The definition and diagnosis of asthma are the subject of controversy that is particularly intense in the case of individuals in the first years of life, due to reasons such as the difficulty of performing objective pulmonary function tests or the high frequency with which the symptoms subside in the course of childhood. Since there is no consensus regarding the diagnosis of asthma in preschool children, a systematic review has been carried out.
Materials and methodsA systematic search was made of the clinical guidelines published in the last 10 years and containing information referred to the concept or diagnosis of asthma in childhood – including the first years of life (infants and preschool children). A series of key questions were established, and each selected guide was analyzed in search of answers to those questions. The review protocol was registered in the international prospective register of systematic reviews (PROSPERO), with registration number CRD42017074872.
ResultsTwenty-one clinical guidelines were selected: 10 general guides (children and adults), eight pediatric guides and three guides focusing on preschool children. The immense majority accepted that asthma can be diagnosed from the first years of life, without requiring pulmonary function tests or other complementary techniques. The response to treatment and the exclusion of other alternative diagnoses are key elements for establishing the diagnosis. Only one of the guides denied the possibility of diagnosing asthma in preschool children.
ConclusionsThere is generalized although not unanimous agreement that asthma can be diagnosed in preschool children.
The diagnosis of asthma in children and adults depends on the concept we have of the disease.1,2 This concept has evolved over time, and at present asthma is seen as a heterogeneous disorder or even as a syndrome in which the patient's signs and symptoms reflect or are attributable to a fluctuating increase in flow resistance within the intrapulmonary airway.1,3 The causes underlying this physiopathological process have not been fully clarified, although the factors (endogenous or environmental) intervening in each individual, as well as the natural history of the disease and the response to treatment, are diverse – as reflected by the multiple phenotypes and endotypes that have been described.3–6 Since there are no evidences or a gold standard, the concept and diagnosis of asthma depend on the consensus reached within the scientific community. Such a consensus is usually embodied in the form of national and international guidelines, most of which (including the GINA) have been produced by groups of experts selected on a scantly systematized basis. Although the Delphi method is regarded as the best strategy for consensuses of this kind, it has rarely been applied in the guides on asthma.
The issue about the diagnosis of asthma is not very different from that seen in other respiratory disorders characterized by airflow obstruction – easily recognizable from a clinical point of view, but not that simple when the manifestations are atypical or overlap with those of other diseases. In elderly individuals, asthma poses differential diagnostic problems with chronic obstructive pulmonary disease (COPD) – a circumstance that has led to the controversial purported existence of an asthma-COPD syndrome.7–10 In the first years of life, other intrapulmonary airway disorders also face definition and diagnostic problems, such as bronchopulmonary dysplasia11–14 and acute viral bronchiolitis.15–17 In this regard, some of the manifestations of these disorders can overlap those of asthma which could develop during this early stage of life.18,19
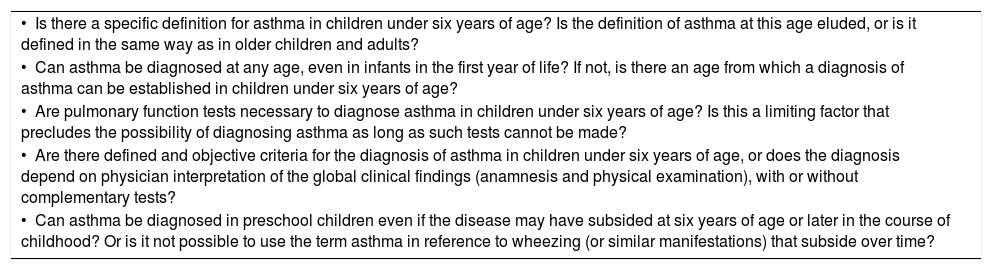
Many children experience recurrent symptoms of bronchial obstruction starting in the first years of life. It is particularly difficult to establish a diagnosis of asthma in infants or preschool children, and the criteria used can vary greatly among different guidelines or studies, and among clinicians, even working in the same setting. This is a problem for determining the true incidence and prevalence of the disease.20 In many cases, the term “asthma” is avoided at such early ages for a number of reasons, including difficulties in performing the pulmonary function tests capable of demonstrating the existence of airflow obstruction,21 a lack of data on the underlying inflammatory substrate,22 or the fact that many children improve and appear to heal in the course of childhood.23–25 All this may cause clinicians to avoid giving a diagnosis that suggests a permanent illness. Spanish pediatricians with expertise in asthma have recently evidenced the lack of agreement referred to basic aspects associated to the diagnosis of asthma in preschool children.26 As a prior step to considering a consensus in Spain, the present study reports the results of a systematic review answering key questions on the concept and diagnosis of asthma in preschool children (i.e., children under six years of age) given in clinical guidelines on asthma. There are very few reviews on the diagnosis of asthma in small children27 or in children and adults28 in clinical guidelines. The selected key questions for this systematic review are presented in Table 1.
