China and Spain are world leaders in the consumption of edible bulbs (garlic and onion), but there are few references to their capacity to cause allergic symptoms. The target was to study allergic sensitization and clinical symptoms associated with garlic and onion consumption in a large sample of allergic patients.
MethodsAn observational cross-sectional study was conducted, testing garlic and onion extracts in 8109 patients of all ages seen by our allergy clinic in 2018. Forty-four aeroallergens and foods were tested, including garlic and onion, with prick test and determination of specific IgE. Oral provocation and contact tests were performed if a delayed reaction was suspected. Western Blot was performed in the serum of patients positive to garlic and onion.
ResultsWe conducted 356,798 skin tests and 4254 specific IgE determinations. Of the 8109 patients tested, 2508 (30.92%) presented with symptoms associated with food intake and, in these patients, food hypersensitivity was detected by skin test, positive specific IgE or provocation in 924 patients, and was caused by garlic or onions in 27, indicating a prevalence of 2.92%. Immunodetection showed an association between the symptoms and a specific LTP to these bulbs, without cross-reactivity with other LTPs in the Mediterranean diet (peach, wheat).
ConclusionsAllergic hypersensitivity to garlic and onions should not be underestimated and, given their high consumption, should be included in the diagnostic food allergy battery.
New allergenic sources of food allergies continue to appear,1–4 some of which have not been studied in depth.
Garlic (Allium sativum) is a bulbous vegetable of the Amaryllidaceae family. It is widely used in cooking, especially in the Mediterranean area, and is also attributed medicinal properties, being used in medicine for the treatment of hypercholesterolemia and the prevention of arteriosclerosis.5 It contains group B and C vitamins, and minerals such as potassium or calcium, as well as sulphur substances (mainly aliin).
Garlic production continues to grow, especially in Asia, the Mediterranean, and North and South America. China is the leading producer. In Europe, Spain is the leading producer, and the autonomous community of Castile-La Mancha has the largest number of hectares dedicated to garlic.
The onion (Allium cepa) also belongs to the Amaryllidaceae family.
Edible onions include the green onion (Allium fistulosum), the shallot (Allium ascalonicum) and chives (Allium sxhoenoprasum). Onions release an irritating substance (thiopropanal sulfoxide) when cut. The onion bulb is composed of cells bound with peptin. Onions are composed mainly of water, but also contain salicin, aliin (both present in greater amounts in garlic), quercetin, thiopropionic acid (which promotes eye irritation), glycolic acid, flavonoids, carbohydrates, amino acids, and minerals such as potassium or copper, and vitamins.
Bulbs are reported to cause allergic respiratory and cutaneous conditions.8–14
Diallyl disulfide is an important allergen in garlic and onion that is known to cause contact dermatitis.6,7,10 Garlic is the most frequent cause of contact dermatitis in the fingers and pulpitis in housewives and suppliers5 and may result in various cutaneous manifestations, most commonly chronic pulpitis of the first three fingers.
The Amaryllidaceae family in general has been implicated as a cause of occupational rhinoconjunctivitis and bronchial asthma,8,9 but there is little information on food allergy, perhaps due, as mentioned in some articles, to its weak allergenicity,8 although cases of anaphylaxis have been reported.11,12
The aim of this study was to investigate allergic sensitization and the clinical symptoms associated with garlic and onion in a large sample of allergic patients.
Materials and methodsStudy designWe carried out a cross-sectional observational study of patients attending the allergy clinic of the Río Hortega University Hospital of Valladolid (HURH) during 2018 to evaluate sensitization to garlic and onion. A total of 8109 patients were evaluated. Prick tests were made and food-specific IgE antibodies, including bulbs, were evaluated in addition to provocation tests in patients who agreed. Contact tests were performed if a cutaneous or late reaction was suspected and Western Blot was carried out in sera of patients positive to garlic or onion.
The protocol was approved by the HURH Clinical Research Ethics Committee and written informed consent was given by patients for all diagnostic techniques used.
