Vaccination for COVID-19 in healthcare workers (HCW) is essential to protect one of the populations most exposed to this disease. However, data on the humoral response rate to the vaccine and the factors associated with it in this population are limited. Therefore, we aimed to evaluate the antibody response against SARS-CoV-2 in HCWs with complete Sputnik V vaccine scheme and factors associated with an increased antibody response.
Material and methodsProspective study to evaluate the anti-SARS-CoV-2 humoral response in HCWs vaccinated with two doses of the Sputnik V vaccine (April-July 2021). The assessment of anti-Spike IgG antibodies in plasma was performed using the COVIDAR IgG enzyme-linked immunosorbent assay. A logistic regression was performed to identify independent factors associated with a positive IgG serology test and an elevated antibody response.
ResultsA total of 630 HCWs were enrolled. Median age (IQR): 47 years (35-56). Female sex: 462 (73.33%). Previous COVID-19: 158 (25%). The median interval time between vaccine doses was 3 (3-4) weeks. Positive serology was observed in 607 (96.35%) HCWs. In the multivariate analysis, a history of systemic reactogenicity was identified as an independent variable associated with a positive serology; and history of systemic reactogenicity, COVID-19, interval between doses ≥4 weeks and time to serology <14 weeks were associated with an elevated antibody response.
ConclusionsThis study provides data on the humoral response to the Sputnik V vaccine in a real-life setting. These initial data can contribute to the development of future immunization strategies in HCWs.
Introducción
La vacunación para COVID-19 en el personal de salud (PDS) es fundamental para proteger a una de las poblaciones más expuestas a esta enfermedad. Sin embargo, los datos de la tasa de respuesta humoral a la vacuna y los factores asociados a la misma en esta población son limitados. Nuestros objetivos fueron evaluar la respuesta de anticuerpos contra SARS-CoV-2 en el PDS con esquema completo de vacuna Sputnik V y los factores asociados con una mayor respuesta de anticuerpos.
Materiales y métodos
Estudio prospectivo de evaluación de la respuesta humoral anti SARS-CoV-2 en PDS con esquema completo de vacuna Sputnik V mediante el enzimoinmunoensayo COVIDAR IgG (abril–julio 202). Se realizó una regresión logística para identificar factores independientes asociados con una prueba de serología IgG positiva y con respuesta elevada de anticuerpos.
Resultados
Se enrolaron 630 PDS. Mediana (RIC) de edad: 47 años (35-56). Sexo femenino: 462 (73.33%). COVID previo: 158 (25%). Mediana de tiempo entre las dosis de vacuna fue 3 (3-4) semanas. Presentaron serología reactiva 607 (96.35%). En el análisis multivariado se identificó como variable independiente asociada a serología positiva al antecedente de reactogenicidad sistémica a la vacuna; y con respuesta elevada de anticuerpos al antecedente de reactogenicidad sistémica a la vacuna, COVID-19 previo, intervalo entre dosis ≥4 semanas y tiempo a serología <14 semanas.
Conclusiones
Este estudio proporciona datos de la respuesta humoral a la vacuna Sputnik V en un escenario de vida real. Estos datos iniciales pueden contribuir al desarrollo de futuras estrategias de inmunización en el personal de salud.
Infection with the SARS-CoV-2 virus, the aetiological agent of COVID-19 disease, was declared a pandemic by the World Health Organisation in March 2020. To date, more than 190 million people have been infected and some four million have died from COVID-19.1 Health care workers (HCWs) are a key population in this disease as they are highly exposed and are one of the hardest-hit groups by the pandemic. Consequently, vaccination against SARS-CoV-2 in HCWs is a priority and fundamental strategy to prevent the spread of this new infection in healthcare institutions and to prevent the entire healthcare system from collapsing.2
To date, more than 10 vaccines against COVID-19 have been approved or licensed in different parts of the world.3 The Sputnik V vaccine (Gam-COVID-Vac) was the first to be launched in our country, in addition to being the most widely used vaccine in the HCW.4 The vaccination campaign for the HCW began in late December 2020 and is still ongoing; most of it was completed during the first months of 2021. The recommended vaccination schedule for this vaccine is two doses at an interval of at least 21 days between doses. The reported overall efficacy in preventing infection in a phase 3 study was 91.6% and the reported seroconversion rate exceeded 95%.5 In the real world, the reported effectiveness in preventing death in people over the age of 60 years in a field study in Argentina was 93%.6 Seroconversion rates and the magnitude of the humoral response observed in some studies conducted in our country were high, particularly in those subjects with a prior diagnosis of COVID-19.7,8 However, the factors associated with a more pronounced humoral response have yet to be well characterised and are extremely important for providing evidence that would enhance active immunisation strategies in this population. In light of the above, it is critical to assess the rate of seroconversion and the magnitude of the humoral response in COVID-19 vaccinated HCW, as well as the variables associated with it.