Key questions selected for the systematic review of the concept and diagnosis of asthma in children under six years of age in clinical guidelines on asthma.
| • Is there a specific definition for asthma in children under six years of age? Is the definition of asthma at this age eluded, or is it defined in the same way as in older children and adults? |
| • Can asthma be diagnosed at any age, even in infants in the first year of life? If not, is there an age from which a diagnosis of asthma can be established in children under six years of age? |
| • Are pulmonary function tests necessary to diagnose asthma in children under six years of age? Is this a limiting factor that precludes the possibility of diagnosing asthma as long as such tests cannot be made? |
| • Are there defined and objective criteria for the diagnosis of asthma in children under six years of age, or does the diagnosis depend on physician interpretation of the global clinical findings (anamnesis and physical examination), with or without complementary tests? |
| • Can asthma be diagnosed in preschool children even if the disease may have subsided at six years of age or later in the course of childhood? Or is it not possible to use the term asthma in reference to wheezing (or similar manifestations) that subside over time? |
This review was promoted by the working group on respiratory allergy and asthma of the Spanish Pediatric Society of Clinical Immunology, Allergology and Asthma (Sociedad Española de Inmunología Clínica, Alergología y Asma Pediátrica [SEICAP]). Collaboration was requested from the working groups of scientific societies related to pediatric asthma in Spain: the Spanish Society of Pediatric Pulmonology (Sociedad Española de Neumología Pediátrica [SENP]), the Spanish Society of Outpatient and Primary Care Pediatrics (Sociedad Española de Pediatría Extrahospitalaria y de Atención Primaria [SEPEAP]), and the Spanish Association of Primary Care Pediatrics (Asociación Española de Pediatría de Atención Primaria [AEPap]). This resulted in the creation of a group of seven reviewers. Most of the communications among the members of the working group were made via e-mail. The recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) were followed. The project received no funding and involved no direct or indirect participation on the part of any public or private institution. The review protocol was registered in the international prospective register of systematic reviews (PROSPERO), with registration number CRD42017074872.
Search and selection of guidelinesA systematic search was made of clinical guidelines on asthma following the methodology used in an earlier study, with the collaboration of its main author (cited under acknowledgements).29 Based on the strategy defined in that study, an exhaustive search was conducted of the guidelines published between 2007 and 2016 in the Trip Database clinical guides registry, and in the MEDLINE database of the United States National Library of Medicine, through the PubMed browser. Search details: (Practice Guideline[ti] OR Guidelines[ti] OR Practice Guideline[pt] OR Guideline[pt] OR Consensus Development Conference[pt] OR Practice Guidelines as Topic[MeSH]) AND (“Asthma”[Mesh] OR asthma*[ti])). No language restrictions were applied. The search results were evaluated by reading the titles and abstracts in order to extract all the clinical guides or analogous documents that may contain information on the concept and diagnosis of asthma, and which included children under six years of age. These results were complemented by a free search on the part of the investigators participating in the study, to identify other guidelines that might comply with the inclusion criteria, but which had not been identified through the systematic search strategy, including guidelines on wheezing in children, as well as more recent updates on the previously-selected guides, conducted in the course of the year 2017. The documents obtained in the selection were reviewed in detail by the authors. The documents included in the present study were required to contain information on the concept or diagnosis of asthma in childhood, including the first years of life (infants and preschool children). We excluded those documents that did not meet the aforementioned criteria, as well as those containing data on the concept and diagnosis of asthma that could constitute duplicated (contents representing a summary or extract from some other main document) or outdated publications (previous versions of the same more recent guideline). We finally included those guidelines that met the criteria established with the agreement of all the investigators.
