal/lumbar pain being of note in 22 (71%). Thirty-seven percent received medical care prior to death without making a diagnosis of certainty.
General data.
| Age | Sex | Personal history | Previous symptomatology/medical care | Toxicological analysis (48 cases) |
|---|---|---|---|---|
| 11–84 years(53.05 ± 16.8 years)≤49 years (21)≥50 years (33) | - M 41 (75.9%)- F 13 (24.1%) | - HT (15)- Smoking (9)- Cocaine (3)- Dyslipidaemia (7)- Known aortic disease (2)- Postpartum (1)- Other (4)Not stated (25) | - Chest pain (15)- Abdominal and/or lumbar pain (7)- Poor general condition, digestive symptoms, or lower limb cramps (4)- Asymptomatic (5)- Medical assistance (20)Unknown (23) | - Negative (21)- Alcohol (4)- Cocaine (3)- Cannabis (2)- Drugs (22) |
Toxicological studies were performed in 48 cases (88.9%) with positive blood results in 27 (56.2%) (Table 2). Alcohol consumption was demonstrated in 4 cases, associated in one with cocaine and cannabis, and in another with cocaine and tramadol; cocaine was detected in another case associated with cannabis and benzodiazepines; other findings were the presence of benzodiazepines, antidepressants, sildenafil, and drugs related to cardiopulmonary resuscitation manoeuvres. The result was negative in 21 cases (43.7%).
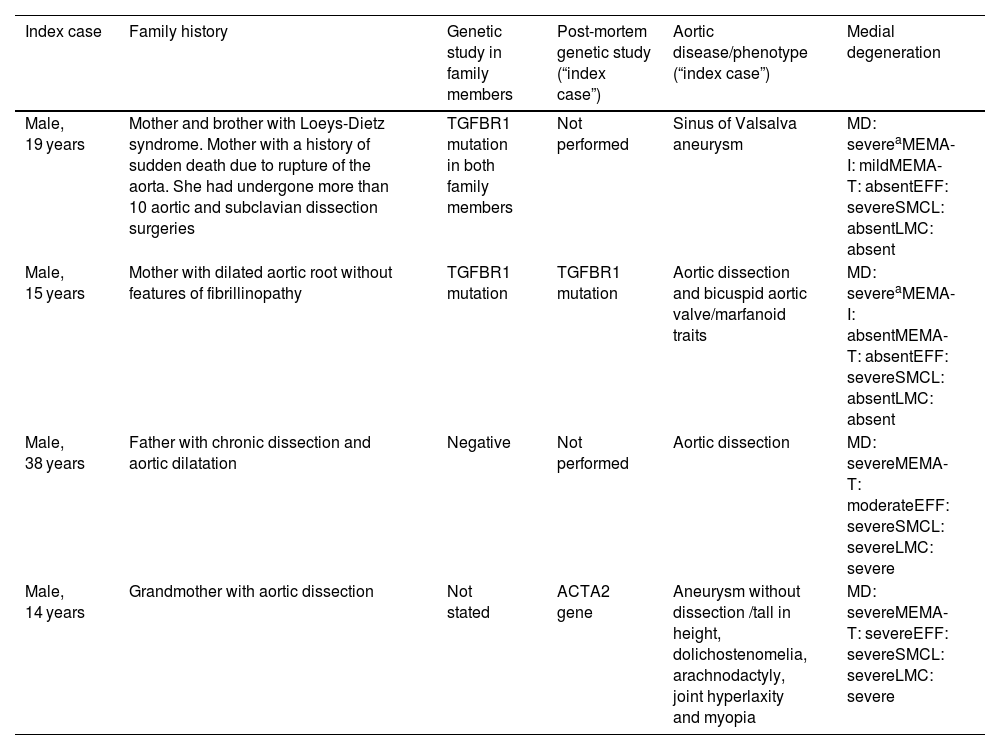
In terms of family history, 4 cases had a history of aortic disease, and 3 of these families underwent genetic study, finding pathogenic variants in the TGFBR1 gene in 2, one with a diagnosis of Loeys-Dietz syndrome. In the second of these cases, the result was also positive in the deceased, a 15-year-old male with marfanoid habitus. In a 14-year-old male, also with marfanoid habitus, the post-mortem genetic study identified a probably pathogenic variant in the ACTA2 gene (Table 3).