ObjectivesTo evaluate the antibody response against SARS-CoV-2 in HCW with the full Sputnik V vaccine (“Gam-COVID-Vac”) schedule in a real-life setting.
To assess the relationship between antibody response against SARS-CoV-2 as it relates to the following variables: age, sex, presence of comorbidities, history of COVID-19, interval between doses, adverse events putatively attributable to vaccination and immunisation, and time between doses.
Materials and methodsThis is an observational, prospective study of the evaluation of the anti-SARS-CoV-2 humoral response in the HCW with a complete vaccination schedule in a hospital in the Autonomous City of Buenos Aires (April-July 2021). During this time frame, the virus was found to be circulating extensively, coinciding with the second wave of COVID-19 in Argentina.
Data collection
Participants were enrolled on a voluntary basis and without a pre-established schedule if they were fully vaccinated with Sputnik V vaccine and more than 4 weeks had elapsed since the second dose of vaccine. Participants who had COVID-19 between vaccination and serology sampling were excluded.
A self-administered questionnaire, accessible to participants in electronic format, was used to capture epidemiological and clinical information.
Determination of humoral response
The presence of antibodies against the SARS-CoV-2 Spike (S) protein in plasma was assayed by COVIDAR® IgG enzyme immunoassay. This technique identifies the antibodies present in the sample by means of a chromogenic substrate which produces a colour the intensity (optical density) of which is proportional to the concentration of the antibodies, thereby providing semi-quantitative results.9 The results were expressed as the ratio between the signal obtained (absorbance) and the cut-off point (S/Co). Bearing in mind that the measured absorbance is directly proportional to the concentration of the antibodies, the test was classified as positive if the S/Co was greater than 1. An S/Co ratio > 2 correlates with titres over 1:800. Furthermore, this serological technique is suitable for large-scale studies, in that it acts as a surrogate for viral neutralisation, with a correlation having been noted between the antibody levels detected and the degree of antibody neutralisation with titres > 1:200.10 An elevated antibody response was defined as an S/Co ratio greater than the median observed in the study population.
Statistical analysisCategorical variables were expressed as absolute and relative frequencies. Continuous variables were denoted by medians and interquartile ranges (IQR). Intergroup comparisons were carried out using the Mann Whitney U-test or the Kruskal-Wallis test for continuous variables or the Chi-square test (χ2) for categorical variables.
To explore the effect of the different independent factors of positive serology and elevated antibody response, a cross-sectional analysis was performed using a multivariate logistic regression model. Variables that can impact the serological response to vaccination were probed, including age (dichotomised as less than or greater than 60 years), sex (female or male), presence of comorbidities (dichotomised as “yes” or “no” according to the presence of any of the following comorbidities: hypertension, diabetes, chronic non-asthma lung disease, asthma, heart disease, obesity, chronic kidney disease, AIDS/HIV, solid neoplasm, immunosuppression) [sic], the presence of a history of COVID-19 (symptomatic or asymptomatic), the interval between vaccine doses (dichotomised as less than 4 weeks or equal to or greater than 4 weeks, as per the recommendation in place at the time when healthcare personnel were being vaccinated, which was to administer the doses at an interval of 21 days), presence of systemic reactogenicity (dichotomised as “yes” or “no”) on the basis of the occurrence of any of the following signs and/or symptoms: fever, chills, muscle ache, headache, diarrhoea, asthenia following the administration of any of the doses of the vaccine and the time span between the administration of the second dose and the serology being performed (dichotomised on the median value observed for this variable). A stepwise backward model selection was performed with a p-value of p = .05. Variables that had been proven in previous studies to be associated with serological response, such as age, history of COVID-19, and the interval between vaccination and serology, were also included in the model. Statistical analysis was performed using Epi Info (version 7.2) and GraphPad Prism (version 9.2.0).
