The use of herbs in patients with allergic diseases is a special problem and still controversial. The objective of this questionnaire-based study was to determine the rate of herbal use in allergy clinic outpatients as well as to explore patient knowledge.
MethodsPatients with respiratory and/or skin disease, either atopic or non-atopic were assigned to a prospective questionnaire study conducted in allergy clinic outpatients.
ResultsThree hundred and ninety-five patients enrolled in the study. The mean age was 33.50±12.14 years. Participants generally had a high educational level (40.5% college and 39% university graduated). The rate of herbal use was 14.2%. All characteristics were similar within herbal user and non-user patients, except gender and age. The number of female patients who use herbal products was greater than for males (p=0.043). Herbal use was common in patients in their late thirties (p=0.024). Three main rationales for herbal use were revealed: (i) acting upon advice of someone (41.1%); (ii) the belief that “herbals are always more beneficial than chemicals” (37.5%); and (iii) the trust that “herbals are always safe” (21.4%). Most of the participants have “no idea” (41.5%) or are “not sure” (33.7%) about potential harmful effects of herbs to allergic people.
ConclusionPeople will continue to use herbals for one reason or another. Allergists and clinical immunologists need to become more knowledgeable about herbal therapies so that they can inform patients about either the benefits or possible harmful effects of herbs.
The use of herbs to treat illness has its roots in an ancient holistic healing tradition that originated in Asia more than 3,000 years ago.1 Nowadays, they are also widely used in many countries either to treat several illnesses or with the expectation of good health. As in other complementary medicines, herbal products should be used in accordance with the results of controlled studies.
“Herbal abuse” is a considerable issue, even in developed countries. Today, there are many commercial herbal preparations, which are reported as being used as a therapeutic agent for several disorders. Because herbs are widely accepted as safer than chemical drugs, uncontrolled uses of these “therapeutic” agents are increasing by the day.
The use of herbs in patients with allergic diseases is a special problem and still controversial. While some clinicians report significant improvements in allergic asthma and/or rhinitis, others draw attention to the potential hazards of herbals in atopic patients.2–4
The objective of this questionnaire-based study was to determine the rate of herbal use in allergy clinic outpatients. In addition, to determine the knowledge and preferences of patients about herbal products and the extent to which differences in social demographic and educational characteristics exist between herbal users and non-users.
Material and methodsThe study was conducted prospectively in Allergy Clinic of Gulhane Military Medical Academy Hospital in Ankara, Turkey. Study protocol has been reviewed and ethically approved by the local ethical committee of Gulhane Military Medical Academy and School of Medicine. Written informed consent was obtained from all patients.
Patients with respiratory and/or skin disease, either atopic or non-atopic were recruited. The participants were randomly selected on the principle of willingness. The questionnaire form was specifically designed for this study and included demographic data, current use and type of herbal remedies, reasons for choosing herbals, suppliers for herbals, clinical outcome and side effects and general knowledge of patients about herbal therapies. A total of 500 questionnaires were given out, 395 completed questionnaires were collected. The response rate was 79%.
Results were recorded and calculated by SPSS for Windows ver.15. The distribution analysis was performed by using chi-square test.
