Functional assessment, and function-based treatments, are the gold standard for the treatment of problem behavior. Historically, these assessment and treatment evaluations have been conducted in austere clinical settings to increase internal validity. While prioritizing internal validity is critical in the initial stages of a treatment evaluation, if there is not an eventual shift to prioritizing the external or social validity of the treatment it may inevitably fail in the natural environment. The purpose of this case example is to outline a socially valid approach to the assessment and treatment of problem behavior that ensures individuals’ and their families’ lives benefit in meaningful ways. More specifically, this case-example will outline a method of prioritizing social validity to identify treatment goals, conduct functional analysis, evaluate and generalize treatment, and implement caregiver training.
La evaluación funcional y los tratamientos funcionales son el estándar de oro para el tratamiento de la conducta problemática. Históricamente, esas evaluaciones y tratamientos se han conducido en escenarios clínicos austeros para aumentar la validez interna. Si bien el priorizar la validez interna es crítico en las etapas iniciales de la evaluación de un tratamiento, si eventualmente no hay un cambio para priorizar la validez externa o social del tratamiento, éste puede fallar en un escenario natural. El propósito del ejemplo de caso que se presenta en este trabajo es mostrar una aproximación válida para la evaluación y tratamiento de conducta problemática que asegura que las vidas de los individuos y de sus familias se beneficien de forma significativa. Más específicamente, el ejemplo de caso que se presenta mostrará un método para identificar las metas del tratamiento priorizando la validez social, para conducir un análisis funcional, evaluar y generalizar el tratamiento y entrenar al cuidador.
Compared to typically developing peers, children with developmental or intellectual disabilities are at an increased risk for engaging in problem behaviors such as aggression, self-injury, property destruction, and pica (Dekker, Koot, van der Ende, & Verhulst, 2002). Estimates of the prevalence of such problem behaviors in this population vary widely, from between 10-15% (Emerson et al., 2001) to as many as 73% of individuals (Rojahn, Matson, Lott, Esbensen, & Smalls, 2001). However, what is unequivocal is that the presence of problem behaviors such as these is associated with negative outcomes for both the child engaging in the behavior and their caregivers. For example, self-injurious behaviors like head-banging, hitting/biting oneself, or skin picking can cause permanent tissue damage or permanent loss of sight or hearing, as well as increase the risk of secondary harm from infections (Minshawi et al., 2014). Wandering or running away (i.e., elopement) puts these children at risk for abduction, injury, or even death due to drowning or being struck by an automobile (Anderson et al., 2012). Such behaviors also frequently result in children being placed in more restrictive educational settings. As a result they benefit less from general educational instruction and spend less time with typically developing peers (Gresham et al., 2004). Similarly, problem behavior can require the child to be placed in restrictive residential settings, further limiting their access to important social and community interactions and supports (Friedman, Kalichman, & Council on Children with Disabilities, 2014).
Problem behaviors such as these also have profound negative effects for caregivers. Research has shown a strong correlation between having a child with problem behavior and an increased level of parental stress (Dykens, 2000; Neece, Green, & Baker, 2012) and poorer overall family functioning (Davis & Gavidia-Payne, 2009). In fact, the presence of problem behavior is more predictive of parental stress than deficits in adaptive behavior or the severity of the symptoms of the developmental disability itself (Baker, Blacher, Crnic, & Edelbrock, 2002; Estes et al., 2013; Hastings & Beck, 2004; Lecavalier, Leone, & Wiltz, 2006). Behavior problems have also been found to negatively impact marital satisfaction (Hartley, Barker, Baker, Seltzer, & Greenberg, 2012), are correlated with higher rates of problem behavior in siblings (Hastings & Beck, 2004), and parents of children with disabilities who engage in problem behavior find it harder to maintain employment (Hall, Bouldin, Andresen, & Ali, 2012). Moreover, caregivers who experience high levels of stress are less able to implement interventions for their child’s problem behavior (Osbourne, McHugh, Saunders, & Reed, 2008). Thus, well-designed interventions for problem behaviors exhibited by children with developmental disabilities have the potential to produce significant benefit not only for the child but for their caregivers as well.
Effective treatments of problem behavior in this population have historically been based upon the scientific approach to the study of behavior known as behavior analysis. Within this literature, problem behavior was hypothesized by Ferster (1961) to be learned and therefore under the control of its environmental consequences. Some of the first researchers to apply this approach to the treatment of problem behavior began evaluating the effectiveness of behavior analytic principles (e.g., reinforcement, extinction, punishment, etc.) for the reduction of self-injurious behavior. Early evidence revealed that behavior analytic approaches could effectively reduce the self-injurious behavior of individuals with developmental and intellectual disabilities (Corte, Wolf, & Locke, 1971; Lovaas & Simmons, 1969). However, these researchers noted that not all self-injurious behaviors were responsive to the same strategies. For some individuals self-injurious behavior decreased only when other non-self-injurious behavior(s) were reinforced (Corte et al., 1971). For others, self-injurious behavior decreased only when punishment was implemented contingent upon self-injurious behavior (Corte et al., 1971; Lovaas & Simmons, 1969). Still others only showed improvements when all forms of positive reinforcement were restricted following episodes of self-injurious behavior (Corte et al., 1971; Lovaas & Simmons, 1969). Carr (1977) summarized much of the research on the treatment of self-injurious behavior at the time and hypothesized that the behaviors could be maintained by extrinsic (e.g., socially mediated) or intrinsic (e.g., automatic) forms of reinforcement. For example, when attention from a caregiver is a sufficiently potent form of positive reinforcement, the child may learn that self-injury is likely to produce attention from caregivers in the form of reprimands, soothing statements, etc. Carr (1977) also suggested that treatments might not be effective at reducing self-injurious behavior if they are not correctly matched to the type of consequences maintaining the self-injury (i.e., its function). In the example above, restricting attention following self-injurious behavior is likely to produce a gradual reduction due to extinction. However, for a child for whom removal of demands serves as a negative reinforcer that maintains self-injury, restricting attention is unlikely to have a reductive effect. Thus, Carr (1977) raised the possibility that an assessment of function could be integral as a guide for selecting treatments for self-injurious behavior.