ResultsA total of 630 HCW were enrolled. The median (IQR) age was 47 years (38-56); 462 (73%) were female, and 174 (28%) had at least one comorbidity. A history of COVID-19 was present in 158 (25%) of participants; 28 (18%) and 130 (82%) had experienced asymptomatic or symptomatic infection, respectively. The median time between vaccine doses was 3 (3-4) weeks. All in all, 371 (59%) subjects had systemic reactogenicity to the vaccine (first and/or second dose) — 305 (48%) to the first dose and 221 (35%) subjects to the second dose, with no significant difference between participants with or without prior SARS-CoV-2 infection (60 vs. 58%, p = 0.77). Likewise, among those subjects with a previous COVID-19 infection, there was no difference in the time to vaccination between those with and without systemic reactogenicity to the first dose (25 vs. 26 weeks, p = 0.79). Forty-eight percent of participants reported using analgesics to prevent reactogenicity. The median time from vaccination to serology sampling was 14 (11-17) weeks (Table 1).
Characteristics of 630 healthcare workers vaccinated with the full Sputnik V schedule
| Characteristics | n (%) |
|---|---|
| Female sex | 462 (73) |
| Age, median (IQR) | 47 (38-56) |
| Presence of comorbidities | 174 (28) |
| COVID-19 prior to vaccination | 158 (25) |
| Symptomatic/asymptomatic prior COVID-19 | 130 (21) / 28 (4) |
| Time between COVID-19 and first vaccine dose (weeks), median (IQR) | 25 (19-30) |