Family history of aortic disease and genetic studies.
| Index case | Family history | Genetic study in family members | Post-mortem genetic study (“index case”) | Aortic disease/phenotype (“index case”) | Medial degeneration |
|---|---|---|---|---|---|
| Male, 19 years | Mother and brother with Loeys-Dietz syndrome. Mother with a history of sudden death due to rupture of the aorta. She had undergone more than 10 aortic and subclavian dissection surgeries | TGFBR1 mutation in both family members | Not performed | Sinus of Valsalva aneurysm | MD: severeaMEMA-I: mildMEMA-T: absentEFF: severeSMCL: absentLMC: absent |
| Male, 15 years | Mother with dilated aortic root without features of fibrillinopathy | TGFBR1 mutation | TGFBR1 mutation | Aortic dissection and bicuspid aortic valve/marfanoid traits | MD: severeaMEMA-I: absentMEMA-T: absentEFF: severeSMCL: absentLMC: absent |
| Male, 38 years | Father with chronic dissection and aortic dilatation | Negative | Not performed | Aortic dissection | MD: severeMEMA-T: moderateEFF: severeSMCL: severeLMC: severe |
| Male, 14 years | Grandmother with aortic dissection | Not stated | ACTA2 gene | Aneurysm without dissection /tall in height, dolichostenomelia, arachnodactyly, joint hyperlaxity and myopia | MD: severeMEMA-T: severeEFF: severeSMCL: severeLMC: severe |
ACTA2: actin alpha 2; EFF: elastic fibre fragmentation and/or loss; LMC: lamellar medial collapse; MD: medial degeneration; MEMA-I: intralamellar mucoid extracellular matrix accumulation; MEMA-T: translamellar mucoid extracellular matrix accumulation; SMCL: sooth muscle cell nuclei loss; TGFBR1: transforming growth factor beta receptor 1.
The grade of MD in these 2 cases could not be determined following Table 1 or the example cases (Supplemental Files and Figures) of the consensus document,9 and therefore the grade of EFF found was considered decisive, taking into account that a severe grade of this lesion significantly affects the structure and resistance of the aortic wall,22 even in the absence of other lesions.
The post-mortem genetic study of a case in which a variant of uncertain significance was found in the filamin A (FLNA) gene is also available; this case had a history of sudden death in a young family member.
Two other cases had a family history of unspecified sudden cardiac death.
Histopathological findingsOf the 54 deceased patients, 49 presented aortic dissection (90.7%); in one 19-year-old male, the dissection occurred over an aneurysm of the sinus of Valsalva.
In terms of the mechanism of death, in 49 cases, death was caused by cardiac tamponade, in 4 by haemothorax, and in 1 case by acute myocardial infarction secondary to the extension of the dissection to the anterior descending coronary artery.
The mean heart weight in the men was 515±137.8 g and in the women 441.4±100.8 g. Heart weight was above the 95th percentile for sex, body weight, and height in 25/38 cases (65.8%). Heart weight could not be accurately assessed in 15 cases due to a lack of anthropometric data, and in 1 case the whole heart was not submitted.
In 44 hearts, tears of the aortic intima located between 0.1 and 8 cm above the sinotubular junction were identified (mean distance: 1.92 cm). The size of the tear ranged from 0.7 to 10 cm in length. In 2 cases, the intimal rupture was located in the descending aorta. The aortic valve was bicuspid in 6 cases (11.1%); in 1 case, it could not be examined because only biventricular sections of the heart and a segment of ascending aorta were submitted. There were 10 cases in which the submitted segment of ascending aorta was very short and no intimal tear was identified.
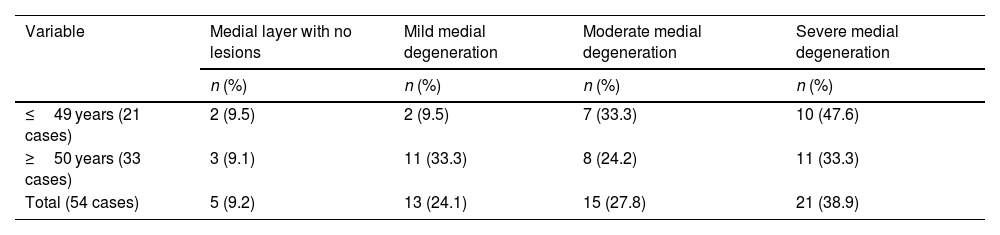
Mild MD was found in 24.1%, moderate MD in 27.8%, and severe MD in 38.9%. If we consider age, we observe that degeneration lesions of the medial layer were found in 19/21 cases of the group ≤49 years (90.5%), most of severe grade (10 cases). In the group aged ≥50 years, MD was observed in 30/33 cases (90.9%), and was severe in 11 cases and mild in 11 cases. There were 5 cases (9.2%) with no medial lesions. There were no statistically significant differences (P<.05) in relation to age (Table 4).