Although other researchers had developed methods for evaluating whether a particular type of reinforcer maintained an individual’s self-injury (e.g., Carr, Newsom, & Binkoff, 1976), Iwata, Dorsey, Slifer, Bauman, & Richman, (1982/1994) were the first to develop a methodology that systematically evaluated several of the most likely functions within a single analysis. Three test conditions, each of which was designed to evaluate a different hypothesis about function, and one control condition were conducted with nine participants. The attention condition served as an analog for those situations in which a caregiver might deliver attention, such as a reprimand, in response to self-injury. As such, it assessed whether self-injury was maintained by social-positive reinforcement in the form of attention. The escape condition served as an analog for situations in which a caregiver discontinues tasks in an effort to stop their child’s self-injury. Thus, this condition assessed whether self-injury was maintained by social-negative reinforcement in the form of escape from demands. The alone condition assessed whether self-injury was maintained by automatic reinforcement. That is, if problem behavior produced some intrinsic reinforcement, such as sensory stimulation, it would be expected to be insensitive to social consequences and persist even when the child was alone in a relatively austere environment. Finally, the toy play condition served as a control for the attention and escape test conditions because problem behavior maintained by social reinforcement would not be expected to occur in the absence of demands and free access to attention. For six of the nine participants, self-injurious behavior occurred at high rates during only one of the test conditions, and treatments based upon results of these functional analyses (FAs) effectively reduced self-injurious behavior. These results provided support to the theories of Ferster (1961) and Carr (1977) that self-injurious behavior likely served specific behavioral function(s) and that function was a key variable in the development of effective treatments.
Since the seminal study by Iwata et al. (1982/1994), FA methodology has been extended to a wide range of problem behaviors, including (but not limited to) aggression (e.g., Baker, Hanley, & Mathews, 2006), pica (e.g., Piazza, Hanley, & Fisher, 1996), elopement (e.g., Piazza et al., 1997), stereotypy (e.g., Mace, Browder, & Lin, 1987), noncompliance (e.g., Reimers et al., 1993; Rodriguez, Thompson, & Baynham, 2013; Wilder, Harris, Reagan, & Rasey, 2007), tantrums, (e.g., Vollmer, Northup, Ringdahl, LeBlanc, & Chauvin, 1996), property destruction (e.g., Fisher, Lindauer, Alterson, & Thompson, 1998), disruptive behavior (e.g., Broussard & Northup, 1995, 1997), and inappropriate sexual behavior (e.g., Fyffe, Kahng, Fittro, & Russel, 2004). Functional analysis of severe problem behavior continues to be widely implemented, and research has continued to expand and adapt the Iwata et al. (1982/1994) methodology. The original methods have also been adapted to evaluate a wide range of additional types of reinforcers, including access to preferred edible or leisure items (e.g., Hagopian, Fisher, Thibault Sullivan, Acquisto, & LeBlanc, 1998), avoidance of social interactions (e.g., Hagopian, Wilson, & Wilder, 2001) and avoidance of transitions (e.g., McCord, Thomson, & Iwata, 2001), to name just a few.
Functional analysis test conditions are designed to evaluate the effects of antecedent and consequence variables, while controlling for extraneous variables present in the environment that make it difficult to identify the function of problem behaviors in less controlled circumstances. Thus, great care is often exerted to ensure such potential confounds are eliminated. It is perhaps not surprising then that reviews of the literature on FAs show that the majority of the assessments are conducted in hospital or institutional settings where significant resources can be allocated (Beavers, Iwata, & Lerman, 2013; Hanley, Iwata, & McCord, 2003). Within these settings, FAs are frequently conducted in specialized session rooms that are devoid of any materials not directly related to the variables being evaluated. Although these analog settings allow for extremely controlled and precise FAs, a disadvantage is that they may not be representative of the natural environment in which the problem behavior occurs. This limitation can be problematic when implementing and evaluating function-based treatments because the goal of most treatments is to reduce problem behavior in the individual’s natural environment.
