During the beginning of the COVID-19 pandemic in our center, neither prehabilitation nor multimodal rehabilitation could be applied due to the excessive patient load on the health system and to reduce SARS-CoV-2 transmission. The objective of our study was to analyze the evolution, complications, and survival up to one year of patients who underwent radical cystectomy in our hospital from March 1st to May 31st, 2020 (period of the first wave COVID-19 pandemic in Spain). We also compared the results with cystectomized patients outside the pandemic period and with application of the ERAS (Enhanced Recovery After Surgery) protocol.
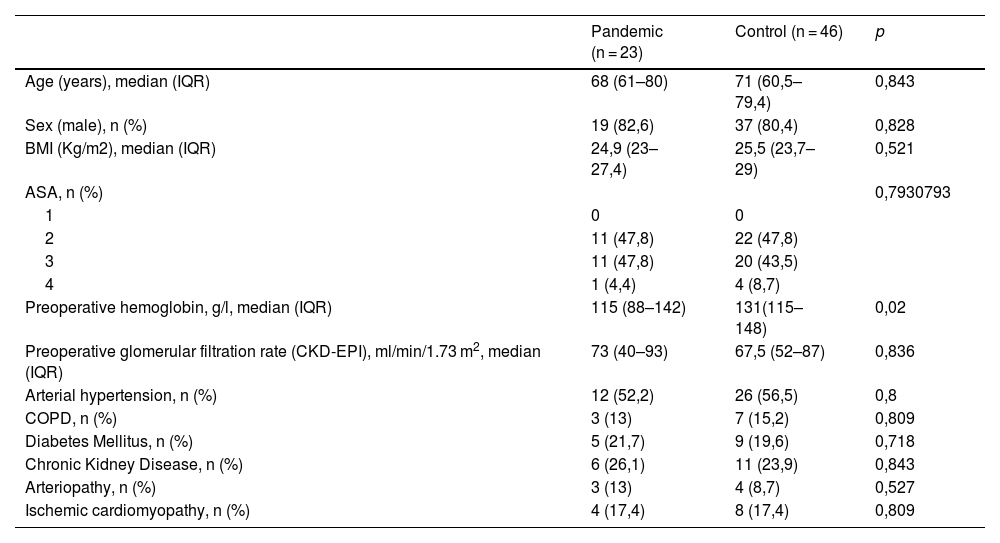
Material and methodsSingle-center, retrospective cohort study of patients scheduled for radical cystectomy from March 1st, 2020 to May 31st, 2020. They were matched with previously operated patients using a 1:2 propensity matching score. The matching variables were demographic data, preoperative and intraoperative clinical conditions.
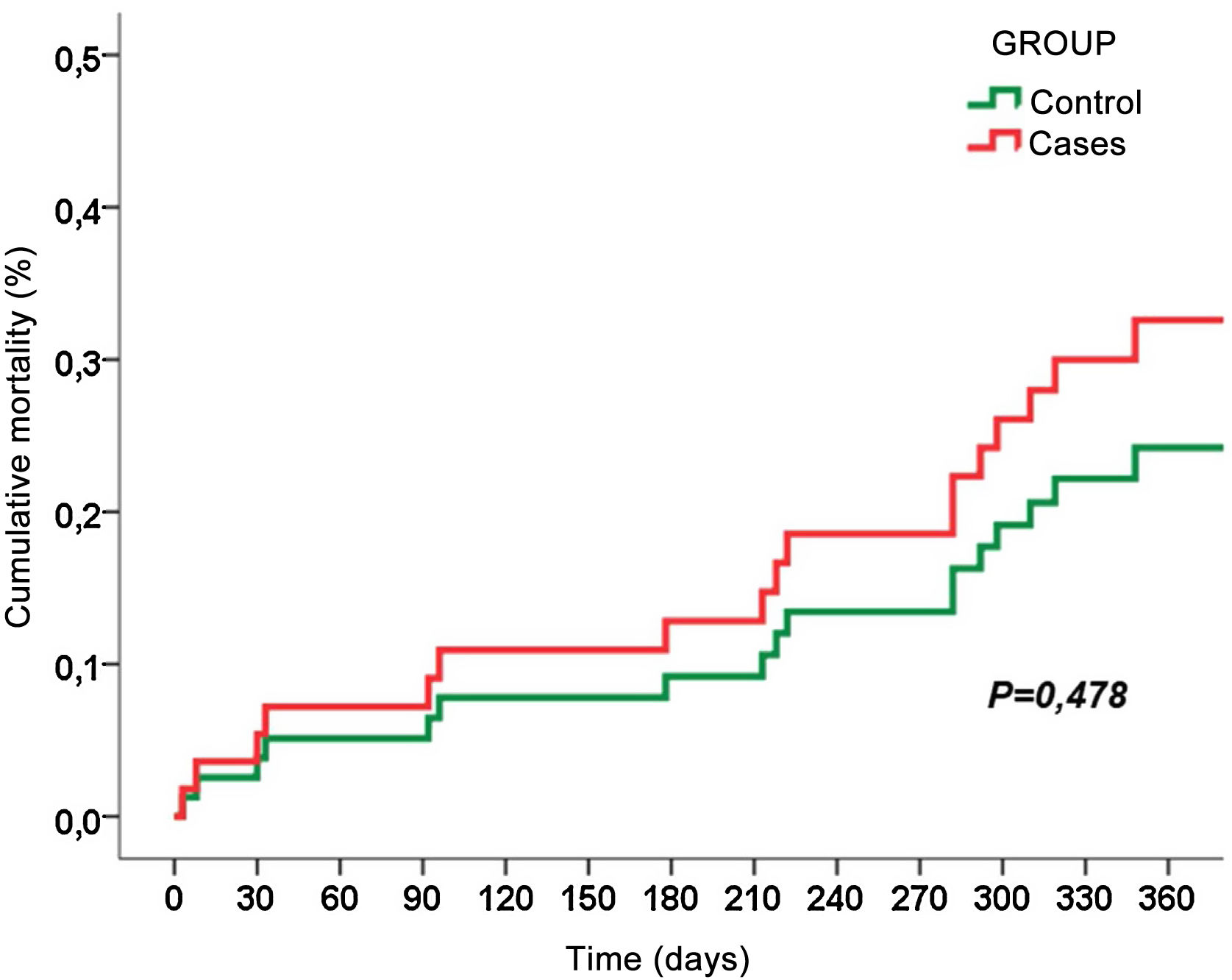
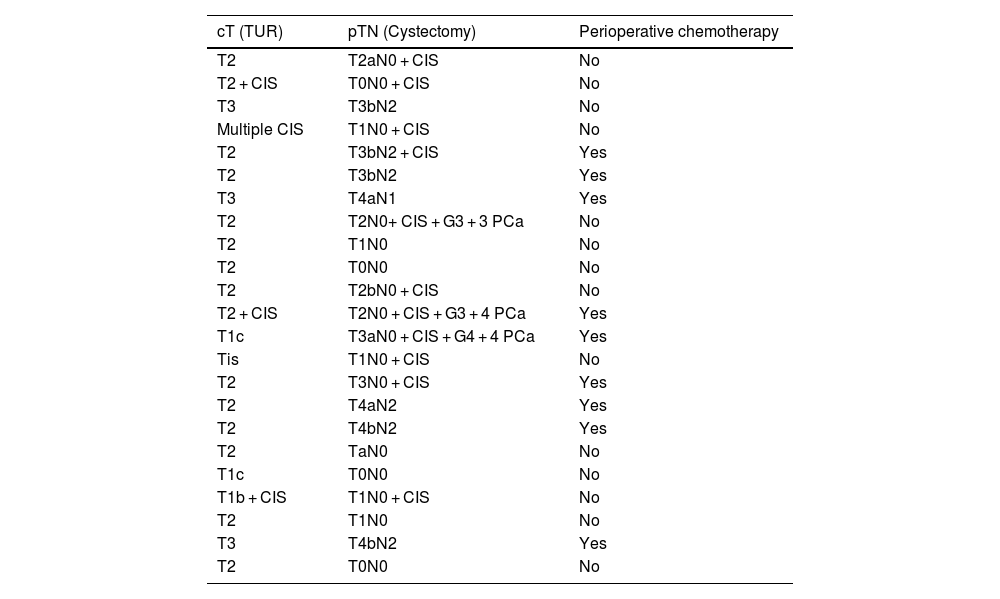
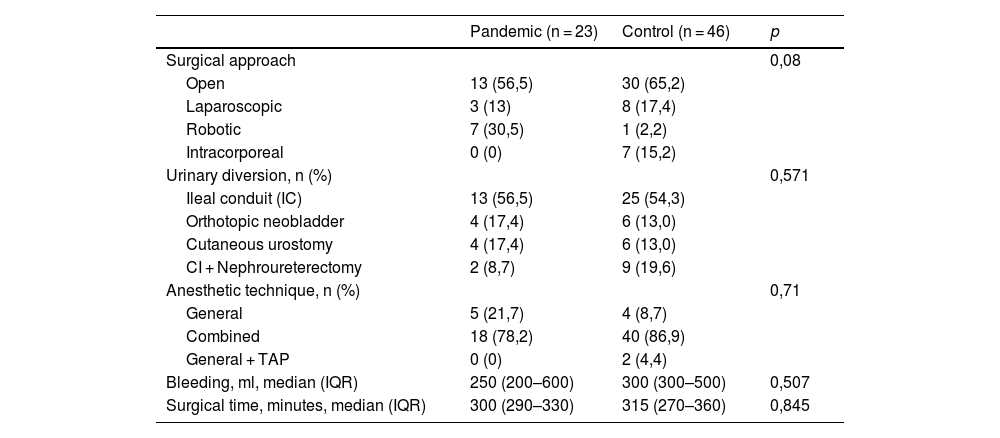
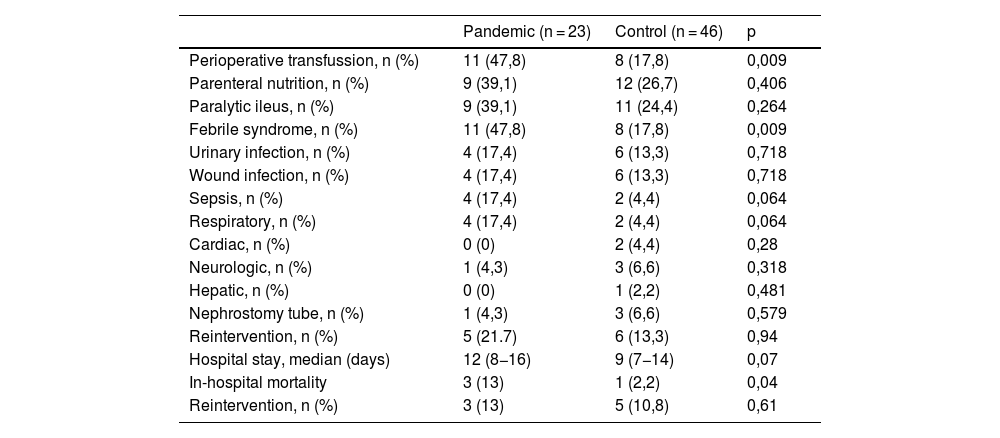
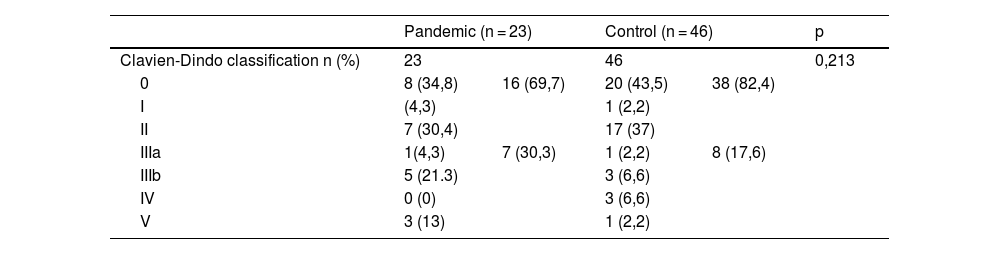