Grade of medial degeneration by age group.
| Variable | Medial layer with no lesions | Mild medial degeneration | Moderate medial degeneration | Severe medial degeneration |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| ≤49 years (21 cases) | 2 (9.5) | 2 (9.5) | 7 (33.3) | 10 (47.6) |
| ≥50 years (33 cases) | 3 (9.1) | 11 (33.3) | 8 (24.2) | 11 (33.3) |
| Total (54 cases) | 5 (9.2) | 13 (24.1) | 15 (27.8) | 21 (38.9) |
The χ2 test and Fisher's exact test were not statistically significant for P<.05.
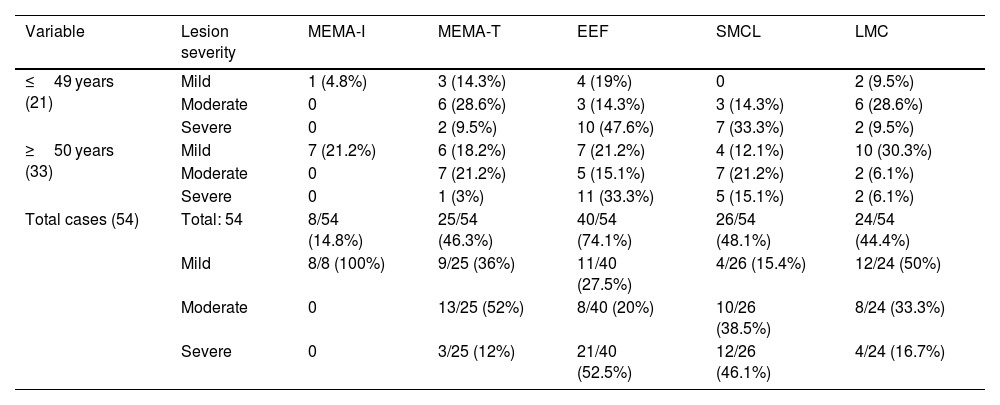
For the MD lesions analysed individually, EFF was the histological lesion most frequently found, in 40 cases (74.1%), followed by MEMA in 33 cases (61.1%), of which 8 presented intralamellar accumulation and 25 cases translamellar accumulation. SMCL was found in 26 cases (48.1%), in 22 of these, the type was banded and in 4 cases, it was patchy. LMC was found in 24 cases (44.4%) (Table 5). There were no statistically significant differences (P<.05) in relation to age. Severe MD was observed in the 4 cases with a family history of aortic disease, and severe grade EFF was the lesion present in all cases, while MEMA was severe in one case, moderate in another, and absent in the other 2 (Table 3).
Medial degeneration lesions.
| Variable | Lesion severity | MEMA-I | MEMA-T | EEF | SMCL | LMC |
|---|---|---|---|---|---|---|
| ≤49 years (21) | Mild | 1 (4.8%) | 3 (14.3%) | 4 (19%) | 0 | 2 (9.5%) |
| Moderate | 0 | 6 (28.6%) | 3 (14.3%) | 3 (14.3%) | 6 (28.6%) | |
| Severe | 0 | 2 (9.5%) | 10 (47.6%) | 7 (33.3%) | 2 (9.5%) | |
| ≥50 years (33) | Mild | 7 (21.2%) | 6 (18.2%) | 7 (21.2%) | 4 (12.1%) | 10 (30.3%) |
| Moderate | 0 | 7 (21.2%) | 5 (15.1%) | 7 (21.2%) | 2 (6.1%) | |
| Severe | 0 | 1 (3%) | 11 (33.3%) | 5 (15.1%) | 2 (6.1%) | |
| Total cases (54) | Total: 54 | 8/54 (14.8%) | 25/54 (46.3%) | 40/54 (74.1%) | 26/54 (48.1%) | 24/54 (44.4%) |
| Mild | 8/8 (100%) | 9/25 (36%) | 11/40 (27.5%) | 4/26 (15.4%) | 12/24 (50%) | |
| Moderate | 0 | 13/25 (52%) | 8/40 (20%) | 10/26 (38.5%) | 8/24 (33.3%) | |
| Severe | 0 | 3/25 (12%) | 21/40 (52.5%) | 12/26 (46.1%) | 4/24 (16.7%) |
The χ2 test and Fisher's exact test were not statistically significant for P<.05. EFF: elastic fibre fragmentation and/or loss; LMC: lamellar medial collapse; MEMA-I: intralamellar mucoid extracellular matrix accumulation; MEMA-T: translamellar mucoid extracellular matrix accumulation; SMCL: smooth muscle cell nuclei loss.