Cutaneous tests (prick test)Prick tests were carried out according to European Academy of Allergy and Clinical Immunology (EAACI) standards and previous studies with garlic.11 A positive test was defined as a wheal of ≥3mm 15–20min after administration, with histamine as a positive control and physiological saline solution as a negative control. Each allergen was tested twice, and the results were recorded for digitalisation.
Allergenic extracts: a battery of 42 aeroallergens was tested (pollens from grasses, trees, weeds and flowers, Dermatophagoides and storage mites, fungi (Alternaria, Cladosporium, Aspergillus, Penicillium and Candida), antigens from seven animals and foods (wheat, barley, rye, egg, milk, nuts, legumes, fish, mustard, anisakis, and lipid transfer proteins (LTP) from fruits and profilins) using commercial allergens (ALK Abelló, Madrid and Leti Barcelona, Spain), and commercial extracts and prick-prick tests with garlic and onion from Castile at 1/100 dilution, which avoided the irritant effect of allylic acid. We performed 356,798 skin tests in the 8109 new patients tested during 2018.
Determination of specific IgEWe made 4254 determinations of IgE using ImmunoCAP, (Thermofisher, Upssala, Sweden).
ProvocationWe carried out a double-blind, placebo-controlled challenge with garlic in two patients who gave consent. The test was made with 5mg of raw garlic, masked and pulverized in peppermint syrup, after fasting for six hours.
Contact tests (European contact battery, /True tests® and GEIDAC)Contact tests were carried out in patients with pulpitis or dermatitis in the hands after handling garlic or onion and those with eczematous dermatitis.
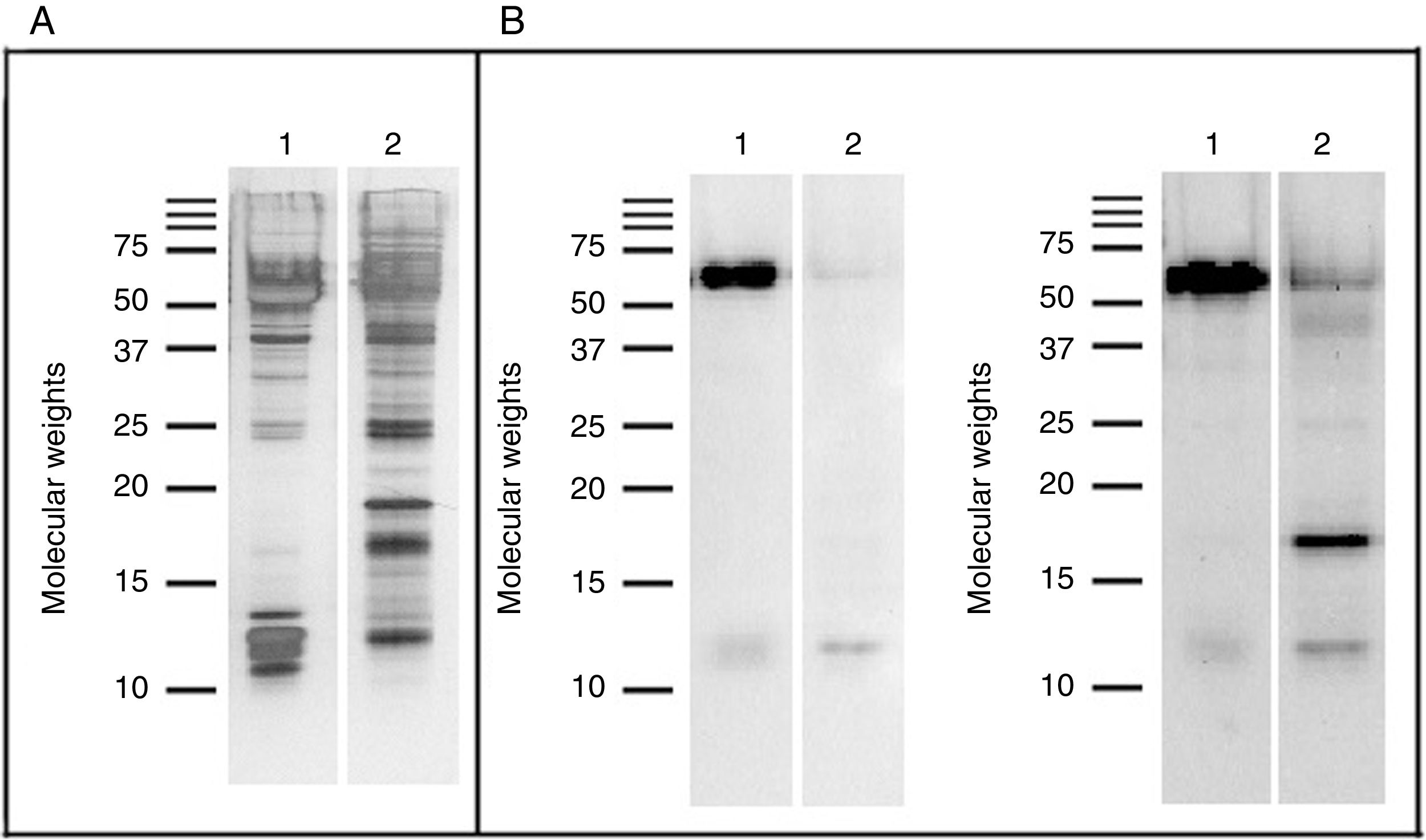
Study of allergenic profilesThe following studies were carried out13: immunodetection of allergens with pools of sera from patients allergic to garlic and onions, respectively. Garlic and onion proteins were extracted by suspension in a buffer solution (phosphate buffered saline, pH 7.4) for two hours at 4°C. After centrifugation, the supernatant was separated from the insoluble part, dialyzed against water, and then lyophilized.