Analysis of the guidelinesThe guidelines included in this review were subjected to various exploratory analyses directed by the coordinator, with participation of all the investigators. Due to the narrative style of the sections related to the concept and diagnosis of asthma, questionnaires were presented to the reviewers to clarify the way in which the guidelines considered the diagnosis of asthma in preschool children, particularly related to the age at which the diagnosis can be established and the conditions (clinical criteria and/or complementary tests) for doing so. The authors answered these questionnaires, followed by comments and discussions via e-mail to further clarify discrepancies and the poorly defined or the most controversial questions. The results of all this information flow were used to define the key questions best suited for answering the most representative aspects of the diagnosis of asthma in preschool children. Following the definition of the key questions (Table 1) and selection of the guidelines, these were distributed in such a way that each guide was analyzed with two reviewers answering the key questions independently. The answers of the evaluators were forwarded to the coordinator. When the answer to a key question given by the two reviewers was identical or similar, the answer was taken to be valid. If the answer was not sufficiently homogeneous, the coordinator stated his personal opinion in an attempt to reach collective consensus. The aim was to secure acceptance by all the reviewers of the key questions referred to each document, if possible. The authors were required to confirm their final agreement with the result reflected in the present article.
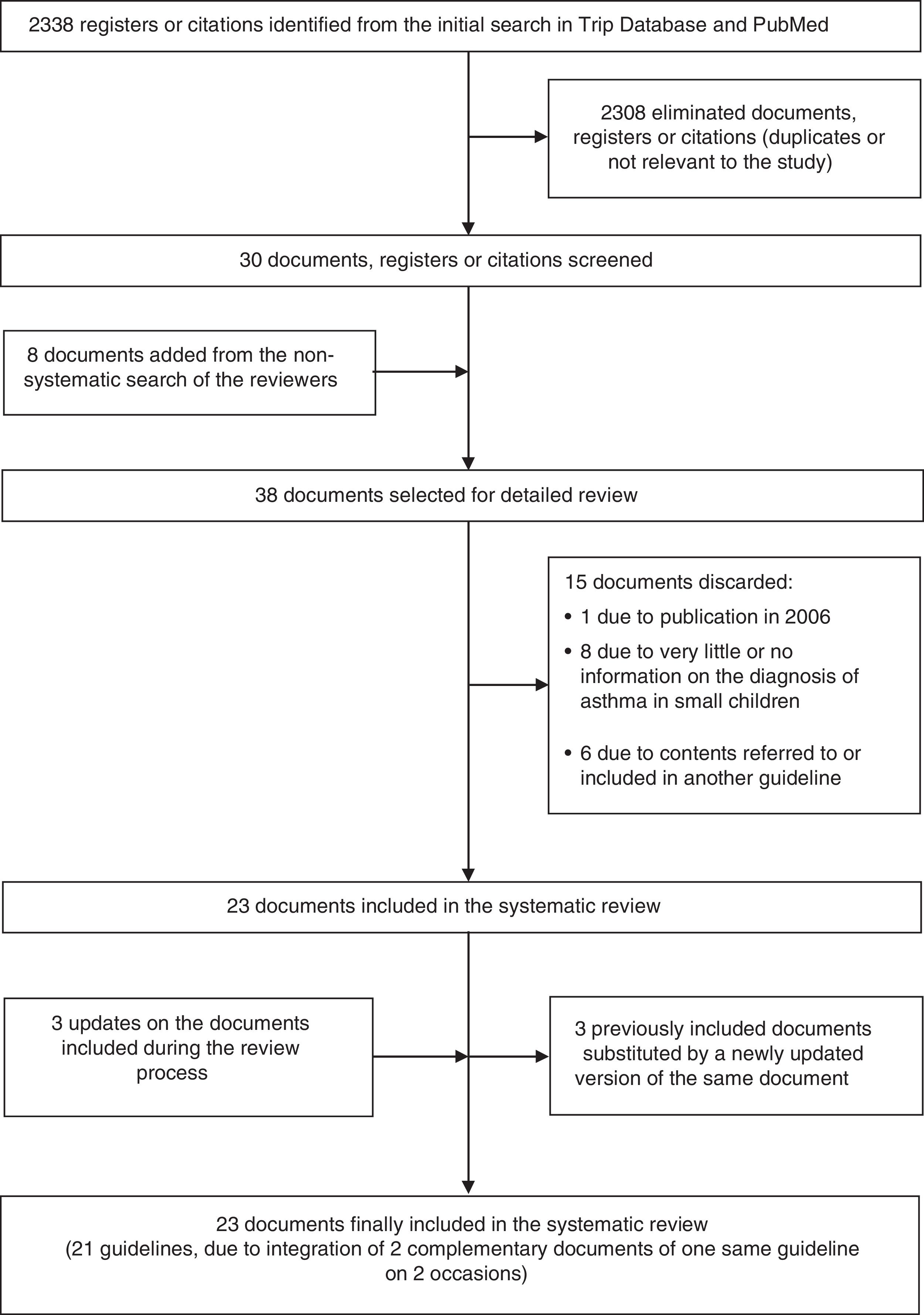
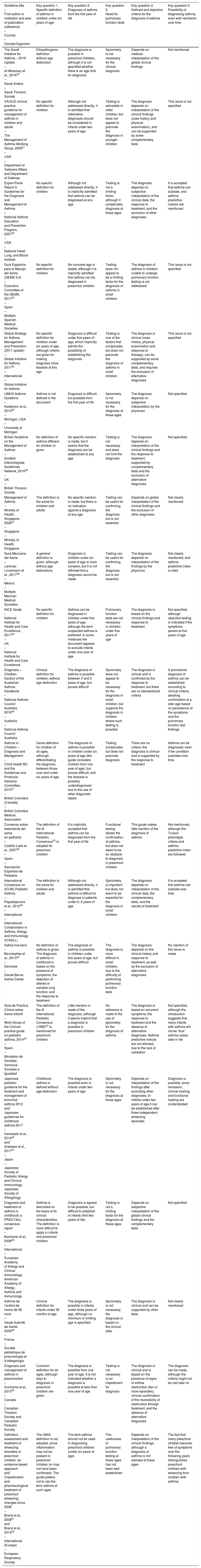
ResultsA total of 2338 references were obtained from the initial search in Trip Database and PubMed. The selection process of the valid documents is shown in Fig. 1. Finally, 23 documents grouped into 21 clinical guidelines were analyzed, since two of the guidelines were considered to be comprised by two different documents that were judged to be complementary. The selected guidelines, the constituting documents, and the answers of the guidelines to the key questions are summarized in Table 2. Ten of the selected guidelines were referred to patients of all ages; eight were pediatric guidelines; and three were exclusively focused on preschool children.
Guidelines selected for offering information referred to the concept or diagnosis of asthma in childhood, including the first years of life (infants and preschool children), and their answers to the key questions.
| Guideline title – First author or institution and year of publication (reference) – Country – Society/Organism | Key question 1. Specific definition of asthma in children under six years of age | Key question 2. Diagnosis of asthma from the first year of life | Key question 3. Need for pulmonary function tests | Key question 4. Defined and objective criteria for the diagnosis of asthma | Key question 5. Possibility of diagnosing asthma, even with remission over time |
|---|---|---|---|---|---|
| The Saudi Initiative for Asthma – 2016 Update – Al-Moamary et al., 201630 – Saudi Arabia – Saudi Thoracic Society | Etiopathogenic definition without age distinction | The diagnosis is possible in preschool children, although it is not specified whether there is an age limit for diagnosis | Spirometry is not necessary for the clinical diagnosis | Depends on medical interpretation of the global clinical findings | Not mentioned |
| VA/DoD clinical practice guideline for management of asthma in children and adults – The Management of Asthma Working Group, 200931 – USA – Department of Veterans Affairs and Department of Defense | No specific definition for children | Although not addressed directly, it is admitted that alternative diagnoses should be considered in infants under two years of age. | Testing is advisable in older children, but does not appear to preclude the diagnosis in younger children | The diagnosis depends on interpretation of the clinical findings (case history and physical examination), and can be supported by some complementary tests | This issue is not specified |
| Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma – National Asthma Education and Prevention Program, 200732 – USA – National Heart, Lung, and Blood Institute | No specific definition for children | Although not addressed directly, it is implicitly admitted that asthma can be diagnosed at any age | Testing is not a limiting factor, although it complicates diagnosis at these ages | The diagnosis depends on subjective interpretation of the clinical data, the response to treatment, and the exclusion of other diagnoses | It is accepted that asthma can subside, and asthma predictive indices are mentioned |
| Guía Española para el Manejo del Asma (GEMA 4.2) – Executive Committee of the GEMA, 201733 – Spain – Multiple Spanish Medical Societies | No specific definition for children | No concrete age is stated, although it is implicitly admitted that asthma can be diagnosed in preschool children | Testing does not appear to be a limiting factor for the diagnosis of asthma in small children | The diagnosis of asthma in children unable to undergo pulmonary function testing is not addressed | This issue is not specified |
| Global Strategy for Asthma Management and Prevention (2017 update) – Global Initiative for Asthma, 201734 – International – Global Initiative for Asthma | No specific definition for children under six years of age, although criteria are given for making diagnosis more feasible at this age | Diagnosis is difficult under five years of age, which implicitly admits the possibility of establishing the diagnosis | Testing is one of the factors that complicates but does not preclude the diagnosis of asthma in small children | The diagnosis is clinical (case history, physical examination and response to therapy), can be supported by some complementary tests, and requires the exclusion of alternative diagnoses | This issue is not specified |
| UMHS Asthma Guideline – Kesterson et al., 201035 – Michigan, USA – University of Michigan | Asthma is not defined in the document | Diagnosis is difficult but possible from the first year of life | Spirometry is not necessary for the diagnosis at these ages | The diagnosis depends on subjective interpretation by the physician | Not specified |
| British Guideline on the Management of Asthma – Scottish Intercollegiate Guidelines Network, 201636 – UK – British Thoracic Society | No definition of asthma different for children is given | No specific mention is made, but it seems that the diagnosis can be established at any age | Testing is not necessary and does not limit the diagnosis | The diagnosis depends on interpretation of the clinical findings and the response to treatment, supported by complementary tests and the exclusion of alternative diagnoses | Not specified |
| Management of Asthma – Ministry of Health, Singapore, 200837 – Singapore – Ministry of Health, Singapore | The definition is the same for children and adults | No specific mention is made, but there is no indication against a diagnosis at any age | Testing can be useful for confirming the diagnosis, but is not essential | Depends on global interpretation of the clinical findings and the exclusion of other diagnoses | Not clearly mentioned |
| Guía Mexicana del Asma – Larenas-Linnemann et al., 201738 – Mexico – Multiple Mexican Medical Societies | A general definition is given, although without age distinctions | Diagnosis in children under six years of age is more complex, but it is not affirmed that a diagnosis cannot be made | Testing can be useful for confirming the diagnosis, but is not essential | The diagnosis depends on interpretation of the findings by the physician | Not clearly mentioned, and asthma predictive index is cited |
| NICE Guide – National Institute for Health and Care Excellence, 201739 – UK – National Institute for Health and Care Excellence | No specific definition for children | Asthma can be diagnosed in children under five years of age, although the term suspected asthma is preferred. In some instances the document appears to exclude infants under one year of age | Pulmonary function tests are not necessary in children under five years of age | The diagnosis is based on the clinical findings and response to treatment | Not specified, although objective testing is indicated if the symptoms persist at five years of age |