| Time interval between vaccine doses (weeks), median (IQR) | 3 (3-4) |
| Systemic vaccine reactogenicity | 371 (59%) |
| Time between full vaccine schedule and COVID-19 serology (weeks), median (IQR) | 14 (11-17) |
IQR: Interquartile Range.
There were 607 (96.35%) participants with reactive serology. There was no significant difference between those with and those without a pre-vaccination history of COVID-19. The median S/Co was 7.81. In participants without prior COVID-19, the median S/Co was 5.96 (2.85-11.36), while in those with asymptomatic prior COVID-19 it was 9.43 (6.36-17.3), p = 0.02, and in those with symptomatic prior COVID-19 15.93 (10.4-18.68), p = 0.0003. (Fig. 1).
Level of anti-SARS-CoV-2 antibodies detected in 630 healthcare workers vaccinated with 2 doses of Sputnik V with or without prior COVID-19. Ref. S/Co: ratio between the signal obtained (absorbance) and the cut-off point. The red line corresponds to the median. The dotted black lines correspond to the interquartile range.
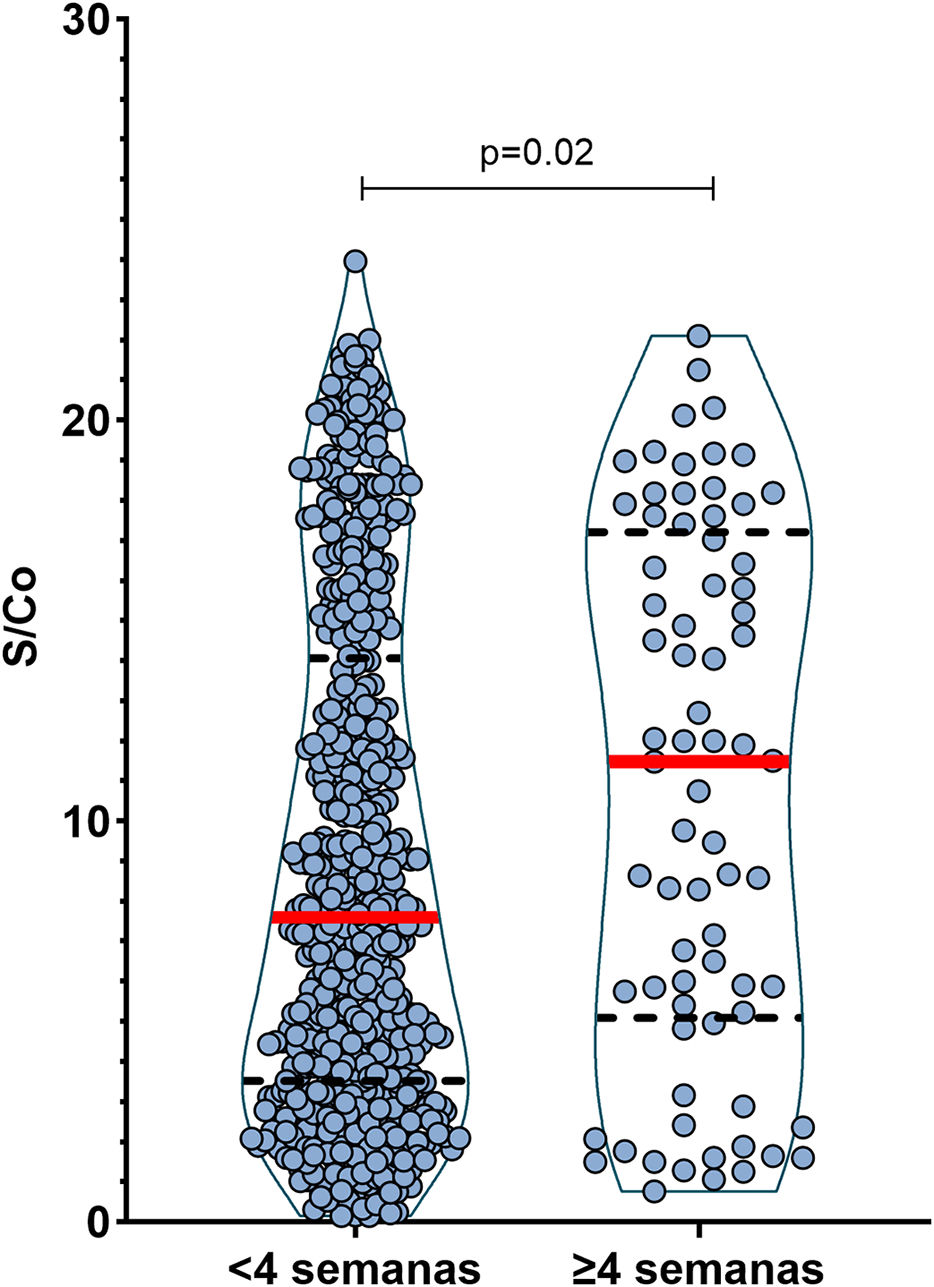
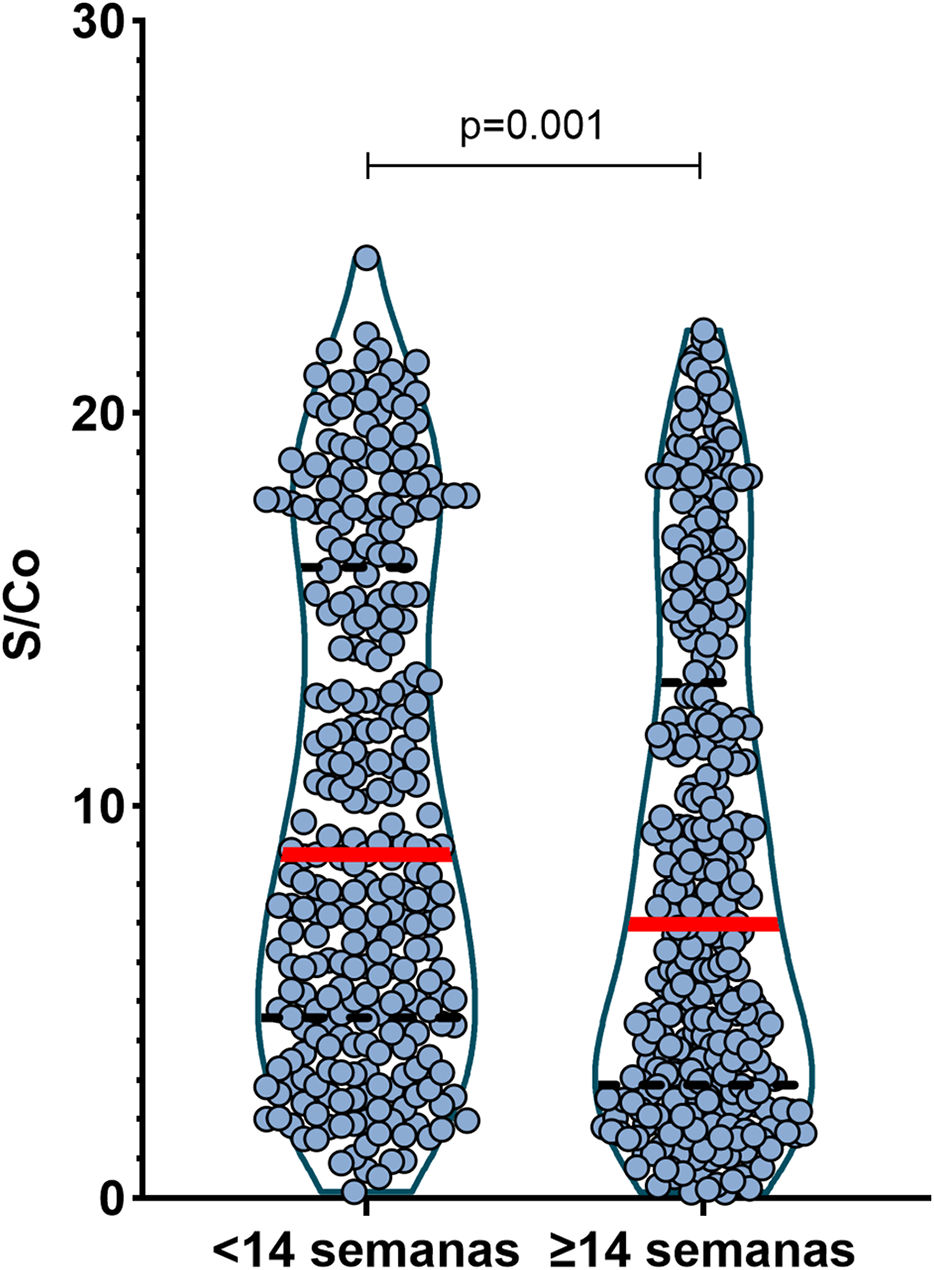
When evaluating the interval between vaccine doses, we observed a higher level of antibodies in those participants who had received both doses at an interval of more than 4 weeks. In these cases, the median S/Co was 11.48 (5.23-17.01) vs. 7.6 in those participants who had received both doses 3-4 weeks apart (3.52-14), p = 0.02 (Fig. 2). When the time from the second dose of vaccine until serology was determined, the median S/Co was 8.75 (4.61-16) vs. 6.98 (2.91-13.02) when 14 weeks or more had elapsed, p = 0.001 (Fig. 3), with no significant difference depending on whether or not the participants had a history of SARS-CoV-2 infection.
Anti-SARS-CoV-2 antibodies detected in 630 healthcare workers vaccinated with 2 doses of Sputnik V based on the interval between both doses of the vaccine. Ref. S/Co: ratio between the signal obtained (absorbance) and the cut-off point. The red line corresponds to the median. The dotted black lines correspond to the interquartile range.
Level of anti-SARS-CoV-2 antibodies detected in 630 healthcare workers vaccinated with 2 doses of Sputnik V by time to serology. Ref. S/Co: ratio between the signal obtained (absorbance) and the cut-off point. The red line corresponds to the median. The dotted black lines correspond to the interquartile range.
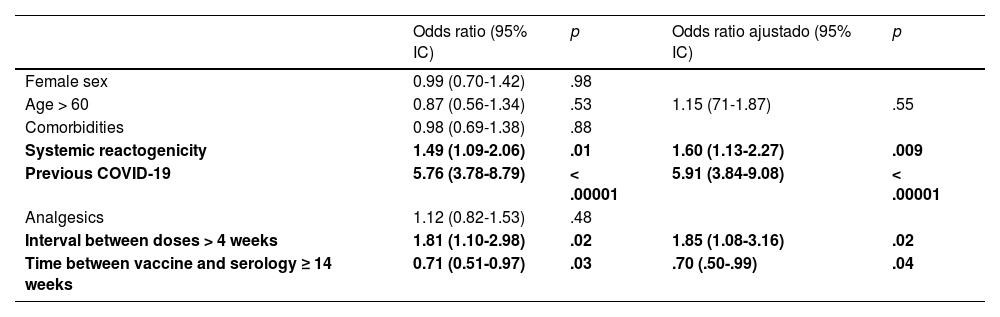
On multivariate analysis, the only factor that was independently associated with having a positive serology was a history of systemic reactogenicity. While the factors independently associated with an elevated antibody response (S/Co > 8) were a history of systemic reactogenicity, previous COVID-19, an inter-dose interval ≥ 4 weeks, as well as an interval between second dose and serology < 14 weeks (Tables 2 and 3).
