We present the clinical case of a 74-year-old woman with an urachal tumor diagnosed in 2004. The patient underwent a partial cystectomy of the dome with remotion of the urachal remnant and the umbilicus. She had been clinical well until 2011 when she had a kidney metastasis from the urachal tumor.
Urachal tumors are very rare, comprising 0.17-0.34% of all bladder cancers. The most common sites of distant metastases are: lung, lymph nodes, bone, intestine, brain, liver, peritoneum, skin and spine. We describe an extremely rare case of a renal metastasis from an urachal cancer, seven years after the initial diagnosis.
Usually, patients with localized disease have a good prognosis when treated with surgery. The prognosis gets worse for patients with metastases or local recurrence because a standard chemotherapy regimen does not exist.
Apresentamos o caso clinico de uma doente com 74 anos diagnosticada com tumor do úraco em 2004. A doente foi submetida a cistectomia parcial da cúpula vesical com excisão do úraco e do umbigo. Esteve clinicamente bem até 2011 quando lhe foi diagnosticada uma metástase renal do tumor do úraco.
Os tumores do úraco são muito raros, compreendendo 0,17-0,34% de todos os tumores da bexiga. Os locais mais comuns de metastização à distância são: pulmão, gânglios linfáticos, osso, intestino, fígado, peritoneu, pele e coluna. Descrevemos um caso extremamente raro de uma metástase renal de um adenocarcinoma do úraco sete anos após o diagnóstico inicial.