A review of behavioral interventions revealed that function-based treatments based on a FA resulted in significantly better outcomes compared to treatments that were not based on a FA (Campbell, 2003; Heyvaert, Saenen, Campbell, Maes, & Onghena, 2014). However, many of the studies summarized in that review limit their outcomes to demonstrations that problem behavior improved in those same well-controlled settings in which the FA was conducted. In contrast, it is important for clinicians to not only consider whether a particular treatment approach holds the possibility of achieving a positive outcome, but whether treatment and outcome are socially valid (i.e., acceptable to the individual, their caregivers, and society; Wolf, 1978). It can be argued that function-based treatments possess some social validity by their very nature because they provide an opportunity for the individual to continue to access reinforcement that is meaningful to them. Conversely, even if a non-function-based treatment effectively reduces problem behavior it will still possess less social validity if the individual is no longer able to access the reinforcer(s) that previously maintained their problem behavior. Thus, it is not surprising that there is evidence that individuals who engage in problem behavior prefer function-based treatments to those that are not based upon the results of a FA (Hanley, Piazza, Fisher, Contrucci, & Maglieri, 1997). However, access to reinforcement is only one component of effective treatments for problem behavior that clinicians and researchers must consider to maximize social validity of treatments for problem behavior.
Designing function-based treatments that are socially valid also requires striking the appropriate balance between internal and external validity. Maximizing internal validity through the use of highly controlled sessions and specialized rooms allows for causal statements to be made regarding the function of problem behavior and any decrease observed as a result of treatment. However, emphasizing such approaches while neglecting the importance of evaluating treatment effectiveness in more naturalistic environments (i.e., external validity) can limit the chances of long-term positive outcomes. On the other hand, emphasizing external validity by conducting sessions in a less controlled manner and more naturalistic conditions can make treatment effects more likely to generalize to the natural environment, but conclusions regarding the active components of behavior change may not be definitive. Therefore, a socially valid treatment plan begins by prioritizing internal validity during the initial treatment evaluation, with a shift towards prioritizing external validity once the treatment has already been shown effective. However, historically there has been less emphasis in the literature on the inclusion of naturalistic stimuli in analog sessions or the modification of treatment components to replicate more naturally existing contingencies.
One way to enhance the probability that treatments will strike the appropriate balance between internal and external validity is to focus attention on the manner in which treatment goals are established. Frequently treatment goals are limited to a description of a desired reduction in targeted problem behaviors. However, such an approach to setting goals is structural rather than functional: this type of treatment goal merely states that the treatment will result in some degree of behavior reduction but does not specify the desired benefit for the individual or caregivers. In contrast, consideration of context or function in establishing goals for treatment is more likely to ensure clinicians develop treatments that will actually address caregivers’ concerns. For example, if a treatment goal states only that “aggression will be reduced by 80%”, clinicians may be prone to determining that treatment has been successful even if aggression has only been reduced within the tightly controlled circumstances of a session room. In contrast, describing the treatment goal as “reduce aggression by 80% when the child is working on difficult demands at school”, compels clinicians to incorporate academic tasks into the FA and treatment analysis, and also increases the probability of evaluating the generalization of treatment to academic settings.
Although there is ample evidence that treatments for problem behavior that are based upon results of an FA can produce significant improvements, there is little published data to show maintenance of treatment effects in the natural environment. A review of behavioral treatments in the research literature reported that only 27.4% of studies attempted to generalize treatment to a new setting or situation (Campbell, 2003). This finding suggests that treatments are commonly evaluated within a single environment, most likely those well-controlled environments in which treatments are typically first developed. This treatment approach raises concerns regarding the maintenance of treatment gains in less structured situations that are inevitable in the natural environment.
Although social validity has not always been emphasized in the literature on function-based treatment of problem behavior, the purpose of the current case study is to outline a socially valid approach to function based treatment of severe problem behavior exhibited by individuals with developmental disorders. More specifically the current case study describes how social validity can guide goal development, behavioral assessment, treatment implementation, and generalization.
MethodParticipant and SettingAt the time of treatment, Stephany was a twelve-year-old female with Autism Spectrum Disorder and obesity. She communicated using single words and required moderate assistance with daily living tasks such as getting dressed. Stephany was referred to an intensive day treatment clinic for treatment of aggression, disruption, self-injurious behavior, spitting, and pica. During the months leading up to her admission, Stephany regularly punched holes in the walls of her home and had broken several windows. Her mother expressed concerns that they would be evicted from their apartment if the landlord became aware of the damage caused by Stephany’s problem behavior. Her mother also reported that several respite workers hired to assist in caring for Stephany had quit due to her problem behavior. Her mother reported that Stephany most commonly engaged in problem behavior in a few situations: when preferred food was restricted, at doctor’s appointments, or if item(s) in her home were rearranged and Stephany was prevented from returning them to their original location. Therefore, Stephany’s mother no longer allowed certain preferred foods in their home and avoided restricting food. As a result of having provided relatively free access to food, Stephany had gained a significant amount of weight, which in turn made it harder for others to physically manage her problem behavior. Stephany’s problem behavior at doctor’s appointments had resulted in her not receiving necessary medical care for over two years. Lastly, prior to Stephany’s admission to the day treatment program, her mother was seeking out an alternate residential placement. At the time of the initial admission meeting, the clinician worked with Stephany’s mother to identify several treatment goals that, if achieved, would most improve her and Stephany’s lives. Stephany’s treatment goals were to tolerate a) her morning routine (i.e., awaking, bathing, brushing her teeth, dressing, and eating breakfast); b) the restriction of food and limited meal portions; c) routine doctor’s appointment; and d) community outings without engaging in problem behavior.
