Recurrent wheezing during the first year of life is a major cause of respiratory morbidity worldwide, yet there are no studies on its prevalence in Portugal.
ObjectiveDetermine the prevalence and severity of recurrent wheezing, treatments employed and other related aspects, in infants during their first year of life in Setúbal, Portugal.
MethodsThis is a cross-sectional study of a random sample of infants aged 12–15 months living in Setúbal district. It uses a validated questionnaire answered by parents/caregivers at local healthcare facilities where infants attend for growth/development monitoring and/or vaccine administration.
ResultsAmong the 202 infants surveyed, 44.6% (95% CI 37.7–51.4) had at least one episode of wheezing; and 18.3% (95% CI 12.9–23.6) had recurrent wheezing. There was significant morbidity associated to recurrent wheezing in terms of severe episodes (17.3%–95% CI 12–22.5), visits to the emergency department (26.2%–95% CI 20.1–32.2) and hospital admissions (5.4%–95% CI 2.2–8.5); 10.4% (95% CI 6.1–14.6) used inhaled corticosteroids and 7.9% (95% CI 4.1–11.6) used a leukotriene receptor antagonist.
ConclusionsThe prevalence of recurrent wheezing in infants during the first year of life is high and is associated with significant morbidity, presenting as a relevant public health problem. An important proportion of infants’ progress with a more severe condition, resulting in high use of health resources (visits to emergency department and hospitalisations). The prevalence of recurrent wheezing in this district of Portugal stays between those related in other European and Latin American Centres, suggesting that maybe some of the well-known risk factors are shared with affluent countries.
Recurrent wheezing (RW) in infancy is a very common condition and causes significant use of healthcare facilities, and is usually associated with severe progression and co-morbidities.1 The prevalence of RW in infants during the first year of life in Latin America and Europe is high, as found by large international cross-sectional, population-based surveys,1,2 although the mean prevalence of RW in Latin American in comparison with European centres is higher. In Spain, the mean prevalence of RW was found to be 15.1% versus 21.4% in Latin America, with a mean prevalence in Brazilian centres of 26%.1 Recently, a survey including 11 centres in different Latin American countries showed that prevalence of RW during the first year of life ranged from 7.5% to 26.4%.2 In a study of children aged 1–5 years from the USA and Europe it was found that 32% suffered from recurrent asthma-like symptoms.3 Differences in prevalence of RW given by ethnic characteristics have been reported in the UK where the prevalence of wheezing (one or more episodes) in one-year olds was 25.5% in South Asians and 35.6% in white infants.4 The prevalence of RW in infants is increased in low-resourced populations, which has been found when comparing Spanish centres with Latin American centres1,5 but to the best of our knowledge there is no information on RW in infants during the first year of life in Portugal which could be useful when interpreting data on RW from Brazilian centres. In preschool children, Pereira et al. have recently reported a prevalence of RW (four or more episodes) in Portugal of 9.4%, however, this figure involves children aged 3–5 years and not infants in their first year of life.6 It is during the first year of life when the occurrence of frequent and severe wheezing episodes is related with early lung function impairment, asthma and COPD later in childhood and adulthood.7,8 The hypothesis of the EISL study (from the Spanish “Estudio Internacional de Sibilancias en Lactantes” or International Study of Wheezing in Infants, in English) is that the prevalence of RW during the first year of life is high and as variable as the prevalence of asthma symptoms in older children and differs between affluent and non-affluent countries.1 Herein, we describe the findings of the aforementioned study, which was performed with a standardised methodology and a validated questionnaire9,10 in Setúbal district, Portugal.
MethodsThis study is part of EISL (from the Spanish “Estudio Internacional de Sibilancias en Lactantes” or International Study of Wheezing in Infants, in English) and was undertaken in the district of Setúbal, Portugal during the year 2015. It was coordinated with the consent of the district's Healthcare Centres Grouping (ACES); the instrument was applied in randomly selected local healthcare facilities. According to Arrábida ACES, the district's total number of infants aged 12 months in the year 2015 was 1800.