MD was present in 5 (83.3%) of the 6 cases with BAV, moderate in 2 (1 at 15 days postpartum), and severe in the other 3. In terms of the lesion, EFF was observed in all 5 cases and translamellar MEMA, SMCL, and LMC were observed in 3 (60%).
Of the 47 cases with tricuspid aortic valve (TAV), 43 cases (91.5%) had MD, which was mild in 12 cases (27.9%), moderate in 13 cases (30.2%), and severe in 18 cases (41.9%). EFF was the most frequently found lesion, seen in 35 cases (81.4%). MEMA was found in 30 cases (69.8%). SMCL was seen in 23 cases (53.5%) and LMC was present in 21 cases (48.8%). In a comparative analysis between cases with TAV and BAV, no differences were observed in the frequency of the lesions considered individually or in the overall assessment of MD.
The 5 cases with aortic rupture without dissection were: a 14-year-old male with a marfanoid phenotype (Table 3), a 44-year-old male with BAV, a 52-year-old male with an ascending aortic aneurysm, a 76-year-old woman with giant cell aortitis, and the last case was an 84-year-old woman. There was severe MD in 4 of these cases and no lesions were found in 1 case (with BAV).
In the 3 cases in which the chemical-toxicological analysis showed the presence of cocaine, the patients were habitual users. The MD found was severe in 1 case and moderate in the other 2 cases. SMCL and LMC were found in all 3 cases. EFF and MEMA were found in 2.
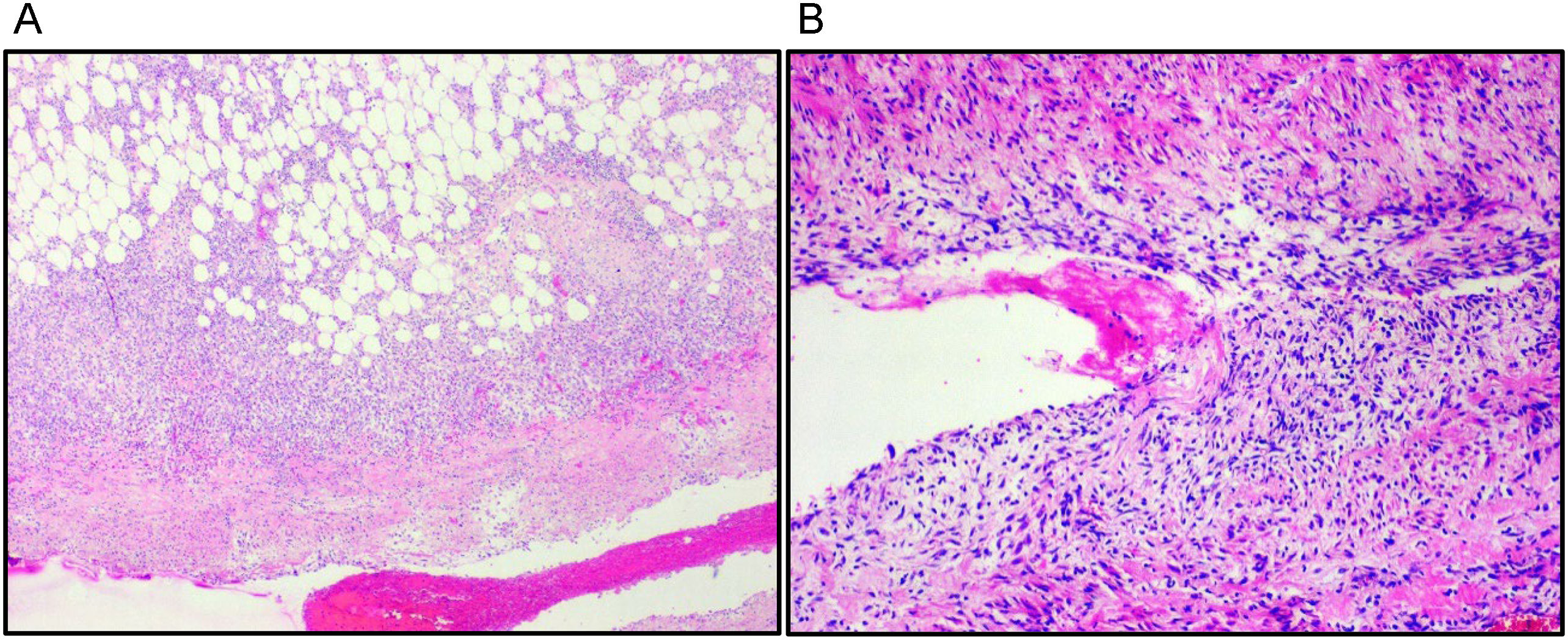
In 15 cases, granulation tissue was observed in the periaortic epicardium and in 3 cases, there was also granulation tissue in the dissection plane in the medial layer (Fig. 2); 8 of these cases had reported chest pain between 2 and 7 days prior to death, 7 of them had received health care, with normal complementary cardiological tests in 4 of these cases. In the other 7 patients who died with this finding, the symptoms prior to death were unknown. In another 4 cases, a neutrophilic infiltrate was detected in the aortic adventitia, 3 had reported chest pain, and 1 case reported epigastralgia and vomiting the day before or the same day of death, and all 4 cases had seen a physician.
DiscussionThe estimated incidence of aortic dissection varies between 2.53 and 15/100 000/year6 and mortality (without surgical treatment) is 58%, generally due to rupture of the wall in the pericardial sac and less frequently in the mediastinum or retroperitoneum. In forensic series of sudden death, aortic dissection accounts for 3.9%–5.4%,2–5 similar to the incidence we observed in our study (3.2%), although histopathological study was probably not requested in many cases because the cause of death was evident at autopsy.