Once the proteins were extracted, the protein concentration of the two extracts was determined according to the Bradford method.15 Subsequently, the proteins from the two extracts were analyzed using SDS–PAGE (polyacrylamide gel electrophoresis with sodium dodecyl sulfate, with proteins being separated according to their electrophoretic mobility) according to the protocol used by Laemmli,16 with cleavage of structural proteins during the assembly of the head of bacteriophage T4 in 15% polyacrylamide gels under reducing conditions. Finally, the proteins were visualized using Coomassie Blue stain R-250.
In an analogous experiment, the proteins were transferred electrophoretically to a polyvinylidene difluoride membrane (BioRad). Binding to the allergens was analyzed used Western Blot, which evaluates the binding of antibodies in sera to the separated protein components to determine which component of the food they react against, using a mixture of the sera of the patients sensitized to the source and the antihuman conjugate non-IgE peroxidase (Southern Biotech). Detection reagents (Western Lightning Plus-ECL, Perkin Elmer) were added to visualize the proteins recognized.
Statistical analysisWe analyzed the 181 allergens for which 4254 determinations of specific IgE were positive. We studied the characteristics of the 27 patients sensitive to garlic or onion, obtaining the frequency of each variable according to sex and contingency tables. The associations between study variables were analysed using Pearson’s Chi-square test. The statistical analysis was performed with the SPSS program version 15.0.
ResultsOf the 8109 patients initially analysed, 2508 (30.92%) reported food-related symptoms. Of these, hypersensitivity to foods (either by cutaneous test, specific IgE or provocation) was observed in 924 (11.39%) patients, and in 27 of these the symptoms were caused by edible bulbs, indicating a prevalence of 2.92% of patients with food hypersensitivity.
After testing, 17 patients were found to be sensitive to garlic and 10 to onion. This included two cases of professional asthma due to inhalation of bulb vapors by chefs and two cases of pulpitis in the index fingers and thumb of the left hand that were diagnosed by contact tests. In addition, an infant who had never consumed garlic was possibly sensitized through breast milk, as the mother very frequently consumed garlic. Provocation tests in the two patients who agreed to them showed labial oedema and urticaria in the first 30min after the test.