We used the EISL questionnaire, Portuguese version which has been previously validated9 and include questions on frequency and severity of wheezing and on protective/risk factors for wheezing. The main objective of our study is to determine the prevalence of RW in the first year of life (defined as three or more parent-reported wheezing episodes during that time), using a validated questionnaire.10 The questionnaire includes questions on wheezing, common cold or upper respiratory tract infection (URTI), treatment modalities as inhaled bronchodilators (BD), inhaled corticosteroids (ICS) and leukotriene receptor antagonists (LTRA); severe episodes, sleep disturbance, emergency department (ED) visits and admissions to hospital due to wheezing, among others. The questions on wheezing had been previously validated against physician-diagnosed wheezing (general paediatricians and paediatric pulmonologists), in centres from Latin America (Spanish and Portuguese speaking countries) and Spain.9,10 The Portuguese version of the questionnaire was translated from Spanish into Portuguese and back-translated from Portuguese into Spanish. The Portuguese questionnaire from Brazil was adapted to European Portuguese to correspond to the current language used in Portugal, with more familiar terms. The sample size was estimated from the total population of infant aged one year living in Setúbal district during the survey (1.800) and with a confidence level of 95%, an expected proportion of infants with RW of 0.15, and using a 0.1 width of confidence interval, the estimated sample size was 214 infants.
After randomly selecting the participating localities in the target district of Setúbal, questionnaires were delivered by field workers to parents/caregivers for their completion when infants were taken to the local health units for vaccination at the age of 12 months, until completing the required sample. The study had the approval of the local Ethics Committee and had the support and permission of the local governmental authorities of health.
Parents or guardians who accepted to participate in the study filled in the questionnaire after reading and signing a full-informed written consent.
Data analysisData were analysed by means of statistical software (SPSS v13, Chicago, IL, USA; and MedCalc Statistical Software version 17.9.6, Ostend, Belgium) using descriptive statistics: results are expressed as proportions and 95% confidence intervals.
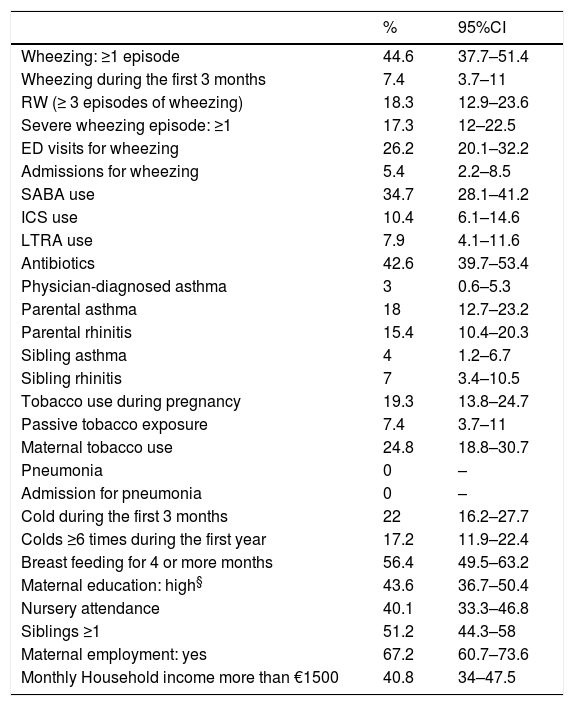
ResultsThe mean age for the whole sample of infants (51.3% female) was 12.3 months; the proportion of questionnaires filled out by the mothers was 86.1%, whereas by fathers and guardians was 13.9%; the response rate was 94%. Data on the prevalence for the different variables are presented in Tables 1 and 2.