| Diagnosis – Children Section of the Australian Asthma Handbook – National Asthma Council Australia, 201640 – Australia – National Asthma Council Australia | Clinical definition for children, without age distinction | The diagnosis of asthma is possible between 0 and 5 years of age, but proves difficult | Spirometry does not appear to be necessary for the diagnosis in small children, but supports the diagnosis in children where such testing is possible | The diagnosis is clinical and is confirmed by the response to treatment, but there are no standardized criteria | A provisional diagnosis of asthma can be established according to clinical criteria, awaiting confirmation at a later age based on persistence of the symptoms and the pulmonary function test findings |
| Asthma in Children – Diagnosis and Management – Child Health BC and the Guidelines and Protocols Advisory Committee, 201541 – British Columbia (Canada) – British Columbia Medical Association | Same definition for children of all ages, although differentiating the diagnosis between those over and under six years of age | The diagnosis of asthma is possible in children under six years of age (the guide considers children from one year of age), but proves difficult, and the disease is possibly underdiagnosed due to the use of other diagnostic labels | Testing complicates but does not preclude diagnosis | There are no criteria; the diagnosis is clinical and is supported by the response to treatment | Asthma can be diagnosed, even if the condition subsides over time |
| Consenso sobre tratamiento del asma en pediatría – Castillo Laita et al., 200742 – Spain – Asociación Española de Pediatría | The definition of the III International Pediatric Consensus53 is adopted for preschool children | It is implicitly accepted that asthma can be diagnosed from the first year of life | Functional testing allows the confirmation of asthma, but does not seem to be an obstacle to diagnosis in preschool children | This guide makes little mention of the diagnosis of asthma | Not mentioned, although the Tucson phenotype criteria and asthma predictive index are followed |
| International Consensus on (ICON) Pediatric Asthma – Papadopoulos et al., 201243 – International – International Collaboration in Asthma, Allergy and Immunology (iCAALL) | The definition is the same for children and adults | Although not addressed directly, it is admitted that asthma is difficult to diagnose in patients under 2–3 years of age | Spirometry is important but does not seem to be essential for the diagnosis in small children | The diagnosis depends on interpretation of the clinical data, the complementary tests, and the results of treatment | It is accepted that asthma can subside over time |
| Astma hos børn – Bønnelykke et al., 201344 – Denmark – Dansk Børne Astma Center | No definition of asthma is given. The diagnosis of asthma in childhood is based on the presence of symptoms, the detection of altered or variable lung function, and the response to treatment | The diagnosis of asthma is possible in children under five years of age, but proves difficult | The diagnosis is more difficult in small children, due to the difficulty of performing pulmonary function tests | The diagnosis depends on the clinical history and response to treatment, as well as the exclusion of alternative diagnoses | No mention of this issue is made |
| Guía de Práctica Clínica sobre Asma Infantil – Work Group of the Clinical practice guide on pediatric asthma, 201445 – Spain – Ministerio de Sanidad, Servicios Sociales e Igualdad | The definition of the III International Pediatric Consensus (1998)53 is mentioned for preschool children | Little mention is made of the diagnosis, although it seems implicit that a diagnosis is possible in preschool children | No reference is made to the use of spirometry for the diagnosis of asthma | The diagnosis is based on recurrent symptoms, the response to treatment and the absence of alternative diagnoses. Asthma predictive indices are not advised, due to the lack of validation | Not specified, although the introduction suggests that many infants with asthma will not be “true” asthma cases later in life |
| Japanese pediatric guideline for the treatment and management of bronchial asthma 2012 and* Japanese guidelines for childhood asthma 2017 – Hamasaki et al., 201446 and* Arakawa et al., 201747 – Japan – Japanese Society of Pediatric Allergy and Clinical Immunology; Japanese Society of Allergology | Childhood asthma is defined without age distinction | The diagnosis is possible even in infants under two years of age | Spirometry is not necessary for the diagnosis at these ages | Depends on interpretation of the findings after excluding other diagnoses. In infants under two years of age it can be established after three independent wheezing episodes | Diagnosis is possible, since remission, clinical healing and functional healing are contemplated |
| Diagnosis and treatment of asthma in childhood: a PRACTALL consensus report – Bacharier et al., 200848 – International – European Academy of Allergy and Clinical Immunology; American Academy of Allergy, Asthma and Immunology | Asthma is described on the basis of its clinical characteristics. The definition is more difficult to apply in infants and preschool children | Diagnosis is agreed to be possible, but difficult to establish in infants (first two years of life) | Testing is not a limiting factor for the diagnosis at these ages | Depends on subjective interpretation of the global clinical findings and the complementary tests | Not specified |
| Asthme de l’enfant de moins de 36 mois – Haute Autorité de Santé, 200949 – France – Société pédiatrique de pneumologie et d’allergologie | Clinical definition for infants under 36 months of age | The diagnosis is possible in infants under three years of age, although no minimum or limiting age is specified. | Spirometry is not necessary; the diagnosis is based on the clinical data | The diagnosis is clinical and can be supported by other tests | Not clearly mentioned |
| Diagnosis and management of asthma in preschoolers – Ducharne et al., 201550 – Canada – Canadian Thoracic Society and Canadian Pediatric Society | Common definition for all ages, although keys to diagnosis in preschool children are given | The diagnosis is possible from one year of age. It is not indicated whether a diagnosis is possible at less than one year of age | Testing is not necessary or an impediment for diagnosis | The diagnosis is clinical and is based on the presence of signs of airflow obstruction (two or more episodes), clinical confirmation of the reversibility of obstruction through treatment, and the absence of alternative diagnoses | The diagnosis can be made, although the criteria might not be met later on |
| Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach and* Classification and pharmacological treatment of preschool wheezing: changes since 2008 – Brand et al., 200851 and* Brand et al., 201452 – International (Europe) – European Respiratory Society | The GINA definition is not adopted, since inflammation may not be present in preschool children (or may not have been confirmed). The guide prefers not to use the term asthma at such ages | The term asthma should not be used in diagnosing preschool children (under six years of age) | The usefulness of pulmonary function testing at these ages has not been well established | Depends on interpretation of the clinical findings, although a diagnosis of asthma is not advised at these ages | The fact that many preschool children become free of symptoms over the following years distinguishes preschool children with wheezing from children with asthma |
The first 10 documents are general guidelines (children and adults); the following eight are pediatric guidelines; and the last three are focused only on preschool children.
The guidelines were generally quite narrative in addressing the concept and diagnosis of asthma. It was therefore difficult to draw clear definitions and diagnostic criterions. Most of the guidelines did not offer explicit answers to the key questions. The answers were found in different sections of the guidelines and could even be interpreted as contradictory within one same document. Table 2 shows the consensus results of the group in summarizing the answers to the key questions.
In most of the guidelines, the concept and definition of asthma were closely related or implicit to the diagnosis of the disease. The general guidelines made no distinction between adults and children in defining asthma. Although most of the pediatric guidelines (including preschool children) defined asthma without distinctions according to age with a view fundamentally oriented by the clinical manifestations, some of them did distinguish between preschool children and older children – particularly when addressing the diagnosis, which was considered to be more difficult in preschool children. The two Spanish pediatric guidelines analyzed made reference to the III International Pediatric Consensus to define asthma in preschool children.53
Most of the guides implicitly recognize that there is no age limit for establishing a diagnosis of asthma, although they underscore the difficulty of establishing a diagnosis in children under 5–6 years of age, and particularly in infants under 2–3 years of age. Only the document of the European Respiratory Society (ERS) on wheezing disorders in preschool children recommends avoiding the term asthma in children under six years of age and considers that the diagnosis cannot be established in patients under that age. In the analyzed guides, spirometry was not considered essential for establishing the diagnosis in preschool children, although the difficulty of performing pulmonary function tests in such young children complicates confirmation of the diagnosis. According to most of the guidelines, the diagnosis of asthma in preschool children is based on subjective physician interpretation of the clinical findings (more than 2–3 bronchial obstruction episodes), the response to treatment (immediate response to bronchodilators or delayed response to inhaled corticosteroids), and the exclusion of other alternative diagnoses. Complementary tests may be added to support or rule out the diagnosis. Many of the guides emphasize the importance of confirming wheezing – a key sign of the asthmatic process – through auscultation.
The ERS guideline on wheezing disorders in preschool children is the clearest document stating that the fact that many preschool children become free of symptoms over time is what distinguishes preschool wheeze from the more persistent asthma. Most of the guidelines fail to address this issue, although some do accept that asthma can subside over time (e.g., the International consensus on [ICON] pediatric asthma and the Japanese guideline), and that this consequently would not impede establishing a diagnosis. Many of the guidelines refer to the phenotypes of preschool children with wheezing/asthma and to the predictive indices of asthma persistence into school-age, although they lack accuracy so they are not indicated or are even not considered useful for diagnosing asthma in preschool children.
DiscussionThe concept and diagnosis of asthma is an unresolved issue affecting patients of all ages, although it is particularly relevant in childhood since this is the period in life when most patients develop the disease. The concept of asthma has gradually broadened and become more diffuse. It is presently understood to be a heterogeneous disease or a complex syndrome – this being an umbrella term encompassing patients with similar clinical manifestations but with a diverse or uncertain etiopathogenesis.3,4 The ambiguity of this concept has led some authors to consider it to be useless, and therefore propose its elimination.54 However, the term asthma remains necessary in designating patients with symptoms attributable to variable bronchial obstruction, at least when no alternative diagnosis can be established, capable of more precisely describing the process underlying the symptoms.
Many children present symptoms consistent with asthma in the first years of life, and the course of the disorder over the subsequent years is highly variable, making it difficult to predict persistence or remission with sufficient reliability. Therefore, and since the physiopathological basis underlying each individual patient is not known, it has been difficult to establish a diagnosis of asthma in patients of this age. However, as the concept of asthma broadens and the clinical features gain a more prominent role versus the underlying etiopathogenic processes or the subsequent course of the disorder, many of the obstacles facing diagnosis in this population of small children are eliminated. The present review has shown that most of the clinical guidelines on asthma implicitly accept that the diagnosis can be established in preschool children, with no lower age limit. A recent study has observed a progressive decrease in the age at diagnosis of asthma in preschool children.55
The guidelines usually base the diagnosis of asthma in preschool children on the reiterated presence of compatible symptoms (several episodes of bronchial obstruction, preferably witnessed by the physician), adequate response to treatment, and the exclusion of other alternative diagnoses. Thus, diagnosis at these ages is fundamentally of a clinical nature, subjectively established by the clinician, and as such should be regarded as amenable to revision, since other more precise diagnoses may be established when justified by further data. Complementary tests (imaging studies, allergy work-up, specific tests for alternative diseases) play a secondary role, contributing indirect data in favor of, or against a diagnosis of asthma or of other disorders. Asthma predictive indices offer poor precision and are likewise not considered useful.56,57 Pulmonary function tests are not regarded as necessary at these ages, since they are difficult to perform, and studies evaluating their usefulness are lacking. The study of pulmonary function can contribute to the diagnosis of asthma in older children, when patient collaboration in forced spirometry can be secured. In some cases, such collaboration is even possible in children from three years of age.58–60 Nevertheless, the usefulness of pulmonary function studies in establishing the diagnosis of asthma has been questioned even in older children and adolescents.61 Another systematic review of the diagnostic criteria of asthma in clinical guidelines also detected discrepancies regarding the need for objective lung function tests in order to establish a diagnosis of asthma in both adults and children.28
It is well known that many young children improve and become symptom-free over time, although it is difficult to precisely predict such improvement or to know whether the disease can reappear after remission.62,63 Only the Japanese guideline clearly speaks of remission (absence of symptoms during one year), clinical healing (absence of symptoms during five years) or functional healing (clinical healing and normal pulmonary function test results). On the other hand, only the ERS document on wheezing disorders in preschool children deviates from the preponderant view and considers that the term “asthma” cannot be used in preschool children with wheezing episodes that can disappear over time. It thus defends a fundamentally etiopathogenic vision of asthma (chronic inflammation of the airway that cannot be confirmed at these ages), versus the much more usual view based on clinical manifestations.