Multivariate analysis of factors associated with the detection of anti-SARS-CoV-2 antibodies in 630 healthcare workers vaccinated with Sputnik Va
| Odds ratio (95% CI) | P | Adjusted odds ratio (95% CI) | p | |
|---|---|---|---|---|
| Female sex | 1.81 (.77 - 4.27) | .17 | ||
| Age > 60 | .49 (.19-1.28) | .15 | .58 (.21-1.60) | .29 |
| Comorbidities | .58 (.25-1.37) | .21 | ||
| Systemic reactogenicity | 2.79 (1.16-6.68) | .02 | 2.54 (1.03-6.26) | .04 |
| Previous COVID-19 | 3.62 (.84-15.61) | .08 | 3.20 (.73-13.94) | .12 |
| Analgesics | 1.46 (.62-3.43) | .38 | ||
| Interval between doses > 4 weeks | 2.96 (.39-22.24) | .29 | ||
| Time between vaccine and serology ≥ 14 weeks | .43 (.17-1.18) | .08 | .41 (.15-1.07) | .07 |
Multivariate analysis of factors associated with elevated anti-SARS-CoV-2 antibody response (S/Co > 8) in 630 health-care workers vaccinated with Sputnik V.a
| Odds ratio (95% IC) | p | Odds ratio ajustado (95% IC) | p | |
|---|---|---|---|---|
| Female sex | 0.99 (0.70-1.42) | .98 | ||
| Age > 60 | 0.87 (0.56-1.34) | .53 | 1.15 (71-1.87) | .55 |
| Comorbidities | 0.98 (0.69-1.38) | .88 | ||
| Systemic reactogenicity | 1.49 (1.09-2.06) | .01 | 1.60 (1.13-2.27) | .009 |
| Previous COVID-19 | 5.76 (3.78-8.79) | < .00001 | 5.91 (3.84-9.08) | < .00001 |
| Analgesics | 1.12 (0.82-1.53) | .48 | ||
| Interval between doses > 4 weeks | 1.81 (1.10-2.98) | .02 | 1.85 (1.08-3.16) | .02 |
| Time between vaccine and serology ≥ 14 weeks | 0.71 (0.51-0.97) | .03 | .70 (.50-.99) | .04 |
In this prospective, real-world study, we investigated the humoral response to the Sputnik V vaccine in more than 600 healthcare workers. This extensive and detailed analysis provides several significant findings that contribute to a better understanding of the immune response to vaccination against COVID-19.
First, the seropositivity rate observed in participants vaccinated with the full Sputnik V schedule exceeded 95%. This rate did not vary significantly by participants’ sex, age, previous exposure to SARS-CoV-2, interval between vaccine doses, and time to serology.
Second, we observed a significant humoral response, similar to that reported in earlier studies.5,7,8 Despite the fact that the optimal antibody titre for suitable virus neutralisation remains unknown, it has been noted that the greater the antibody titre, the greater the neutralising activity of the antibodies.10,11
Some of the factors investigated in our study were independently associated with higher antibody titres. Participants who had COVID-19 prior to vaccination, most notably those who were symptomatic, had almost 3 times more antibodies than those not previously exposed to the virus. This observation is similar to findings reported by several studies that have evaluated humoral responses to different vaccines.7,8,12 Even a single dose of vaccine in those subjects who had previously had COVID-19 generated the same or greater humoral response than in those having no prior diagnosis of COVID-19 and 2 doses of vaccine. Based on these results, we believe that, when faced with low vaccine availability, a single dose in people previously diagnosed with COVID-19 would be indicated, and in the reverse scenario, a third dose in individuals without a history of COVID-19 would be recommended.
More than half of the participants reported signs or symptoms of systemic reactogenicity. This is similar to what was observed in the development stage of the Sputnik V vaccine and in a surveillance study conducted in a hospital in Argentina.5,13 Some studies involving mRNA vaccines found a higher prevalence of systemic reactogenicity in subjects with a history of exposure to SARS-CoV-2.14 In our study, we did not find a history of COVID-19 or time to vaccination to be associated with an increased risk of systemic reactogenicity. While the reactogenicity of a vaccine represents the physical manifestation of the inflammatory response to the vaccine antigen, it is unclear whether stronger reactogenicity leads to a more intense immune response.15 The information available with respect to this subject with COVID-19 vaccines is very limited. In our study, the presence of reactogenicity to the Sputnik V vaccine was associated with an increased level of antibody production. This same observation was also reported in a study that examined messenger RNA-based vaccines.16 In contrast, another recently published study revealed no association between reactogenicity and humoral response with the ChAdOx1 (AstraZeneca) and BNT162b2 (Pfizer-BioNTech) vaccines.17 To the best of our knowledge, the association found in our case series has not been previously reported for the Sputnik V vaccine. However, more specifically designed studies are needed to confirm this observation.