Prevalence rates (%) of variables related to wheezing during the first year of life in the whole sample of infants from Setúbal, Portugal.
| % | 95%CI | |
|---|---|---|
| Wheezing: ≥1 episode | 44.6 | 37.7–51.4 |
| Wheezing during the first 3 months | 7.4 | 3.7–11 |
| RW (≥ 3 episodes of wheezing) | 18.3 | 12.9–23.6 |
| Severe wheezing episode: ≥1 | 17.3 | 12–22.5 |
| ED visits for wheezing | 26.2 | 20.1–32.2 |
| Admissions for wheezing | 5.4 | 2.2–8.5 |
| SABA use | 34.7 | 28.1–41.2 |
| ICS use | 10.4 | 6.1–14.6 |
| LTRA use | 7.9 | 4.1–11.6 |
| Antibiotics | 42.6 | 39.7–53.4 |
| Physician-diagnosed asthma | 3 | 0.6–5.3 |
| Parental asthma | 18 | 12.7–23.2 |
| Parental rhinitis | 15.4 | 10.4–20.3 |
| Sibling asthma | 4 | 1.2–6.7 |
| Sibling rhinitis | 7 | 3.4–10.5 |
| Tobacco use during pregnancy | 19.3 | 13.8–24.7 |
| Passive tobacco exposure | 7.4 | 3.7–11 |
| Maternal tobacco use | 24.8 | 18.8–30.7 |
| Pneumonia | 0 | – |
| Admission for pneumonia | 0 | – |
| Cold during the first 3 months | 22 | 16.2–27.7 |
| Colds ≥6 times during the first year | 17.2 | 11.9–22.4 |
| Breast feeding for 4 or more months | 56.4 | 49.5–63.2 |
| Maternal education: high§ | 43.6 | 36.7–50.4 |
| Nursery attendance | 40.1 | 33.3–46.8 |
| Siblings ≥1 | 51.2 | 44.3–58 |
| Maternal employment: yes | 67.2 | 60.7–73.6 |
| Monthly Household income more than €1500 | 40.8 | 34–47.5 |
RW, recurrent wheezing; SABA, inhaled short-acting beta two agonists; ICS, inhaled corticosteroids; LTRA, leukotriene receptor antagonists.
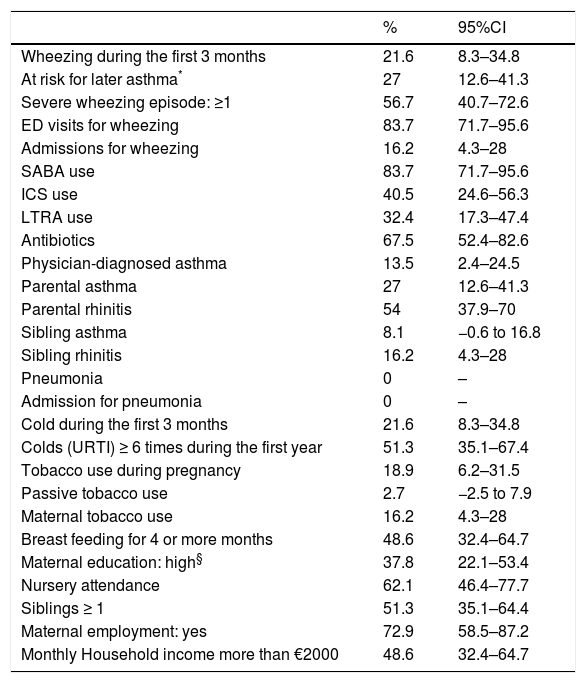
Prevalence of variables related to wheezing during the first year of life in infants with RW in Setúbal, Portugal.