The higher proportion of men (75.9%) compared to women (24.1%) found in the present study coincides with that reported in the literature.5,6,8,15,16
HT is the most important risk factor for dissection.1,5,6,9,14,15,17,23,24 In our study, we recorded this history in only 15 cases (27.8%), but most probably the number of hypertensive patients was greater since cardiac hypertrophy was observed in 65.7% of the cases with the available anthropometric data.
Hormonal changes occur during pregnancy that can weaken the aortic wall (fragmentation of the elastic fibres, reduction of acid mucopolysaccharides, and loss of the normal undulation of the elastic fibres), as well as haemodynamic changes associated or not with HT, which are risk factors for developing aortic complications;25,26 the association with other factors such as Marfan syndrome or BAV (present postpartum in our series), where the elasticity of the aortic wall is abnormal, could favour aortic dissection.26,27 Kamel et al. conducted a comparative study of 36 pregnant and 9 non-pregnant women with acute aortic syndrome (AAS), identifying that the period of risk in pregnant women increased up to 3 months postpartum.26
The predominant symptom prior to death found in our review was chest pain (57.7%), which coincides with most published series,5–7,14,28 although, in a recently published study, abdominal pain was more frequent than chest pain (29.5% versus 20%).24 The varied clinical presentation and the fact that a clinical diagnosis of certainty prior to death was not made in any of the cases coincides with the review by Morentin et al.5 and confirms the difficulty in clinically diagnosing thoracic aortic dissection/rupture in some cases.
Overall, we found medial lesions in 90.8% of the cases studied compared to 77% in another autopsy series 5 and they were observed in 4 of the 5 cases with rupture without dissection.
Schlatmann et al. demonstrated that with age in the normal aorta, accumulation of mucopolysaccharides, fragmentation of the elastic fibres, fibrosis, and smooth muscle cell nuclei loss, produced by a phenomenon of injury and repair associated with haemodynamic events, occurs in the innermost layer of the media.29 These lesions are similar to those found in genetic aortic syndromes, but these occur in younger individuals and the lesions are more extensive.9 These data coincide with our results where, although MD was of a fundamentally severe grade, in almost half the cases in the group ≤49 years, and was severe in one-third ≥50 years, there were no statistically significant differences. The prevalence of a medial layer without lesions was similar in both groups (Table 4).