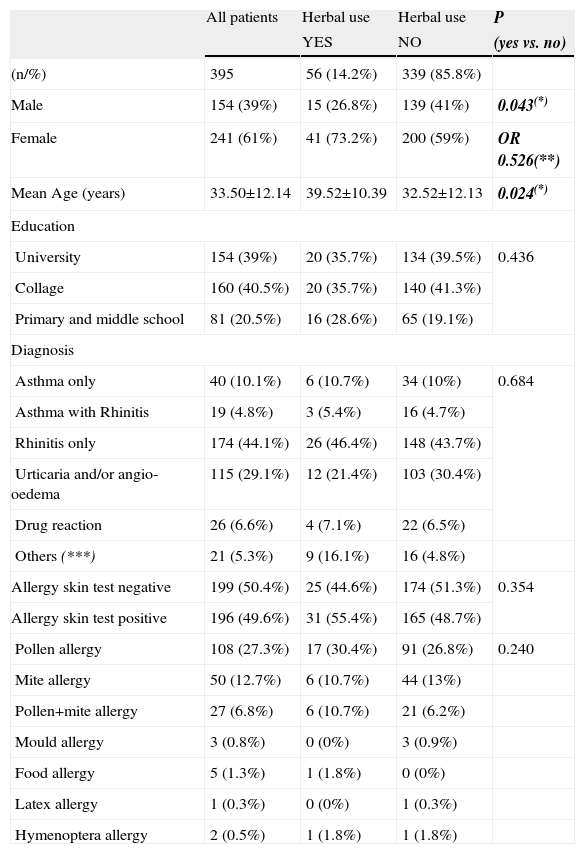
ResultsA total of 395 patients were enrolled in the study (154 males and 241 females). The mean age was 33.50±12.14 years (9 years to 80 years). Participants generally had a high educational level (40.5% college, and 39% university). The majority of hospital admissions were for respiratory and/or skin complaints (44.1% rhinitis only, 10.1% asthma only, 4.8% asthma with rhinitis and 29.1% urticaria and/or angio-oedema). About half of the patients (n=198, 50.1%) were allergic to at least one aeroallergen with a dominance of pollen allergy. Only 56 of 395 patients (14.2%) were using a herbal product (Table 1).
Characteristics and comparison of herbal user and non-user patients
| All patients | Herbal use | Herbal use | P | |
| YES | NO | (yes vs. no) | ||
| (n/%) | 395 | 56 (14.2%) | 339 (85.8%) | |
| Male | 154 (39%) | 15 (26.8%) | 139 (41%) | 0.043(*) |
| Female | 241 (61%) | 41 (73.2%) | 200 (59%) | OR 0.526(**) |
| Mean Age (years) | 33.50±12.14 | 39.52±10.39 | 32.52±12.13 | 0.024(*) |
| Education | ||||
| University | 154 (39%) | 20 (35.7%) | 134 (39.5%) | 0.436 |
| Collage | 160 (40.5%) | 20 (35.7%) | 140 (41.3%) | |
| Primary and middle school | 81 (20.5%) | 16 (28.6%) | 65 (19.1%) | |
| Diagnosis | ||||
| Asthma only | 40 (10.1%) | 6 (10.7%) | 34 (10%) | 0.684 |
| Asthma with Rhinitis | 19 (4.8%) | 3 (5.4%) | 16 (4.7%) | |
| Rhinitis only | 174 (44.1%) | 26 (46.4%) | 148 (43.7%) | |
| Urticaria and/or angio-oedema | 115 (29.1%) | 12 (21.4%) | 103 (30.4%) | |
| Drug reaction | 26 (6.6%) | 4 (7.1%) | 22 (6.5%) | |
| Others (***) | 21 (5.3%) | 9 (16.1%) | 16 (4.8%) | |
| Allergy skin test negative | 199 (50.4%) | 25 (44.6%) | 174 (51.3%) | 0.354 |
| Allergy skin test positive | 196 (49.6%) | 31 (55.4%) | 165 (48.7%) | |
| Pollen allergy | 108 (27.3%) | 17 (30.4%) | 91 (26.8%) | 0.240 |
| Mite allergy | 50 (12.7%) | 6 (10.7%) | 44 (13%) | |
| Pollen+mite allergy | 27 (6.8%) | 6 (10.7%) | 21 (6.2%) | |
| Mould allergy | 3 (0.8%) | 0 (0%) | 3 (0.9%) | |
| Food allergy | 5 (1.3%) | 1 (1.8%) | 0 (0%) | |
| Latex allergy | 1 (0.3%) | 0 (0%) | 1 (0.3%) | |
| Hymenoptera allergy | 2 (0.5%) | 1 (1.8%) | 1 (1.8%) | |
Mean±std.dev. (*)Chi-square test (**) Odds Ratio (95% Confidence Interval 0.280 to 0.988) (***) Others: Food allergy, atopic dermatitis, contact dermatitis, cold urticaria, chronic sinusitis, solar urticaria, hereditary angio-oedema.