| % | 95%CI | |
|---|---|---|
| Wheezing during the first 3 months | 21.6 | 8.3–34.8 |
| At risk for later asthma* | 27 | 12.6–41.3 |
| Severe wheezing episode: ≥1 | 56.7 | 40.7–72.6 |
| ED visits for wheezing | 83.7 | 71.7–95.6 |
| Admissions for wheezing | 16.2 | 4.3–28 |
| SABA use | 83.7 | 71.7–95.6 |
| ICS use | 40.5 | 24.6–56.3 |
| LTRA use | 32.4 | 17.3–47.4 |
| Antibiotics | 67.5 | 52.4–82.6 |
| Physician-diagnosed asthma | 13.5 | 2.4–24.5 |
| Parental asthma | 27 | 12.6–41.3 |
| Parental rhinitis | 54 | 37.9–70 |
| Sibling asthma | 8.1 | −0.6 to 16.8 |
| Sibling rhinitis | 16.2 | 4.3–28 |
| Pneumonia | 0 | – |
| Admission for pneumonia | 0 | – |
| Cold during the first 3 months | 21.6 | 8.3–34.8 |
| Colds (URTI) ≥ 6 times during the first year | 51.3 | 35.1–67.4 |
| Tobacco use during pregnancy | 18.9 | 6.2–31.5 |
| Passive tobacco use | 2.7 | −2.5 to 7.9 |
| Maternal tobacco use | 16.2 | 4.3–28 |
| Breast feeding for 4 or more months | 48.6 | 32.4–64.7 |
| Maternal education: high§ | 37.8 | 22.1–53.4 |
| Nursery attendance | 62.1 | 46.4–77.7 |
| Siblings ≥ 1 | 51.3 | 35.1–64.4 |
| Maternal employment: yes | 72.9 | 58.5–87.2 |
| Monthly Household income more than €2000 | 48.6 | 32.4–64.7 |
It was found that 44.6% (95% CI 37.7-51.4) wheezed at least once during their first year of life; 18.3% (95% CI 12.9–23.6) had RW; and 7.4% (95% CI 3.7–11.0) of infants had their first episode of wheezing during the first three months of life.
Parental history of asthma was reported in 18% (95% CI 12.7–23.2) of infants, whereas in children with RW it was reported in 27% (95% CI 12.6–41.3). Reported physician-diagnosed asthma was 3% (95% CI 0.6–5.3) and, in children with RW, 13.5% (95% CI 2.4–24.5).
The prevalence of the severity markers of wheezing (severe episodes, visits to ED and hospital admissions) was as follows: 17.3% (95% CI 12–22.5), 26.2% (95% CI 20.1–32.2) and 5.4% (95% CI 2.2–8.5), respectively.
Sleep disturbance, with frequent arousals (two or more per week for most of the months) due to cough or wheezing was reported in 21.3% (95% CI 12.7–29.8).
The reported use of ICS in infants with RW during the first year of life was 40.5% (95% CI 24.6–56.3); in RW infants the prevalence of admissions, visits to ED was 16.2% (95% CI 4.3–28) and 83.7% (95% CI 71.7–95.6), respectively.
Antibiotic use in the whole sample was found in 42.6% (95% CI 39.7–53.4), and in 67.5% (95% CI 52.4–82.6) of RW children.
DiscussionThis is the first study on the prevalence of RW during the first year of life in Portugal. We have found that, as previously reported,1 the prevalence of RW was high with a significant proportion of infants with RW suffering from sleep disturbance, severe episodes, ED visits and admissions to hospital.
In addition to verifying the prevalence of wheezing in the first year of life in a district in Portugal, the study allowed us to relate this prevalence with those found in studies conducted in other centres, with the application of the same EISL methodology. By filling out the questionnaire, data were obtained on variables that, in the future, with a larger sample, will let us identify regional risk factors for RW.
Few data on asthma prevalence in children are available in Portugal. Standardised methodology on asthma prevalence is limited for ages 6–7 and 13–14 years old in the International Study of Asthma and Allergies in Childhood (ISAAC). The ISAAC study in Portugal assessed the prevalence of asthma in four cities. For children aged 6–7 years old the global prevalence of asthma in the last 12 months was 13%; for teenagers (13–14 years old) the global prevalence of current asthma ranged between 9% in 1995 and 12% in 2002.11
The first Portuguese National Asthma Survey estimated the prevalence of current asthma in the Portuguese population. The global prevalence in children and adolescents under 18 years old was 12.4%.12 The stratification of prevalence in other age groups, including pre-schoolers and infants, was not presented.