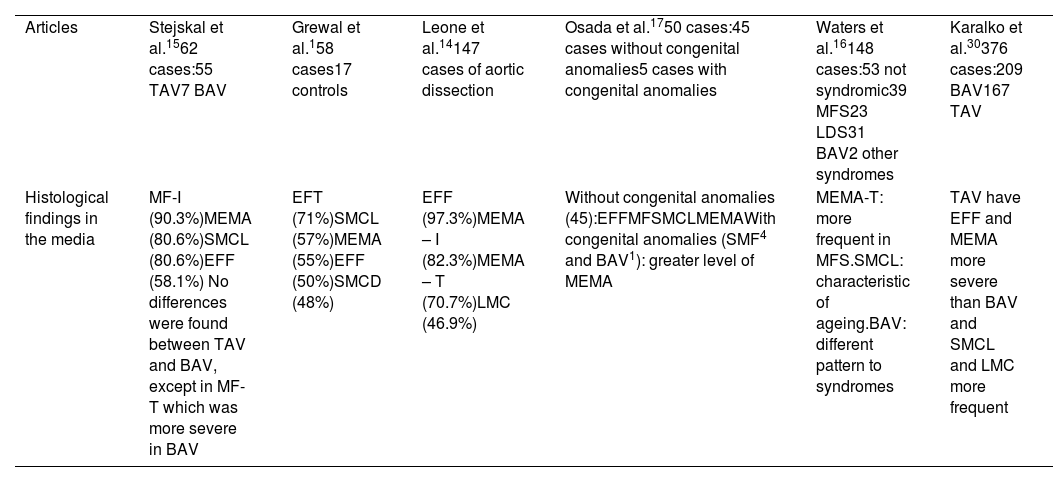
Regarding the lesions studied individually, the lesions analysed and the frequency of each vary according to the series. In some studies,14,16 as in our study, EFF is the most frequent, while in others intralamellar fibrosis 15 and thinning of the elastic fibres were the most frequent1 (Table 6). We should highlight that in our study, we did not analyse the latter due to the subjective nature of assessing them and because they are not included in those that the consensus document considers highly advisable to assess. In the lesions studied, we found no differences in prevalence according to age, EFF being the most frequent lesion in both groups (Table 5).
Medial lesions according to surgical series.
| Articles | Stejskal et al.1562 cases:55 TAV7 BAV | Grewal et al.158 cases17 controls | Leone et al.14147 cases of aortic dissection | Osada et al.1750 cases:45 cases without congenital anomalies5 cases with congenital anomalies | Waters et al.16148 cases:53 not syndromic39 MFS23 LDS31 BAV2 other syndromes | Karalko et al.30376 cases:209 BAV167 TAV |
| Histological findings in the media | MF-I (90.3%)MEMA (80.6%)SMCL (80.6%)EFF (58.1%) No differences were found between TAV and BAV, except in MF-T which was more severe in BAV | EFT (71%)SMCL (57%)MEMA (55%)EFF (50%)SMCD (48%) | EFF (97.3%)MEMA – I (82.3%)MEMA – T (70.7%)LMC (46.9%) | Without congenital anomalies (45):EFFMFSMCLMEMAWith congenital anomalies (SMF4 and BAV1): greater level of MEMA | MEMA-T: more frequent in MFS.SMCL: characteristic of ageing.BAV: different pattern to syndromes | TAV have EFF and MEMA more severe than BAV and SMCL and LMC more frequent |
BAV: bicuspid aortic valve; EFF: elastic fibre fragmentation and/or loss; EFT: elastic fibre thinning; LDS: Loeys-Dietz syndrome; LMC: laminar medial collapse; MEMA: mucoid extracellular matrix accumulation (I: intralamellar and T: translamellar); MF-I: medial fibrosis (I: intralamellar and T: translamellar); MFS: Marfan syndrome; SMCD: smooth muscle cell disorganisation; SMCL: smooth muscle cell nuclei loss; TAV: tricuspid aortic valve.
Comparative studies of aortic media lesions without congenital diseases and with some collagen disease, find that the aortas of patients with Marfan syndrome have severe MEMA.9,16,17 In our 4 deceased patients with a family history, although 3 had MEMA, it was only of severe grade in one case with Marfan traits associated with a variant in the ACTA-2 gene and was of mild grade in the case of the family with Loeys-Dietz syndrome (Table 3).