The first day of Stephany’s admission was spent in her home in which therapists took a tour, observed Stephany and her mother in their daily routine, and instructed Stephany’s mother to replicate those situations that she had reported typically resulted in problem behavior. Following the home visit, Stephany began attending the day treatment program for six hours per day, five days a week. Assessment and treatment sessions were initially conducted by therapists in a padded session room with video cameras and a one-way mirror separating an adjoining observation room. Because this setting allowed for strict control over variables hypothesized to evoke or maintain problem behavior, it also maximized internal validity. External validity was emphasized once an effective treatment had been identified, by conducting sessions in more naturalistic settings around the treatment facility (e.g., playroom, classroom, waiting area near a physician’s office), and finally in Stephany’s home and school.
MeasurementWhen attempting to strike the right balance between internal and external validity, it is important to establish a rigorous data collection system. For Stephany, data were collected separately for each topography of her problem behavior. Aggression was defined as any instance or attempt to hit, kick, head-butt, scratch, bite, push, choke, pull hair, or throw an object at another person. Each of these behaviors was operationally defined in great detail for data collection purposes. For example, pushing was defined as any instance in which Stephany’s hand(s) contacted another person and applied force that altered the original standing position of that person. Other topographies of problem behavior that were similarly defined included disruption, which included throwing, hitting, or destroying objects; self-injurious behavior, which included head-banging and self-scratching; pica and spitting. Data were collected on customized data collection software via laptop computers during the FA. During stages of the treatment evaluation that were conducted in more naturalistic settings, data were collected via paper and pencil.
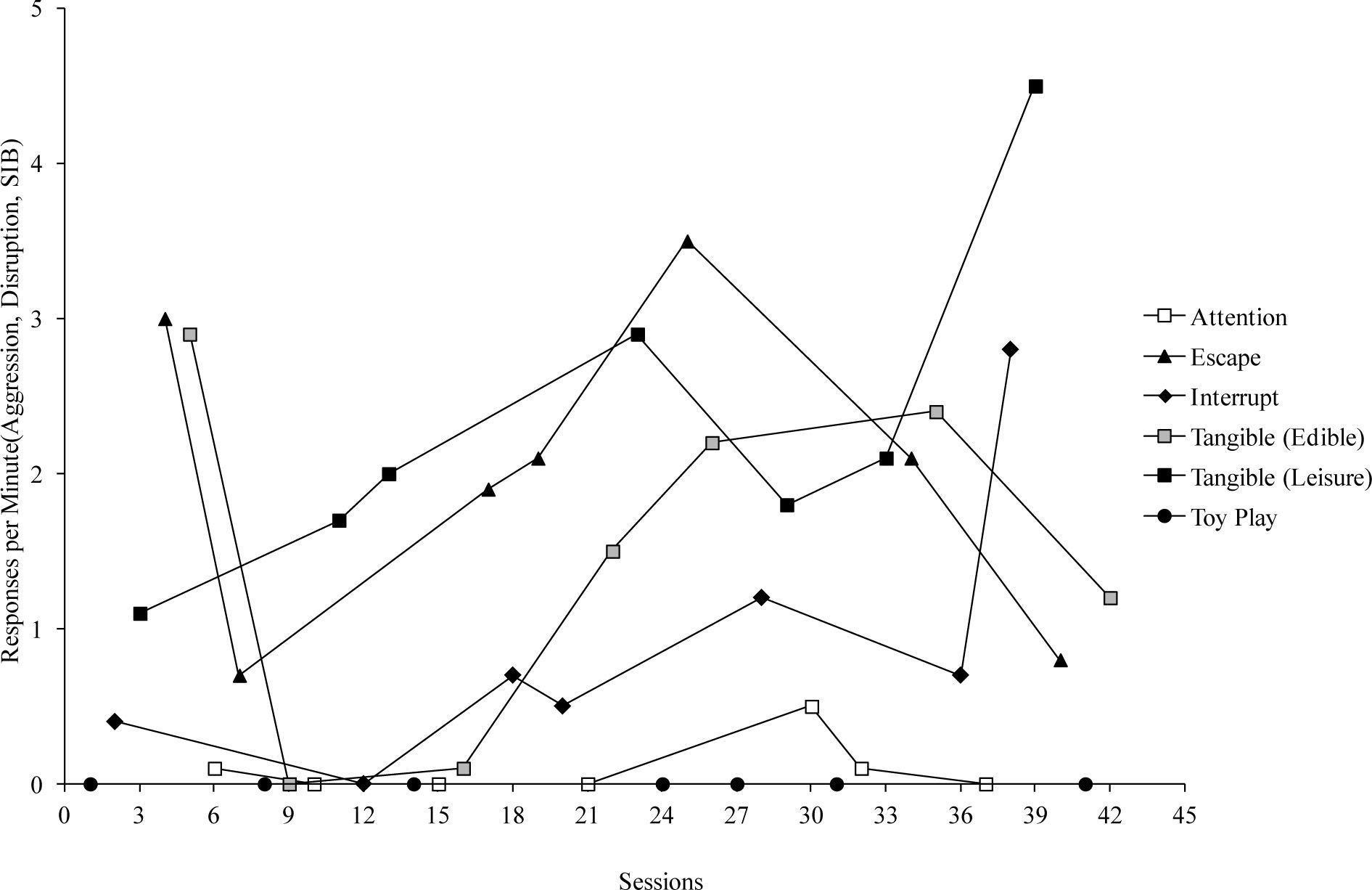
Functional AnalysisPrior to conducting the FA, it was important to empirically identify stimuli that were most likely to exert some influence over Stephany’s problem behavior. However, rather than select items or demands arbitrarily, as is commonly done, these were initially identified based on home/school observations and interviews with her mother. As has become customary, the items identified via home/school observation and caregiver report were included in a paired-stimulus preference assessment (Fisher et al., 1992) to identify a hierarchy of preference for edible and leisure items. Similarly, a demand assessment (Call, Pabico, & Lomas, 2009) identified demands that were likely to be aversive for Stephany. Results of these two assessments were used to select leisure and/or edible items for inclusion in toy play, attention, and tangible conditions, as well as demands to be included in the escape condition.
A modified FA based on the procedures described by Iwata et al. (1982/1994) was conducted using a variety of conditions, each of which were conducted in repeated 10min sessions. During sessions of the Toy play condition Stephany was provided with continuous access to a highly preferred leisure items (i.e., Legos™ and Playdoh™) and edible item (i.e., chips or fruit snacks). The therapist provided attention no less than every 30 s, refrained from touching any of Stephany’s leisure or edible items, and did not make any requests or place demands on her. There were no scheduled consequences for problem behavior during these sessions. The purpose of the toy play condition was to serve as a control for the test conditions.
Prior to the start of the Tangible (leisure) condition, Stephany was given 2minutes continuous access to the highly preferred leisure items. Once the session began, the therapist restricted access to the items but provided 30 s access contingent upon problem behavior. Following the 30 s reinforcement interval, the therapist again restricted access to the item. No attention or demands were delivered during these sessions.
Prior to conducting the Attention condition, the therapist provided Stephany with 2minutes of continuous high-quality attention. Once session began, the therapist restricted their attention by telling Stephany they had to do some work. Stephany had continuous access to an item identified as low preferred in the prior preference assessment (bubbles). Contingent upon problem behavior the therapist delivered a brief verbal reprimand.
During the Escape condition, the therapist repeatedly prompted Stephany to complete the task identified in the prior demand assessment (a number identification task) using a 3-step progressive prompting procedure: the therapist first delivered a verbal prompt to complete the task and allowed 3-5 s for compliance. If Stephany did not comply with the task, the therapist provided a model prompt. If Stephany did not comply within 3-5 s following the model prompt, the therapist physically guided the correct response. Contingent upon problem behavior, the therapist provided a 30 s break from the demand and removed all the demand materials from the table. No additional attention was provided beyond prompting the completion of the demands.
Based on caregiver reports, and observations conducted in Stephany’s home and school, two additional test conditions were included in the FA. The purpose of these conditions was to evaluate additional hypotheses regarding possible antecedent and consequence variables evoking and maintaining Stephany’s problem behavior. That is, Stephany’s problem behavior was hypothesized to be maintained by access to food and by terminating or avoiding the interruption or manipulation of items in her environment. Again, the addition of these conditions enhanced the external and social validity of the FA by evaluating hypotheses about potential individualized reinforcers that were maintaining her problem behavior.
Prior to the start of sessions from the Tangible (edible) condition, Stephany was allowed to choose between several preferred edible items. Once Stephany selected an edible item, she had 2minutes of continuous access to the item. Tangible (edible) sessions were identical to those in the Tangible (leisure) condition with the exception that the edible item she had selected prior to session was restricted and delivered contingent upon problem behavior.
Prior to the Interruption condition, Stephany received 2minutes of access to the preferred leisure items during which the therapist did not interact with the items. Once the session began, the therapist manipulated Stephany’s leisure items every 5 s (e.g., rearranged the Legos™). Contingent upon problem behavior, the therapist refrained from manipulating or touching the leisure items for 30 s. During the interruption sessions, the therapist provided Stephany with continuous attention even when they were not manipulating her leisure items.
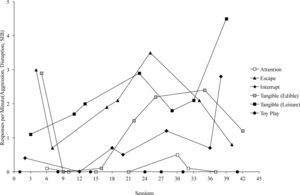
ResultsFigure 1 depicts the results of the FA. Stephany consistently engaged in high rates of problem behavior during the Tangible (leisure), Tangible (edible), Interrupt, and Escape conditions compared to the Attention or Toyplay conditions. This differentiation between the rates of problem behavior in the control (i.e., Toyplay) and specific test conditions indicated that her problem behavior served multiple functions, including access to social-positive reinforcement (in the form of preferred leisure and edible items) and social-negative reinforcement (in the form of escape from demands and escape from others manipulating the items with which she was engaged).
Treatment EvaluationThe clinical team used the results from Stephany’s FA, in combination with her caregiver’s goals, to design an intervention in which problem behavior was replaced with appropriate communicative behavior. Stephany’s mother conveyed being able to restrict access to edible items was her highest priority. The initial treatment package was then modified to address subsequent treatment goals such as requiring Stephany to tolerate her morning routine tasks, academic work, leisure activities and the manipulation of items in her environment. All of these permutations of the treatment were made within the context of restricting Stephany’s access to preferred edible items.