Herbal “user” and “non-user” patients were compared with respect to:
- a)
Gender: The number of female patients who use herbal products was greater than for males. The difference was meaningful (p=0.043).
- b)
Mean age: Herbal use was common in patients in their late thirties (p=0.024).
- c)
Education: The level of education was similar in both herbal user and non-user patients.
- d)
Diagnosis: Distribution of the diagnoses was similar in all groups and not a distinguishing factor for herbal use.
- e)
Atopy: Skin test positivity to an aeroallergen was not different in herbal user and non-user patients. Similarly, the sort of positive allergens in atopic patients were also not different between the two groups.
Three main rationales for herbal use were exposed:
- (i)
Acting upon advice of someone (41.1%): Friends were common advisors (46.4%). The media (the Internet, newspapers and magazines) was second with a similar ratio to friends (41.1%). Only 12.5% of herbal users were using them by a physician's recommendation.
- (ii)
The belief that “herbals are always more benefit than chemicals” (37.5%).
- (iii)
The trust that “herbals are always safe” (21.4%).
Patients declared several “indications” for their herbal use (other than allergic diseases) (e.g. constipation, haemorrhoids, peptic ulcer, hyperlipidaemia, anti-anxiety, sleep-induce, chronic fatigue, to lose weight, and mostly to maintain good health).
All participants were questioned about potential harmful effects of herbs on allergic people. Answers were similar in both allergic and non-allergic patients:
- •
“No idea” (41.5%)
- •
“Not sure, maybe” (33.7%)
- •
“Herbs have not harmful effects for allergic people” (8.9%)
- •
“Herbs are definitely injurious for people with allergic diseases” (15.9%)
Sources of herbals were also asked. There were two main suppliers, “Aktar” shops (*); and pharmacies, in 58.9% and 33.9% of patients, respectively. In addition, a small number of patients (7.2%) pick the herbs themselves directly from nature. ((*) Aktar means seller of herbs, spices and folk remedies in the Turkish language. They do not have a school-based education on herbs, but have considerable knowledge about plants and herbal remedies, which are mostly data inherited from father to son, in other words it is a traditional occupation).
The final question was “Did you benefit from the herb?” Not surprisingly, numerous herbal users (64.3%) answered affirmatively. Twelve per cent of users were not benefitted. The remaining (23.2%) declined to answer this question.
DiscussionThe use of herbs to enhance health status as well as to treat medical symptoms is becoming increasingly popular. Studies show that about one-half of the general population and one-third of allergic patients use unconventional remedies, including herbal products.5,6 “Herbal remedies” must be distinguished from medicinal plants and botanicals or botanical preparations intended for use as ingredients. The terms of “herbal” or “herbs” used in this paper, mainly imply the whole, fragmented or cut plants, unprocessed plant parts or herbal preparations marketed as “complementary” products.