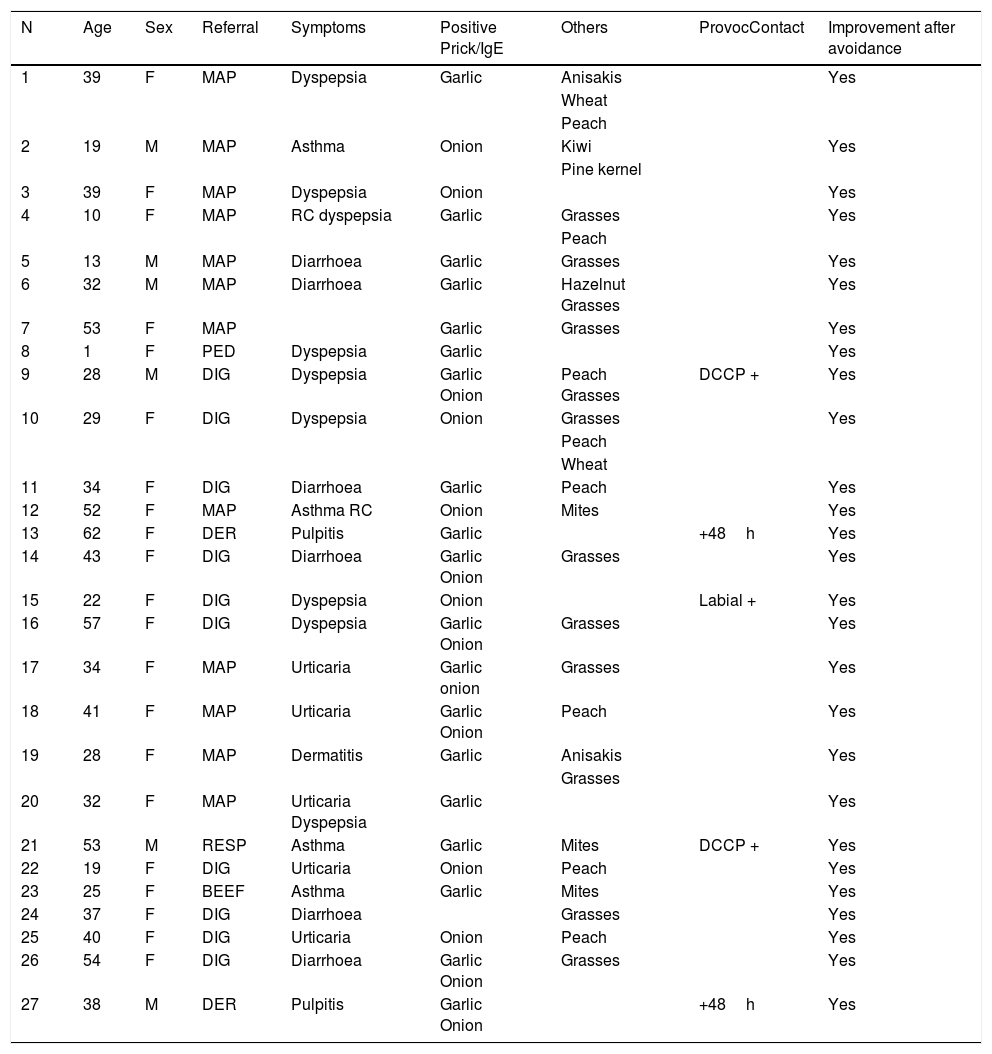
The demographic and clinical data of the 27 patients are shown in Table 1; 29.6% were male. Forty-four per cent were referred from primary care and 37% from the digestive service, 7.4% from pulmonology and 7.4% from dermatology (two patients each), and one from paediatrics. The predominant symptoms were chronic diarrhoea (14.8%), dyspepsia (flatulence, poor digestion) (11.1%), and asthma (7.4%).