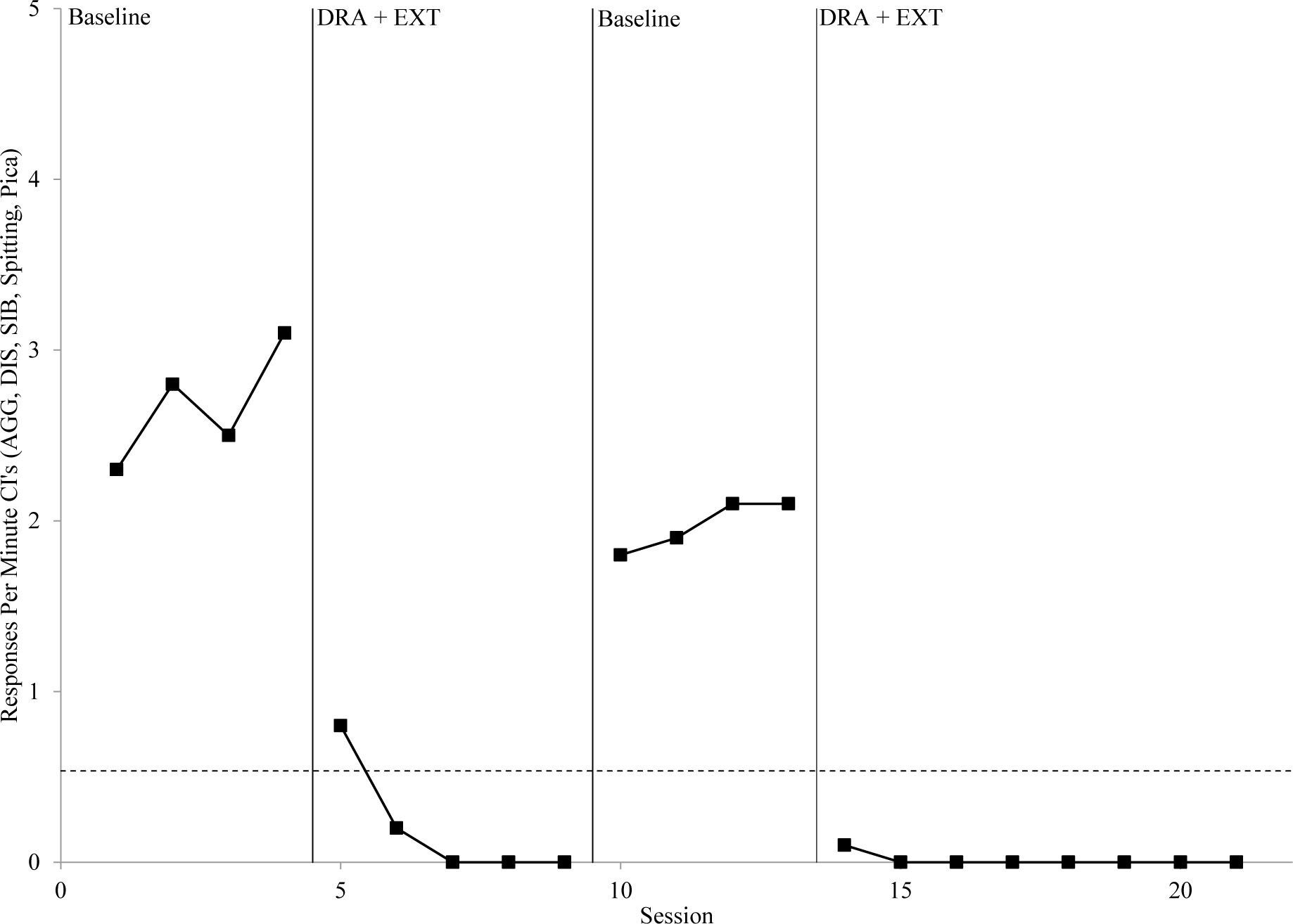
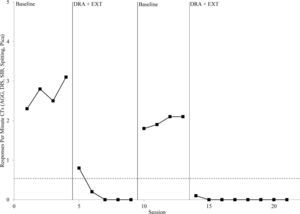
Functional Communication TrainingStephany was taught a vocal request for each of her preferred edible items using a progressive time delay prompting procedure (Charlop, Schreibman, & Garrison Thibodeau, 1985). Contingent upon mastery criteria for all vocal requests, a Differential Reinforcement for Alternative Behavior (DRA) intervention was evaluated. During these sessions, Stephany’s requests were reinforced with 30 s access to an edible item, and all problem behavior was placed on EXT. A reversal design compared rates of problem behavior under DRA, and baseline conditions that replicated the Tangible (Edible) condition of the FA (see Figure 2). Stephany’s problem behavior was eliminated within three sessions of the DRA treatment.
Treatment EvaluationAs described above, the results of treatments for problem behavior reported in the literature generally reflect the effects of interventions conducted in well controlled environments. In essence, this is what Stephany’s treatment had achieved to this point. However, it was not yet a socially valid treatment that would achieve the goals established by her mother. That is, it was not reasonable to expect that Stephany’s mother would be able to reinforce every appropriate request for preferred edible items. In addition, due to health concerns regarding Stephany’s weight, her mother had established a goal to restrict all access to food during certain periods of the day. Therefore, the clinical team designed a treatment in which there were periods of time during which Stephany could appropriately request food, but there were also periods during which food was unavailable even if she appropriately requested. This treatment has been conceptualized as a multiple schedule (Fisher, Kuhn, & Thompson, 1998; Hanley, Iwata, & Thompson, 2001), with the aim of bringing requests under the control of discrete stimuli.
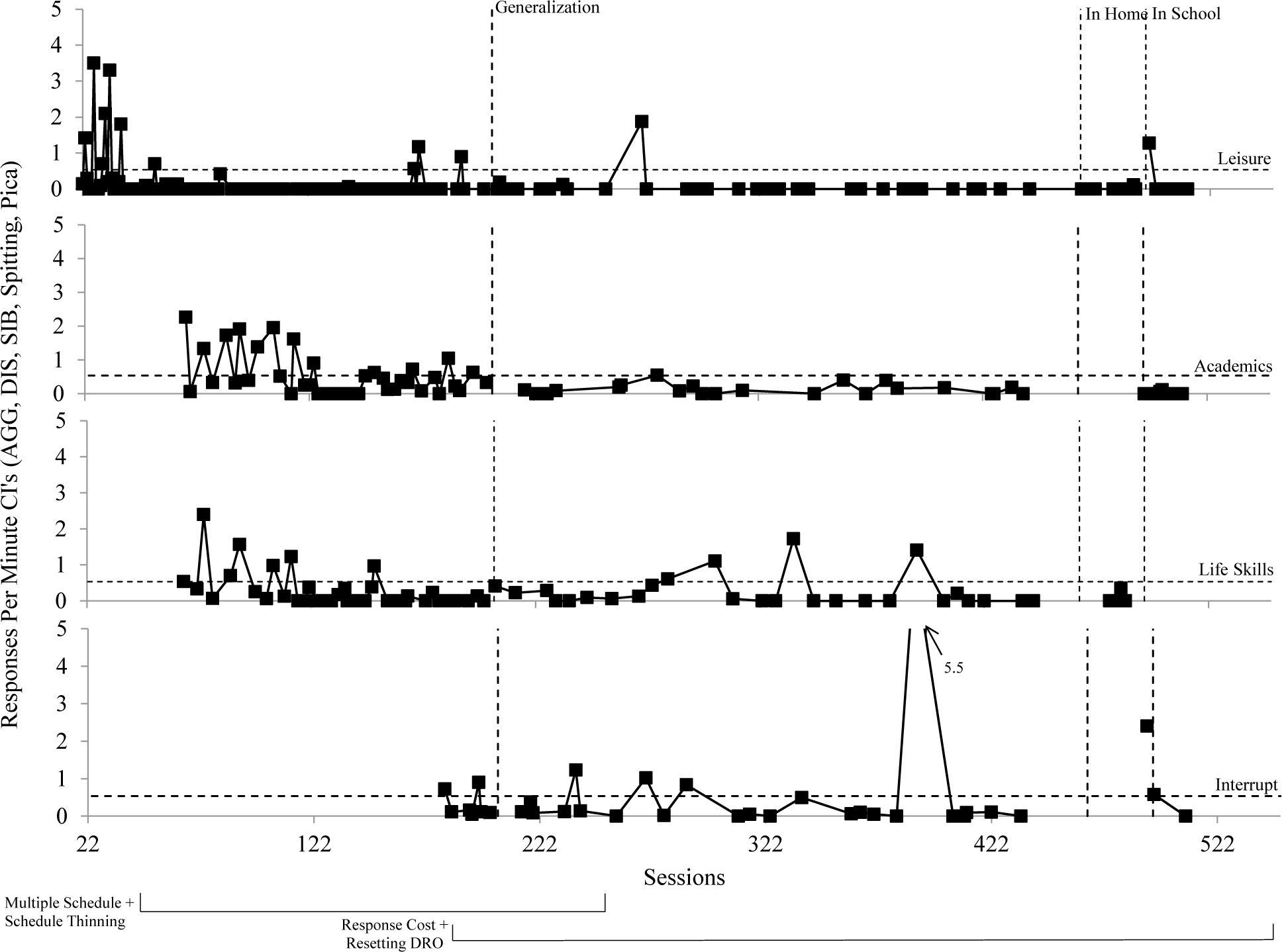
During the multiple schedule treatment, a yellow card signaled to Stephany when appropriate requests would be reinforced, whereas a purple card signaled when appropriate requests would not be reinforced. Initially the yellow card interval was set at 45 seconds, whereas the purple card interval was set at 15 seconds. Within sessions, the therapist rotated between the yellow and purple card intervals. Therefore, within one session, Stephany experienced periods of time in which a therapist reinforced her requests for preferred edible items and periods of time in which her preferred edible items were unavailable, even if she appropriately requested them. Following the introduction of treatment there was an initial increase in problem behavior, however three consecutive sessions without problem behavior were established within 21 sessions (see Figure 3).
To further increase the social validity of the treatment, and accomplish the treatment goal of being able to restrict Stephany’s access to food throughout the day, it was critical to increase the duration of the purple card interval during which edible items were unavailable. Therefore, the purple card interval was gradually increased from 15 s to the terminal goal of 15min. Once the terminal goal had been achieved, the treatment protocol was adapted to address the additional situations Stephany’s mother had identified as treatment goals. For example, the treatment was modified to address times in which Stephany was required to complete her morning routine, daily living tasks, academic tasks, leisure time with family, and to allow Stephany’s family to re-arrange items in their home.