Habitualmente, os doentes com doença localizada apresentam um bom prognóstico quando tratados com cirurgia. O diagnóstico é pior para doentes com metástases ou recorrência local uma vez que ainda não existe um regime de quimioterapia estabelecido.
Urachal adenocarcinomas are very rare tumors, usually diagnosed at an advanced stage because the lack of symptoms. We present a rare case of a renal metastasis developed seven years after the first treatment.
Case reportWe present the case of a 74-year-old woman that was sent to the urologist in 2003 to investigate gross hematuria. She did a computed tomography (CT) scan that showed a proliferative mass of the anterior bladder wall. The cystoscopic evaluation confi a lesion at the bladder dome. The lesion was ressected and the histology revealed infiltration of the bladder mucosa by mucinous adenocarcinoma.
Gynecology and General Surgery excluded secondary adenocarcinoma of the bladder.
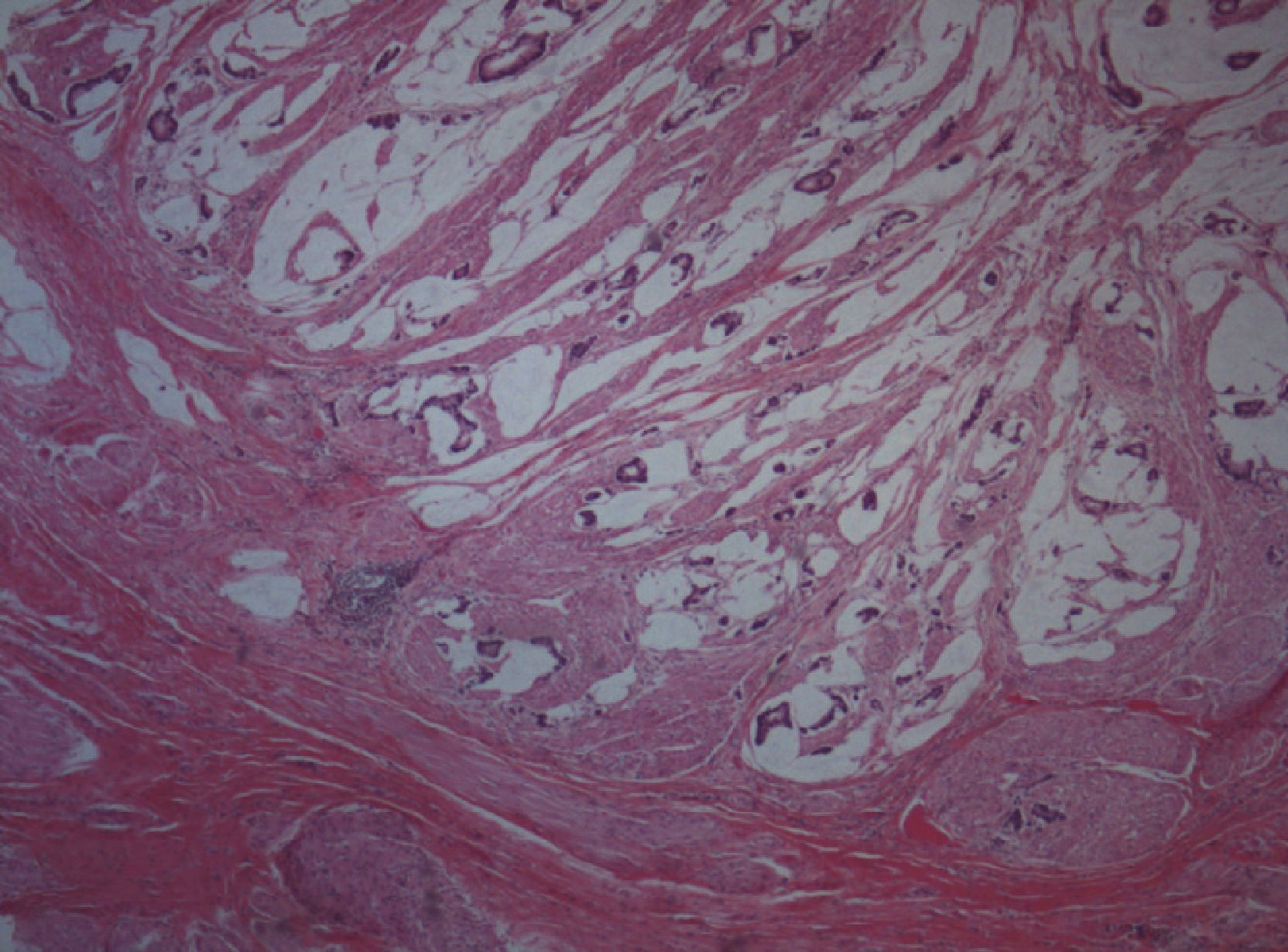
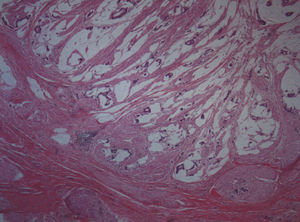
A partial cystectomy of the dome was performed with remotion of the urachal remnant and the umbilicus. The histology revealed infiltration of the bladder mucosa by mucinous urachal adenocarcinoma (Fig. 1).
The follow-up was maintained and the patient had been clinically well until November 2011, when the CT scan of the abdomen and pelvis revealed a renal mass involving the lower pole of the left kidney. This mass had 75×41×54mm and its appearance was suspicious for a proliferative lesion. There was no evidence of lymphadenopathies.