It is well known that as time passes since vaccination, the level of protection conferred by a vaccine can wane. COVID-19 vaccines would be no exception.18,19 While no longitudinal follow-up of participants' serology was carried out in our study, we noted that the participants with more than 14 weeks since vaccination had lower levels of antibodies. This was especially true for those subjects with no prior SARS-CoV-2 infection. It is important to clarify that the level of IgG antibody immune response against the Spike protein is not the only correlate of protection. The neutralising capacity of these antibodies and the cellular immune response must also be assessed.
Most of the HCW included in our study received the 2 doses of Sputnik V vaccine with a 3-week interval, as initially recommended by the Argentinean health authorities.4 When analysing the influence of the vaccine dose interval on the humoral response, we observed a higher level of antibodies in those participants who received the second dose four weeks or more later. These results are in line with those observed for the ChAdOx1 vaccine (AstraZeneca), where greater immunogenicity and efficacy was observed if the second dose was administered after 3 months and not at 21 days.20 This would suggest that it is the time interval and not the vaccine dose that has the strongest impact on the vaccine's immunogenicity. Similar results were obtained for other vaccines, such as influenza and Ebola.21 The Gamaleya Institute (Russia) and the health authorities in Argentina have recently recommended prolonging the interval for the second dose of the Sputnik V vaccine to 90 days.22 At present, no publication has assessed the level of antibodies as related to the dosing interval of the vaccine.
Finally, it must be remembered that the effectiveness of a vaccine does not depend solely on humoral response. There are other immune mechanisms at play, such as the innate response, CD4+ or CD8+ T-cell response, B-cell memory response, among others.23 Therefore, it has yet established whether the level of anti-SARS-CoV-2 antibodies generated by the vaccine correlates with the degree of effectiveness of the vaccine. Nevertheless, recent observations suggest that antibody-mediated immunity would be the primary mechanism to protect against infection by SARS-CoV-2 and its respective variants.24 Moreover, there is growing evidence that those with higher post-vaccination antibody titres would have a lower risk of symptomatic SARS-CoV-2 infection, and lower infectivity (viral load) in the event of infection.20,25–28
Our study has certain notable limitations. First, the neutralising activity of the antibodies detected in the participants could not be titrated and assessed. However, the results obtained with the serological technique used expressed as S/Co show a strong correlation, on the one hand, with the titration of the antibodies and, on the other hand, with the neutralising activity of the antibodies. Furthermore, the results obtained in our study resemble other studies using quantitative techniques.7,8 Second, baseline serology was not performed at the time of vaccination to detect previously undiagnosed cases of COVID-19. However, the HCW at our centre routinely performed rapid serological tests and nasopharyngeal swabs whenever there was a risk exposure with a case of COVID-19. We therefore believe that the likelihood of a healthcare worker having had a previously undiagnosed asymptomatic SARS-CoV-2 infection is low. Third, there was no longitudinal follow-up of participants, making it impossible to assess the persistence of antibodies over time, and few samples were examined with more than 14 weeks post second dose to serological testing.
Finally, the humoral response was not measured on the basis of a pre-established schedule, but was performed on a voluntary basis among the participants. Therefore, both the baseline characteristics of the participants and the time interval between vaccination and sample collection are not identical. These characteristics mean that this study yields valuable data from a real-world setting.
It is important to remember that the best way to assess the protection of vaccines against COVID-19 is to accompany a study assessing the immune response of subjects with a real-world effectiveness study.
ConclusionsThe present work reports highly relevant data regarding humoral response and the variables associated with it in HCW vaccinated against COVID-19. These initial data may contribute to the development of future immunisation strategies in one of the populations most exposed to this disease.
Please cite this article as: Cordova Ezequiel, Lespada M Ines, Cecchini Diego, Nieto Fabiola, Palonski Susana, Badran Mariana, et al. Evaluación de la respuesta de anticuerpos igg específicos contra SARS-CoV-2 en personal de salud con esquema completo de vacuna Sputnik V (GAM-COVID-VAC). Vacunas. 2022. https://doi.org/10.1016/j.vacun.2022.01.008