A nationwide, population-based study, including a representative sample of Portuguese children aged 3–5 years old, verified the presence of ≥1 episode of wheezing in the last 12 months. The prevalence of current wheezing was 24.5% (95% CI 23.3–25.7), 9.4% of participants had ≥4 episodes of wheezing in the previous year and less than 5% reported having a medical diagnosis of asthma.6 The findings of Pereira et al. and ours would suggest that asthma is being underdiagnosed in young children, which could have important consequences for the classification and proper management of the condition.
The wheezing prevalence, characteristics (frequency, severity) and risk factors in infants under the age of 12 months cannot be extrapolated from studies with older children. During the first year of life, a high proportion of infants with RW have severe episodes resulting in an elevated frequency of visits to the ED and hospital admissions for wheezing.13 Our results also demonstrated that RW in infants is not a benign condition as usually considered, independently of how it will progress later in childhood or adolescence.
The Spanish and Portuguese versions of the EISL written questionnaire, validated in different settings, have shown good agreement between objective physical examination and wheezing reported by parents/caregivers of 12–15-month-old infants.9,10 The questionnaire has also proved to be a reliable means of obtaining data on wheezing in the first year of life, with high sensitivity, specificity, positive predictive values (PPVs), and negative predictive values (NPVs).9,10
An international population-based study was performed in random samples of infants aged 12–15 months from 17 centres in Latin America and Europe. Among the 30,093 infants surveyed, they found that the prevalence of RW during the first year of life varied between localities and is lower and less severe in European than in Latin American (LA) centres, suggesting that there is a higher risk for the disease in developing areas.1 The prevalence of RW in Brazil ranged from 21.9% to 36.3% and the mean prevalence in LA was 21.4% (95% CI 20.9–21.9).1 On the other hand, the mean prevalence in Europe (four centres in Spain and one in The Netherlands) was 15% (95% CI 14–15.9).1 In Setúbal, the RW prevalence, 18.3% (95% CI 12.9–23.6), overlapped only with one Spanish centre and was higher than the others in Europe.
A more recent study included 12,405 infants from 11 centres in six LA countries (Argentina, Brazil, Chile, Colombia, Peru and Uruguay). The RW prevalence ranged from 7.5% to 26.4% and the mean prevalence was 16.6% (95% CI 16.0–17.3).2 The analysis did not include some Brazilian centres that had higher prevalence in the previous study. Data obtained from two surveys administered seven years apart were used to identify changes in the prevalence and severity of recurrent wheezing (RW) in infants in three large LA cities: Curitiba (Brazil), São Paulo (Brazil), and Santiago (Chile).14 The prevalence and severity of RW during the first year of life remained high over time, with remarkably high rates of ED visits, admissions for wheezing and use of asthma medications.
There was a wide and significant variability in the prevalence, severity markers and use of medications between the centers.2
In fact, the EISL methodology was applied in many more centres in LA than in Europe. It seems, however, that the prevalence of RW in this district of Portugal stays between those related in other European and in LA centres, perhaps due to some shared well-known risk factors with those affluent countries.
This study has the limitations inherent to all cross-sectional studies, the foremost being that causality cannot be inferred. This study uses parental reports instead of physician's reports; however, the questionnaire was validated for infants attending the ED with acute wheezing episodes and against the paediatric thoracic physician's examination.10 Recall bias is always an issue in transversal studies. In this study, however, parents were surveyed regarding several events in early childhood (12–15 months), in which recall would be easier than in late childhood.
Evidence suggests that parents and healthcare professionals differ in their perceptions of “wheezing”. Different meanings for “wheezing” are recognised in Portuguese language and may be influenced by education, respiratory history and regional terminology, but our questionnaire was also validated in Portuguese (Brazilian) and adapted to European Portuguese. In a Portuguese survey, only 69% participants identified “wheezing” as a sound located in the chest, in agreement with its epidemiological definition.15 It has been shown that these different concepts may be a source of bias in survey results, with a considerable impact on wheezing prevalence estimates.15 In that case it could be worse because of underestimation of true prevalence, which is why questionnaires on wheezing in infants or children should be validated against a gold standard (paediatric pulmonologist) as for EISL questionnaire.