The patient underwent a laparoscopic radical nephrectomy of the left kidney on January 2012.
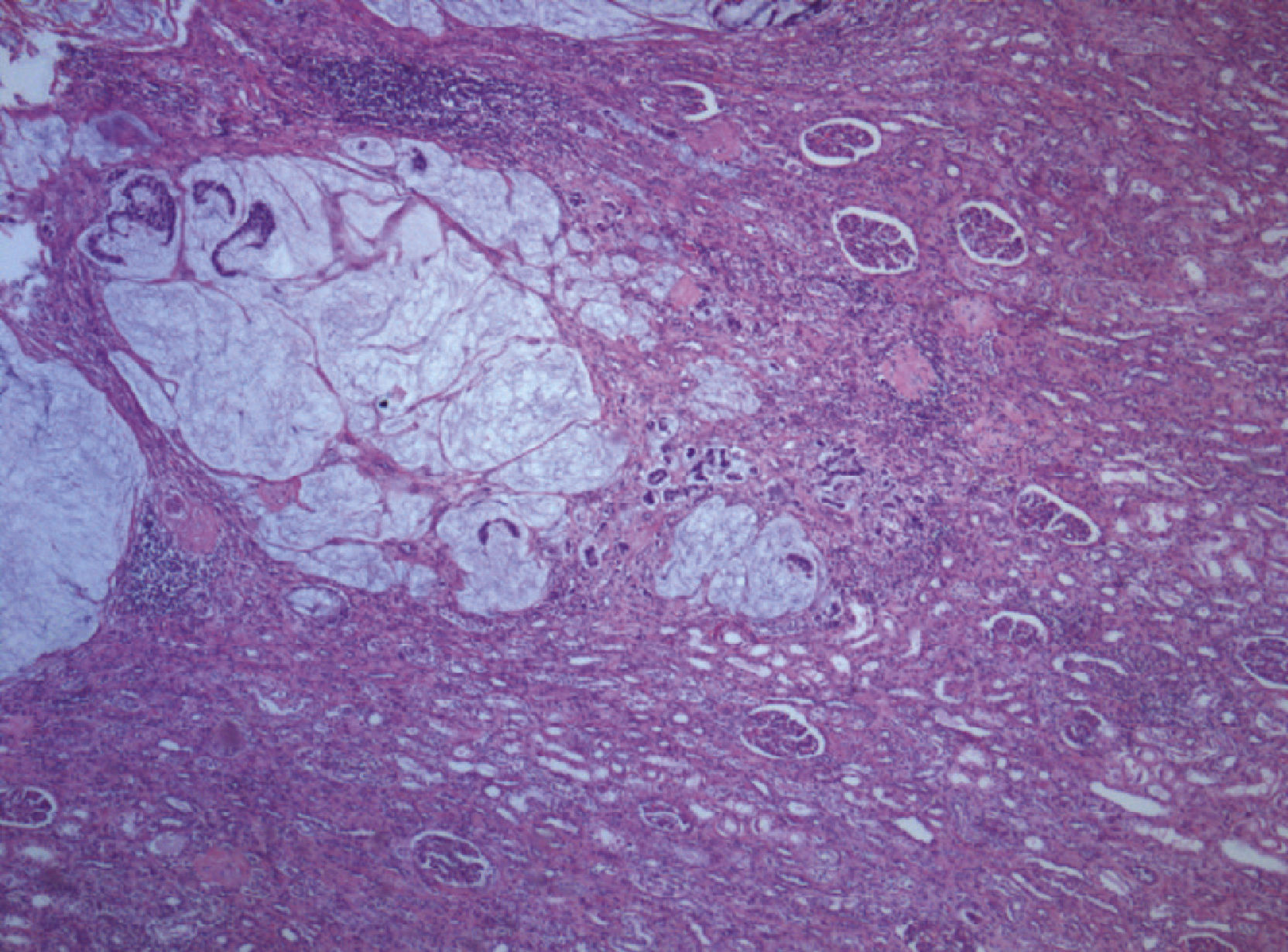
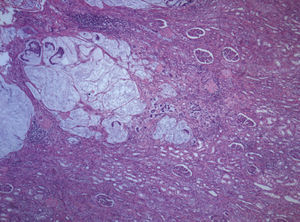
The histology showed infiltration of the renal parenchyma from the Gerota fascia to the calyces by mucinous adenocarcinoma (Fig. 2). Imunohistochemical staining showed that cells were positive to CK20 but negative to CK7. Neural invasion was present and the margins were positive. The histologic exam concluded secondary infiltration of the kidney by mucinous adenocarcinoma similar to the analyses performed in 2003.
The gynecologic exam and the colonoscopy did not reveal alterations. It was concluded that the kidney mass was a metastasis from the urachal tumor.
On May 2012, the patient had an episode of intestinal subocclusion and was admitted in the General Surgery's Department. During this period she underwent a virtual colonoscopy that did not reveal polipoid images. The CT scan of the thorax, abdomen and pelvis showed a latero-aortic lymph node and a heterogeneous lesion in the renal fossa sugestive of local relapse.
The serum levels of carcinoembryonic antigen (CEA) were elevated.
With evidence of disease progression the patient was sent to the Oncologist. She began salvage chemotherapy with Gemcitabine, once a week.
A CT scan performed on February 2013 showed volume reduction of the residual mass and of the latero-aortic lymph node. However it was also documented progression of the disease with identification of a lumbar vertebral sinking.
The patient died on March 2013.