Demographic and clinical data of the 27 patients allergic to garlic and/or onion.
| N | Age | Sex | Referral | Symptoms | Positive Prick/IgE | Others | ProvocContact | Improvement after avoidance |
|---|---|---|---|---|---|---|---|---|
| 1 | 39 | F | MAP | Dyspepsia | Garlic | Anisakis | Yes | |
| Wheat | ||||||||
| Peach | ||||||||
| 2 | 19 | M | MAP | Asthma | Onion | Kiwi | Yes | |
| Pine kernel | ||||||||
| 3 | 39 | F | MAP | Dyspepsia | Onion | Yes | ||
| 4 | 10 | F | MAP | RC dyspepsia | Garlic | Grasses | Yes | |
| Peach | ||||||||
| 5 | 13 | M | MAP | Diarrhoea | Garlic | Grasses | Yes | |
| 6 | 32 | M | MAP | Diarrhoea | Garlic | Hazelnut Grasses | Yes | |
| 7 | 53 | F | MAP | Garlic | Grasses | Yes | ||
| 8 | 1 | F | PED | Dyspepsia | Garlic | Yes | ||
| 9 | 28 | M | DIG | Dyspepsia | Garlic Onion | Peach Grasses | DCCP + | Yes |
| 10 | 29 | F | DIG | Dyspepsia | Onion | Grasses | Yes | |
| Peach | ||||||||
| Wheat | ||||||||
| 11 | 34 | F | DIG | Diarrhoea | Garlic | Peach | Yes | |
| 12 | 52 | F | MAP | Asthma RC | Onion | Mites | Yes | |
| 13 | 62 | F | DER | Pulpitis | Garlic | +48h | Yes | |
| 14 | 43 | F | DIG | Diarrhoea | Garlic Onion | Grasses | Yes | |
| 15 | 22 | F | DIG | Dyspepsia | Onion | Labial + | Yes | |
| 16 | 57 | F | DIG | Dyspepsia | Garlic Onion | Grasses | Yes | |
| 17 | 34 | F | MAP | Urticaria | Garlic onion | Grasses | Yes | |
| 18 | 41 | F | MAP | Urticaria | Garlic Onion | Peach | Yes | |
| 19 | 28 | F | MAP | Dermatitis | Garlic | Anisakis | Yes | |
| Grasses | ||||||||
| 20 | 32 | F | MAP | Urticaria Dyspepsia | Garlic | Yes | ||
| 21 | 53 | M | RESP | Asthma | Garlic | Mites | DCCP + | Yes |
| 22 | 19 | F | DIG | Urticaria | Onion | Peach | Yes | |
| 23 | 25 | F | BEEF | Asthma | Garlic | Mites | Yes | |
| 24 | 37 | F | DIG | Diarrhoea | Grasses | Yes | ||
| 25 | 40 | F | DIG | Urticaria | Onion | Peach | Yes | |
| 26 | 54 | F | DIG | Diarrhoea | Garlic Onion | Grasses | Yes | |
| 27 | 38 | M | DER | Pulpitis | Garlic Onion | +48h | Yes |
After avoidance of the bulb (85.2%) patients improved and 11.1% were cured, and 3.7% improved after barrier measures were introduced.
The most significant association with other foods was with LTP of peach and wheat (p<0001). However, immunodetection revealed a specific LTP without cross-reactivity with other LTPs in the Mediterranean diet (peach, wheat). The reactivity of sera against the proteins from the garlic and onion extracts is shown in Fig. 1. Several components binding to IgE were revealed. In the pool of sera from patients sensitized to garlic, two proteins of approximately 12 and 60kDa were recognized in both extracts, although the 60kDa protein was revealed with greater intensity in the garlic extract. The mixture of sera from patients sensitized to onion recognized the same proteins as the garlic extract and, additionally, a protein of approximately 17kDa was revealed with a high intensity in the onion extract.