The small population-based sample might not be representative of the region, but provides, for the first time, relevant local information such as the frequency of antibiotics prescriptions to infants with RW and the whole sample of infants at the community level. This is important because of the irrational overuse of antibiotics in infants with or without recurrent wheezing.2
To avoid any bias due to seasonal and annual variation we included infants born in all four seasons.
The present study shows that the prevalence of RW during the first year of life in Setúbal is high and progresses with considerable severity in terms of medications prescribed, associated visits to ED and hospital admissions for wheezing. These characteristics suggest that the current approach for the prevention, diagnosis and management of RW in infants needs to be improved, which may have an impact on decreasing frequency and severity of wheezing episodes.
Conflict of interestThe authors have no conflict of interest to declare.
We are grateful to the parents who participated with their infants in the present study and to the collaboration provided by the staff of the participating Primary Care Health centres.
EISL 1 Study Group: Manuel Baeza-Bacab, (Mérida, Mexico); Álvaro Madeiro Leite, Olívia Costa Bessa (Fortaleza, Brazil) Elaine Xavier Prestes (Belem, Brazil), Emanuel Sarinho, Décio Medeiros (Recife, Brazil); Paulo Camargos, María Jussara Fernández-Fontes, Wilson Rocha (Bello Horizonte, Brazil); Dirceu Solé, Caroline Della Bianca (São Paulo, Brazil); Nelson Rosario Herberto Chong (Curitiba, Brazil); Gilberto B. Fischer (Porto Alegre, Brazil); Eduardo Cepeda (Barranquilla, Colombia); Oscar Aldrey, Arnaldo Capriles (Caracas, Venezuela); Javier Mallol, Viviana Aguirre, Alejandro Gallardo (Santiago, Chile); Mario Calvo, (Valdivia, Chile); Luis García-Marcos, Antonela Martínez-Torres, Virginia Pérez-Fernández, (Murcia, Spain), Carlos González-Díaz, Andrés González Hermosa (Bilbao, Spain), Ángel López-Silvarrey Varela (La Coruña, Spain), María Morales Suárez-Varela (Valencia, Spain); Paul L.P. Brand, Chantal AN Visser (Zwolle, The Netherlands).
EISL 3 Study Group: Dirceu Solé, Carolina Aranda, and Caroline Della Bianca (São Paulo, Brazil); Nelson Rosario and Herberto Chong (Curitiba, Brazil); Eliana C. Toledo, Cibele Matsuura de Oliveira (São José do Rio Preto, Brazil); Líllian Sanchez-Lacerda Moraes, Olga Akiko Takano (Cuiabá, Brazil); Marilyn Urrutia-Pereira and Juan Carlos Ivancevich (Uruguaiana, Brazil); Patrícia Polles de Oliveira Jorge (São Carlos, Brazil); Jurg Niederbacher-Velásquez, Carlos A. Cuadros-Mendoza, Diana C. Archila-Santamaria, Leonela Ballesteros-Chaparro, and Juan M. Joya-Moreno (Bucaramanga, Colombia); Javier Mallol*, Viviana Aguirre (Santiago, Chile); Gabriela A. Szulman, Ilse Behrends, and Ángela Spagnuolo de Gentile (Buenos Aires, Argentina); Erika Arruda-Chaves, Silvia Cachay-Chávez, and Claudia Mory-Arciniega (Lima, Perú); Catalina Pinchak, Anabel Akiki, Silvia Brea, Maria Nelly Márquez, Isabel Moreira, Adriana Muiño, and Marilyn Valentin (Montevideo, Uruguay); and Luis-García Marcos, Virginia Pérez-Fernández, and Antonela Martínez-Torres (Murcia, Spain).
*General Coordinator.