DiscussionAdenocarcinoma of the bladder comprises less than 2% of all bladder carcinomas. They could arise from the bladder proper or from the urachus, or could be an extension of adenocarcinoma from adjacent organs or metastases from a distant organ.1
The histological differentiation between vesical, urachal and metastatic adenocarcinoma is difficult and requires correlation of clinical and pathological findings.1,2
The immunostaining with CK7 and CK20 is used in surgical pathology to help determine the origin of epithelial neoplasms. However, by itself it does not provide sufficient specifi ty to allow accurate distinction between secondary colorectal adenocarcinomas and primary bladder adenocarcinomas.3
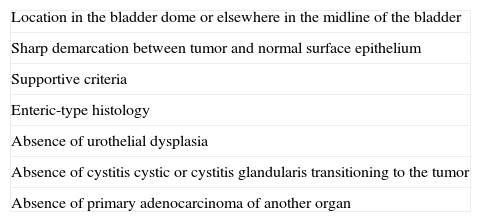
In order to diagnose an urachal cancer some criteria have to be fulfilled (Table 1). Some investigators consider any patient presenting with an enteric-type adenocarcinoma of the bladder, at the bladder dome or elsewhere in the midline as having an urachal tumor until proven otherwise.4
MD Anderson Cancer Centre Criteria for the diagnosis of urachal cancer.
| Location in the bladder dome or elsewhere in the midline of the bladder |
| Sharp demarcation between tumor and normal surface epithelium |
| Supportive criteria |
| Enteric-type histology |
| Absence of urothelial dysplasia |
| Absence of cystitis cystic or cystitis glandularis transitioning to the tumor |
| Absence of primary adenocarcinoma of another organ |
Urachal tumors are very rare neoplasms that represent 0.01% of all cancers5 and 0.17-0.34% of all bladder cancers.6
The majority of cases are described in men, with many reports indicating a median age at diagnosis of approximately 50-60 years.5,7,8
A systematic review of the literature reveals a 5-year survival rate of less than 25%,5,6 although some studies realized in Mayo Clinic revealed a 5-year survival rate of 43-49%.7,8
Patients with this kind of tumor most commonly present with hematuria.6–8 Another symptoms described by different authors are: mucinuria, palpable mass in the lower abdomen, bacteriuria, pain, disuria and umbilical discharge.4,6,7
Owing to lack of early symptoms, the cancer usually presents at an advanced stage.4,5,9,10
The cystocopy usually shows a mass at the dome of the bladder or anterior wall which could be described in appearance as a polypoid or ulcerated lesion.6,7
Like other enteric-type adenocarcinomas, urachal tumors may have detectable serum levels of CEA, CA125 and cancer antigen 19-9. These serum markers could be helpful in evaluating response to systemic chemotherapy.4,10
The gold standard of treatment is the surgery that includes an en bloc resection of the urachal ligament and umbilicus with a complete or partial cystectomy.4,6,10 Sampling lymph nodes allows a better staging of the disease.7
Some authors describe as risk factors associated with recurrence after surgery: positive margins, lymph node or other metastases at the time of surgery, tumor grade and failure to resect the umbilicus.4,5,8
Local recurrence after surgery include: pelvic lymph nodes, peritoneum and omentum. The most common sites of distant metastases are: lung, lymph nodes, bone, intestine, brain, liver, peritoneal carcinomatosis, skin and spine.4,7,8 The rare distant metastases are: scalp, pleural effusion, adrenal, abdominal wall, pancreas and orbit.4
Surgical resection of local tumor recurrences can be curative, but the role of radiation therapy and chemotherapy are unclear.8
There is no standard chemotherapy regimen and the choice of regimens has been based on case reports and single institution experiences.10
The standard chemotherapy for this type of cancer should include a taxane or a regimen used to treat gastrointestinal malignances as opposed to standard transicional cell carcinoma regimens which have not shown much efficacy.10
The clinical trial with Gemcitabine+fluorouracil+leucovorin+cisplatin (Gem-FLP) is showing promise and may provide a chemotherapy standard.4,10
Usually, patients with localized disease have a good prognosis when treated with surgery. The prognosis gets worse for patients with metastases or local recurrence as we show with this case.
We described a renal metastasis from urachal cancer. This clinical case shows that positive margins after surgery may represent a risk factor to recurrence. Given the rarity of urachal cancer, all new findings are important to improve the knowledge in this area. The creation of randomized follow-up studies with collaboration of different institutions is necessary to investigate the role of adjuvant and salvage therapies and establish a standard regimen.
Ethical disclosuresProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We acknowledge the Pathology Department of Hospital Curry Cabral for the figures.