BAV is the most common valvular malformation with an incidence in the general population of 0.5%–2%.31–33 The risk of dissection is much higher than that of TAV and its prevalence in series of aortic dissection varies between 3.8% and 43%,1,5,6,10,14,15 in our review, the prevalence was 11.3%. In 1999, Parai et al. observed, by means of histological studies with morphometry of aortas from autopsies, fewer elastic fibres in the aortic media of patients with BAV, which could explain their propensity for dissection.34 In recent studies comparing medial lesions in dissections with BAV and TAV, some authors observed no differences,15,16 while others found that in cases with TAV, EFF, MEMA, SMCL, LMC, and elastic fibre thinning were more prominent than in cases with BAV.30,35 Of the 6 cases of BAV in our series, half had severe MD in line with other studies,14 but there were no differences with respect to TAV cases although our sample is very limited.
Biomechanical studies have determined that there are areas of the aortic wall that are exposed to greater stress, specifically above the sinotubular junction and distal to the ostium of the left subclavian artery. These areas correlate with the sites where intimal tears most frequently occur.35 In the review by Morentin et al.,5 aortic rupture was found at a mean of 2.10 cm above the sinotubular junction, similar to our study where the mean was 1.92 cm.
Cocaine consumption is a known risk factor for the development of vascular diseases such as acute coronary syndromes, myocardial infarction, or stroke, but it also increases the risk for aortic dissection/rupture,5,7,9,28,36,37 being implicated in 1.8% of patients with aortic dissection, according to data from the International Registry of Acute Aortic Dissection.38 It occurs especially in young hypertensive men with left ventricular hypertrophy and smokers,28,39 although <1% of cocaine users present aortic dissection.40 Increased diastolic diameter, loss of elasticity, and increased aortic stiffness have been observed in chronic users;41,42 sudden elevation of blood pressure and tachycardia, a consequence of acute cocaine use, would cause dissection by affecting a weakened aortic wall.28,40
It is possible that in our 3 cases with positive results from chemical-toxicological analysis for cocaine, and who were also regular users, the medial lesions found (SMCL and LMC of moderate/severe grade and mild MEMA) could have predisposed to rupture.
Aortic dissection is a disease that is very difficult to diagnose, which means that in many cases medical reports, where possible, need to date the time of onset. The inflammatory response in the periaortic epicardium and/or in the dissection plane can provide valuable information regarding the dating of the lesions. The granulation tissue identified in 15 cases could be explained by blood filtration prior to rupture, consistent with the clinical manifestations of chest pain in the preceding days; whereas, in the 4 cases with neutrophilic inflammatory infiltrate, the symptoms appeared a few hours before death. These results coincide with the histologic evolution published by Xu and Burke in samples from surgical resections.36
Conclusions- •
The standardisation of the nomenclature and classification of degenerative aortic media lesions provided by the AECVP/SCVP consensus document are applicable to samples from sudden deaths, although the identification of some of the lesions described is subjective, and the overall assessment of MD is difficult when there is great variability in the intensity of the lesions considered individually.
- •
Application of the AECVP/SCVP consensus document allows the detection of medial lesions in most of those who died from aortic rupture (90.8%).
- •
No differences by age were found in the prevalence of lesions considered individually, although considered globally, severe MD was more frequent ≤49 years.
- •
EFF was the most frequently encountered lesion, with no differences by age. No greater prevalence of MEMA was seen in young people or in deceased people with a family history of aortic disease. Neither is BAV associated with specific lesions.
- •
Aortic rupture/dissection was also observed in cases in which the aortic media did not present lesions.
- •
The study of the inflammatory response in the periaortic tissue and in the dissection plane of the media could be useful to estimate time of onset.
Considering that these are forensic autopsy cases, the information available in many cases is very limited, primarily on personal and family medical history, the presence or absence of symptoms prior to death, etc.
A case–control study applying the consensus document is necessary to determine the relevance of medial lesions in the pathophysiology of aortic dissection/rupture.
The number of cases examined is very limited.
FundingThe present research study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors are grateful for the work of the technicians of the Histopathology Services of the Madrid Department of the National Institute of Toxicology and Forensic Sciences. We would also like to thank JL Merino Llorens for the statistical analysis.
Please cite this article as: García-Pérez JL, Martín-Gómez M and Suárez-Mier MP. Histopathological findings in dissection and rupture of the thoracic aorta. Study of 54 autopsy cases. Revista Española de Medicina Legal. 2024. https://doi.org/10.1016/j.reml.2023.03.002.