The rate of herbal use in our study was 14.2%. Except for gender and age, all characteristics were similar within herbal user and non-user allergy clinic out-patients (Table 1). The user percentage was significantly lower than a previously published Turkish study, which was conducted in the same city and in patients with a similar number and characteristics.7
Self-medication is a crucial problem about herbal remedies. Administration of herbals without physician communication may cause not only side-effects but also a delay in the beginning of the proper treatment or an alteration of the treatment that the patient is following. Another important issue that must be considered in self-medication is the risk of possible adverse interactions between prescription medicines and herbs.8 In our study only 12.5% of herbal users were using them following medical advice. On the other hand, many physicians who recommend herbal products are not trained for herbal therapy. Because of the undesired effects mentioned above, herbal remedies must be a regular part of the health care systems, as in the European Union.9
In fact, a herb can show some clinical benefits. However, it also involves a considerable risk of adverse effects ranging from a negligible inconvenience to a severe and life-threatening event. While these effects can be predicted for conventional medicines, little is known about adverse reactions of unconventional methods. Patients are generally aware of herbal related adverse effects, as our patients are. Approximately three quarters of the study participants had “no idea” and “not sure” about possible harmful effects of herbs. This may be due to a misconception that herbal agents come from natural plants and are therefore naturally safe. Although there are several published reports about herbal therapies in allergic diseases, results lack consistency and are without high-quality scientific data. It means we still have no appropriate guidelines for their use in patients with allergic disorders. Efficacy and safety of herbal therapies need to be established with randomised, double-blind, placebo-controlled trials before integrating these “traditional” methods into “conventional” treatments.4,10,11
Various problems including substitution, misidentification/misbranding, contamination, adulteration and toxicity had been attributed to herbal preparations. However, exacerbation of allergies and asthma, and anaphylactic reactions are usually omitted. We think that using a herbal product for any reason in patients with atopy and allergy needs a special concern. Herbals seem to be more prone to cause unwanted effects in these groups of patients. “Allergic” reactions to herbals are reported several times. However, most reports are anecdotal. There is a lack of surveys that could provide estimates of the incidence of allergic side-effects to herbal preparations.4,12
The spectrum of herbal allergies is very wide, ranging from cutaneous lesions to life-threatening events. Both type 4 (delayed) and type 1 (immediate) hypersensitivity reactions can be seen. Type 4 reactions seem to be more frequent. There are many reported cases including, recurrent facial dermatitis from chamomile tea,13 phototoxic reaction on neck and extremities after taking a dietary supplement containing ginseng and goldenseal,14 allergic contact dermatitis from chamomile used in phytotherapy,15 allergic and systemic contact dermatitis from Matricaria chamomilla tea,16 vulval allergic contact dermatitis due to peppermint oil in herbal tea17 and erythema multiforme-like generalised allergic contact dermatitis caused by Alpinia galangal.18
Type 1 hypersensitivity reactions to herbals may happen due to new sensitisation to herbals used, or in consequence of cross-reaction due to existing pollen allergy. Almost all clinical presentation of immediate reactions such as urticaria,19 conjunctivitis;20 asthma exacerbation;21 and anaphylaxis,22–26 and 27 have been reported with herbals. These reactions are more likely in patients already sensitised with pollens. This is because most herbals are naturally contaminated with pollens. Another cause is cross-reactivity, which means a pollen specific IgE in host can react with a herbal allergen which contains similar allergenic epitopes. This similarity may lead to allergic reactions from oral allergy syndrome to systemic anaphylaxis. Allergy due to cross-reactivity is best described in Echinacea and Chamomilla, which are highly cross-reactive with several pollen allergens.24,26,28,29,30
Anaphylactic reactions to herbals need a special concern. Anaphylaxis is the most severe form of Type 1 hypersensitivity reaction, which sometimes can be fatal. Aetiological diagnosis is of great consideration to prevent further anaphylactic episodes. However, the cause of anaphylaxis can be elucidated in less than half of the cases.31 Herbals should always be considered and asked about in cases with anaphylaxis with unknown aetiology. Since herbals are not usually perceived as medicine by the patients, these are only declared when the physician expressly asks. In fact, we have had an experience of this kind of case: a 42-year-old female patient, who experienced a near-fatal anaphylactic reaction, referred to our allergy clinic. Her medical history was not indicative for any possible cause of anaphylaxis. After we showed a strong positivity to parsley on epidermal allergy test, she declared a regular consumption of parsley for several years to maintain good health. Furthermore, she described an itching sensation in her whole body during every previous intake of parsley. She was also allergic to several weed pollens which are strongly cross-reactive to parsley (unpublished clinical case).
In conclusion, the reality is that people will continue to use herbals for one reason or another. As confirmed again by our results, herbal usage is not related with education or social statue. Allergists and clinical immunologists need to become more knowledgeable about herbal therapies so that they can inform patients about either the benefits or possible harmful effects of herbs.
Conflict of interestThe authors have no conflict of interest to declare.