To increase Stephany’s compliance with completing demands associated with her morning routine without engaging in problem behavior, a life skills treatment was implemented. For life skills sessions, the purple card interval indicated time in which Stephany was required to complete life skills tasks such as folding and putting away clothes or brushing her teeth. To address the goal that Stephany complete academic tasks without engaging in problem behavior the treatment was modified to include academic sessions. During academic sessions, Stephany was required to complete an academic task during the purple card interval. To replicate times in which Stephany and her family members were engaged in their own preferred leisure activities and preferred food was restricted, the treatment was modified to incorporate Stephany’s preferred leisure activities. During purple card intervals for leisure activities, Stephany was prompted to engage in less preferred leisure activities while edible items remained restricted. Lastly, to address times in which Stephany’s leisure items or other non-leisure items in her household were manipulated, the treatment was modified to require Stephany to tolerate periods of time in which another person manipulated her items without her engaging in problem behavior. During interruption sessions, a therapist manipulated Stephany’s leisure items during the purple card interval. Each of these permutations of the treatment package was addressed separately (see Figure 3).
Due to an increase in problem behavior across the life skills, academic, and interruption sessions, response cost and resetting differential reinforcement for other behavior (DRO) components were implemented across all conditions. The response cost component was implemented during yellow card intervals and consisted of immediately changing the yellow card to the purple card contingent upon problem behavior. In other words, Stephany lost the opportunity to request preferred edible items contingent upon problem behavior. The DRO component was implemented during purple card intervals and consisted of the resetting of the purple card interval contingent upon problem behavior. For example, if the purple card interval was set at 5min and Stephany engaged in problem behavior during the first minute of the interval, she would have to go an additional 5min without engaging in problem behavior to gain access to the yellow card interval. It is important to note that had the treatment evaluation ended prior to modifying the treatment to address multiple treatment goals, Stephany would have been discharged with a treatment that had been evaluated only in a highly internally valid manner. However, through an emphasis on external and social validity, further treatment evaluation resulted in modifications to maintain low rates of problem behavior in more naturalistic settings and achieve her caregiver’s goals.
Treatment Generalization and Caregiver TrainingAs previously discussed, evaluating the effectiveness of treatments beyond an austere session room is a critical, and often overlooked, component of treatment evaluations. Therefore all of Stephany’s treatment sessions were generalized to more naturalistic settings within the clinic and subsequently to her own home and school settings. For example, the leisure and interrupt sessions were conducted in clinic space that was designed to resemble a family’s home. It contained a living room area with a couch and television; a dining area with a table and chairs; a kitchen area with a fridge, cabinets, counters, and a dishwasher; and lastly a play area with shelves containing a wide variety of leisure items. Academic sessions were generalized to a similar clinical space that was designed to resemble a classroom that contained several desks, chairs, and tables. Life skills sessions were generalized to both the classroom setting and a bathroom. In addition, other clients and therapists who were part of the day treatment clinic were present in the playroom and classroom, which replicated situations in Stephany’s home and school in which other family members or peers were present.
In addition to evaluating treatment effectiveness in more naturalistic settings, it is also important to ensure that the treatments are designed to incorporate naturally existing reinforcement contingencies when possible. By doing so (e.g., delivering reinforcers after all of the clothing items are folded versus delivering reinforcement after 15min of folding clothes), treatments can become easier for caregivers and teachers to implement and less stigmatizing for the client. Therefore, treatment for academics and life skills were both modified so that reinforcement was contingent upon compliance or task completion. Stephany engaged in low rates of problem behavior across the leisure, life skills, interrupt, and academic sessions during this generalization phase (see Figure 3).
Lastly, Stephany’s caregivers completed intensive training on the treatment protocol until they were implementing all treatment components consistently (i.e., 80% or higher treatment fidelity). This training made it possible to conduct the final phase of treatment: generalization to the natural environment (i.e., Stephany’s home and school). During the last two weeks of Stephany’s admission, all sessions were conducted in her own home and school. Stephany’s problem remained low across leisure, life skills, interrupt, and academic sessions when treatment was generalized to these settings (see Figure 3).
DiscussionOverall, Stephany’s case serves as a useful example of how to ensure that FAs and function-based treatments are socially valid. Important steps that were part of Stephany’s admission, but are not always discussed in the research literature, included identifying treatment goals that were meaningful to the individual and their caregivers, designing an individualized FA, adapting treatments to address multiple goals, training caregivers to implement the treatment, and generalizing treatments to the natural environment. Stephany’s treatment goals emphasized social validity in that they were nominated by her mother and targeted specific situations that were problematic in their lives. Functional analysis conditions emphasized social validity in that they were individualized to assess the specific antecedents and consequences that were problematic for Stephany (e.g., evaluating interruption and manipulation of items, restricted access to preferred edible items). When implementing function-based treatments for problem behavior, service providers should strive to develop treatments that are feasible for caregivers to implement in the natural environment. Methods of increasing the feasibility of treatments can range from incorporating naturally occurring contingencies for appropriate behavior to modifying a single treatment package to address multiple treatment goals. A final component of ensuring that a treatment is socially valid is to evaluate the treatment in increasingly naturalistic environments. Ultimately, a successful treatment means that caregivers are able to implement a treatment within their daily lives and maintain the treatment effects that are meaningful to them. Through a more socially valid approach to the assessment and treatment of problem behavior, service providers can produce more meaningful changes in individuals’ and their caregivers’ lives.