Discussion/ConclusionAny food may be an allergen, although some are more frequent than others.1,3 Onion consumption in Spain is 1,351,495tons, suggesting they might be considered as potential allergens, although they are not usually included in diagnostic food batteries.
In 2011, an observational, retrospective study of all patients diagnosed with dermatitis due to contact with proteins in the last 10 years was carried out in the dermatology skin allergy unit of the Hospital de Valencia, and it was found that 3.7% of cases were caused by pork, garlic and anisakis.10
Onion is also involved in cases of contact dermatitis, but there are few reports on onions as a source of food allergy, although isolated cases of patients with anaphylaxis have been described.11,12 The first report of monosensitization to the thermolabile component of onion was in 2000 in a 44-year-old patient who presented an anaphylactic reaction after eating raw or undercooked onions, but not when eating well-cooked onions.12 The case of a woman with an anaphylactic reaction after eating garlic has been described. This patient was also sensitized to pollen and nuts.11 A case of urticaria and oral itching after ingestion of raw onion was reported in a patient with a history of rhinoconjunctivitis and contact urticaria with mugwort and oral itching with peach skin, with LTP being found to be a trigger allergen in food allergy to onions.13 A 2013 study of 108 Saudi patients evaluated specific IgE for garlic and onion in patients already under study for food allergy: 15 patients had serum IgE for garlic and onion, and specific antibodies to both garlic and onion were detected in 12 patients.14
In 2015, a genetic analysis of the onion bulb was carried out to identify possible allergens.7 Based on sequence homology onion genes were categorized into 49 different groups. Of the categorized genes, 61.2% showed metabolic functions followed by cellular components such as binding, cellular processes; catalytic activity and cell part.
In 2018, a nine-month old baby accidentally ingested homemade garlic sauce which caused generalized erythema and coughing. In our series, an infant who had never consumed garlic was possibly sensitized through breast milk, a young man presented anaphylaxis after eating raw onion and two cooks had professional asthma when cutting garlic.4 In our study, two patients also had pulpitis related to garlic, and therefore garlic should be taken into account as a professional allergen.
Early diagnoses of food allergy can greatly improve the quality of life by avoiding unnecessarily restrictive diets. In 2014 there was an increase in the incidence of allergy to onions and garlic, perhaps because the world production of garlic and onions has increased substantially, and they have become common foods, with culinary and therapeutic uses, although their cultivation goes back thousands of years.8
The only clinically-relevant garlic allergen identified to date is aliin lyase, which was identified and characterized in 2004, although other possible garlic allergens have been suggested.6 Likewise, cross reactivity within the Amaryllidaceae family was also demonstrated in the same year. Cross-reactivity between this family and grass pollens has also been shown.17
Our study suggests the need to evaluate sensitization to garlic and onion in persons with food allergies of unclear cause, and in people with dyspepsia and chronic diarrhoea, given their widespread use in the Mediterranean diet. The prevalence found (2.9%) indicates there is greater, but not negligible, tolerance than for other foods. This might be genetic, as garlic and onions have formed part of the Spanish diet since ancient times.
A response to similar proteins was demonstrated in garlic and onion (12 and 60Kda respectively), and a 17 KDa protein in the onion extract. Immunodetection showed an association between the symptoms and specific LTPs to these bulbs without cross-reactivity with other LTPs in the Mediterranean diet (peach, wheat).
The Saudi study is perhaps the study most similar to ours, and concluded that specific IgE antibodies to garlic and onion in a considerable number of patients indicate sensitization and the allergenic potential of these foods. However, it was carried out on a much smaller sample of patients who mostly consumed onions.
Our study is novel because it analyzes, for the first time, allergic sensitization and the clinical symptoms associated with garlic and onion in a large sample of allergic patients from an area of high production and consumption of these bulbs.
Conflicts of interestsThe authors have no conflicts of interest to declare.
Declaration of all sources of fundingNone.
The study team would like to thank the contribution of the patients, and the health care professionals who sent them to our clinic and made this research possible.