It should be mentioned that the information referred to the concept of asthma was not always contained or well defined in the analyzed guidelines, and that some made very little mention of the diagnostic process. It is notorious that while treatment was one of the main objectives of the guidelines, the lack of definition made it difficult to know to what patient population treatment was targeted. It therefore proved complicated to offer simple answers to the established questions, and in many cases indirect conclusions had to be drawn in order to answer them. This element of subjectiveness in interpretation may have been a principal limiting element in our review, and we attempted to overcome it through the participation of several reviewers with expertise in childhood asthma. Another possible limitation is the exclusion of guidelines that could not be retrieved from the databases or through personal searches by the reviewers. There undoubtedly may be more guidelines on asthma, particularly at a national level. However, we feel that the selected documents are the most significant and best-known guidelines, and that those which could not be obtained with our strategy were probably few and were unlikely to afford relevant information different from that analyzed in the present review.
The results of this review are supported by the very recent report of a Commission publishing its vision of how asthma should be understood and studied in order to overcome the apparent lack of advances in the last 10 years.64 The first of its recommendations has been to “use asthma solely as a descriptive label for a collection of symptoms. We make no assumptions about physiopathology. The label asthma thus becomes the start, not the end, of the diagnostic and therapeutic process.” This vision allows expansion of the syndromic concept of asthma at all ages, thereby eliminating the previous difficulties in establishing a diagnosis of asthma in preschool children. Neither lung function nor the physiopathological substrate or the persistence of symptoms are necessary to establish a diagnosis equivalent to describe an airway disease that must be “deconstructed into components or treatable traits” in each individual patient. This need to individualize treatment has been the subject of many studies seeking to define phenotypes and endotypes among asthmatic patients,65 although further research is needed in order to determine their usefulness in orienting treatment,66,67 which continues to largely depend on a trial and error approach.
In conclusion, most of the guidelines consider that asthma can be diagnosed in preschool children provided that the clinical condition is compatible with the disease, the response to treatment is adequate, and other possible diagnoses have been ruled out. This diagnosis would be the starting point for deconstructing the observable features (phenotype) and the genetic and environmental factors (endotypes) intervening in each patient, or until a more precise alternative diagnosis can be established (e.g., cystic fibrosis, tracheobronchomalacia or vascular ring, to mention just a few possibilities). From the clinical perspective, the diagnosis of asthma in preschool children is established by the physician in charge of the patient and involves a series of peculiarities inherent to patients of this age, such as limitations for performing pulmonary function tests, greater attention to differential diagnoses, limited response to common asthma treatments, and a high probability of symptoms remission during childhood. It would be advisable to reach a general consensus on the concept of asthma and thus avoid the use of other diagnostic labels such as “wheezing” (which may be useful for questionnaire-based epidemiological studies) or “reactive airways disease”,68 which can lead to confusion. The study of the factors participating in asthma among preschool children is crucial for improving treatment and for better understanding asthma and airway disease in adult life and old age.
Ethical disclosuresConfidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the corresponding Clinical Research Ethics Committee and with the guidelines of the World Medical Association and the Declaration of Helsinki.
Conflict of interestThe authors have no conflict of interest.
We thank Agustín Acuña Izcaray for help in the systematic search of asthma clinical guidelines, and Ulla Aguilera Jacobsen for the Spanish translation of diagnostic aspects of the Danish guideline of asthma in children.