ResultsA total of 23 radical cystectomies with urinary diversion were performed in the period described. In none of the cases the prehabilitation or the follow-up of our ERAS protocol could be applied, and this was the only difference we found between the 2 groups. Although the minimally invasive approach was more frequent in the pandemic group, the difference was not statistically significant. Three patients were diagnosed with COVID-19 during their admission, presenting severe respiratory complications and high in-hospital mortality. Apart from respiratory complications secondary to SARS-CoV-2, we also found statistically significant differences in other postoperative complications. The hospital stay increased by 3 days in the pandemic group.
ConclusionsPatients who underwent radical cystectomy at our center during the first wave of the COVID-19 pandemic had a higher number and severity of respiratory and non-respiratory complications. Discontinuation of the ERAS protocol was the main difference in treatment between groups.
Al inicio de la pandemia COVID-19 no se pudo implementar ni prehabilitación ni rehabilitación multimodal por sobrecarga del sistema sanitario. Nuestro objetivo fue analizar evolución, complicaciones y supervivencia hasta el año de pacientes sometidos a cistectomía radical en nuestro centro desde 1 de Marzo hasta 31 de Mayo de 2020 (primera ola). Comparamos resultados con pacientes también cistectomizados fuera de pandemia donde sí estaba instaurado el protocolo ERAS.
Material y MétodosEstudio de cohortes retrospectivo, unicéntrico, de pacientes programados para cistectomía radical desde 1 de marzo de 2020 hasta 31 de mayo de 2020; se emparejaron con pacientes intervenidos anteriormente a través de score de emparejamiento por propensión 1:2. Las variables de emparejamiento fueron datos demográficos, condiciones clínicas preoperatorias e intraoperatorias.
ResultadosSe realizaron 23 cistectomía en este periodo; en ningún caso se aplicó ni prehabilitación ni seguimiento del protocolo ERAS, y ésta fue la única diferencia en el tratamiento entre grupos. Tres pacientes se diagnosticaron de COVID-19 durante su ingreso presentando complicaciones respiratorias graves y alta mortalidad intrahospitalaria. La tasa de transfusión sanguínea fue mayor en el grupo pandemia. La estancia hospitalaria aumentó en 3 días en grupo pandemia.
ConclusionesLos pacientes sometidos a cistectomía en nuestro centro durante la primera ola de pandemia COVID-19 presentaron complicaciones respiratorias y no respiratorias en mayor número y más graves que los cistectomizados fuera de este periodo. La no aplicación del protocolo ERAS fue la principal diferencia en el tratamiento entre grupos.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora