In previous studies, anti-inflammatory, anti-apoptotic and immunomodulatory effects of ursodeoxycholic acid (UDCA) on liver diseases have been shown. In this study, we aimed to investigate the effects of UDCA on airway remodelling, epithelial apoptosis, and T Helper (Th)-2 derived cytokine levels in a murine model of chronic asthma.
MethodsTwenty-seven BALB/c mice were divided into five groups; PBS-Control, OVA-Placebo, OVA-50mg/kg UDCA, OVA-150mg/kg UDCA, OVA-Dexamethasone. Mice in groups OVA-50mg/kg UDCA, OVA-150mg/kg UDCA, OVA-Dexamethasone received the UDCA (50mg/kg), UDCA (150mg/kg), and dexamethasone, respectively. Epithelium thickness, sub-epithelial smooth muscle thickness, number of mast and goblet cells of samples isolated from the lung were measured. Immunohistochemical scorings of the lung tissue for matrix metalloproteinase-9 (MMP-9), vascular endothelial growth factor (VEG-F), transforming growth factor-beta (TGF-β), terminal deoxynucleotidyl transferase-mediated dUTP nick endlabeling (TUNEL) and cysteine-dependent aspartate-specific proteases (caspase)-3 were determined. IL-4, IL-5, IL-13, Nitric oxide, ovalbumin-specific immunoglobulin (Ig) E levels were quantified.
ResultsThe dose of 150mg/kg UDCA treatment led to lower epithelial thickness, sub-epithelial smooth muscle thickness, goblet and mast cell numbers compared to placebo. Except for MMP-9 and TUNEL all immunohistochemical scores were similar in both UDCA treated groups and the placebo. All cytokine levels were significantly lower in group IV compared to the placebo.
ConclusionsThese findings suggested that the dose of 150mg/kg UDCA improved all histopathological changes of airway remodelling and its beneficial effects might be related to modulating Th-2 derived cytokines and the inhibition of apoptosis of airway epithelial cells.
Asthma is a common chronic disorder of the airway that is characterised with the complex interaction of airway inflammation, airway remodelling, and bronchial hyperresponsiveness which lead to recurrent episodes of breathlessness, wheezing, chest tightness, and coughing.1 The airway inflammation is typically eosinophilic and it is accompanied by the elevation of Th-2 cytokines such as IL-4, IL-5, IL-13. Airway remodelling consists of epithelial injury, goblet cell hyperplasia, airway smooth muscle hyperplasia, sub-epithelial layer thickening from increased deposition of extra cellular matrix proteins, and angiogenesis.2 Extensive studies on airway remodelling in asthma focused on the determination of the implicated cytokines, growth factors, and chemokines. Several mediators of remodelling were identified, including IL-4, IL-9, IL-13, IL-17, VEGF, MMP-9 and TGF-β.3,4
Apoptosis has important and beneficial regulatory roles in the normal airway epithelium. However, airways of asthmatics exhibit an elevated rate of epithelial apoptosis and this is related with increased disease severity.5 Apoptotic process includes the cleavage of a number of proteins, which can be observed by cysteine-dependent aspartate-specific proteases (caspase)-3 staining and DNA fragmentation that can be detected by terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling (TUNEL) staining.5
The presence of advanced airway remodelling is associated with a poorer clinical prognosis and is therefore considered as an important therapeutic target.6 Unfortunately, current anti-inflammatory therapeutic strategies including inhaled corticosteroids are less successful in treating structural alterations in airway remodelling even though they are effective in reducing the inflammation.7 Thus, novel therapeutic strategies which have a potent effect on the airway remodelling should be developed.
Ursodeoxycholic acid (UDCA) is a tertiary bile acid that has been used for centuries in the clinical treatment of gallstones, primary biliary cirrhosis, and primary sclerosing cholangitis.8 Immunomodulatory properties of UDCA in liver diseases have been shown in previous studies.9–12 UDCA also has immunomodulatory effects except in the gastrointestinal tract.13 However, according to our knowledge, the effects of UDCA on airway remodelling, epithelial apoptosis, and TH2 immune response have been firstly investigated in the murine model of chronic asthma in our study in comparison with the conventional dexamethasone treatment.
Materials and methodsAnimals, experimental protocol and study drugsA total of twenty-seven, conventionally raised, 6–8-week-old male BALB/c mice weighing 18–20g were used in the study. The animals were kept in hygienic macrolane cages in air-conditioned rooms on a 12-hour light/dark cycle. Mice were fed with commercial diet ad libitum for the experiment. All experimental procedures complied with the requirements of the Animal Care and Ethics Committee of the Dokuz Eylul University.
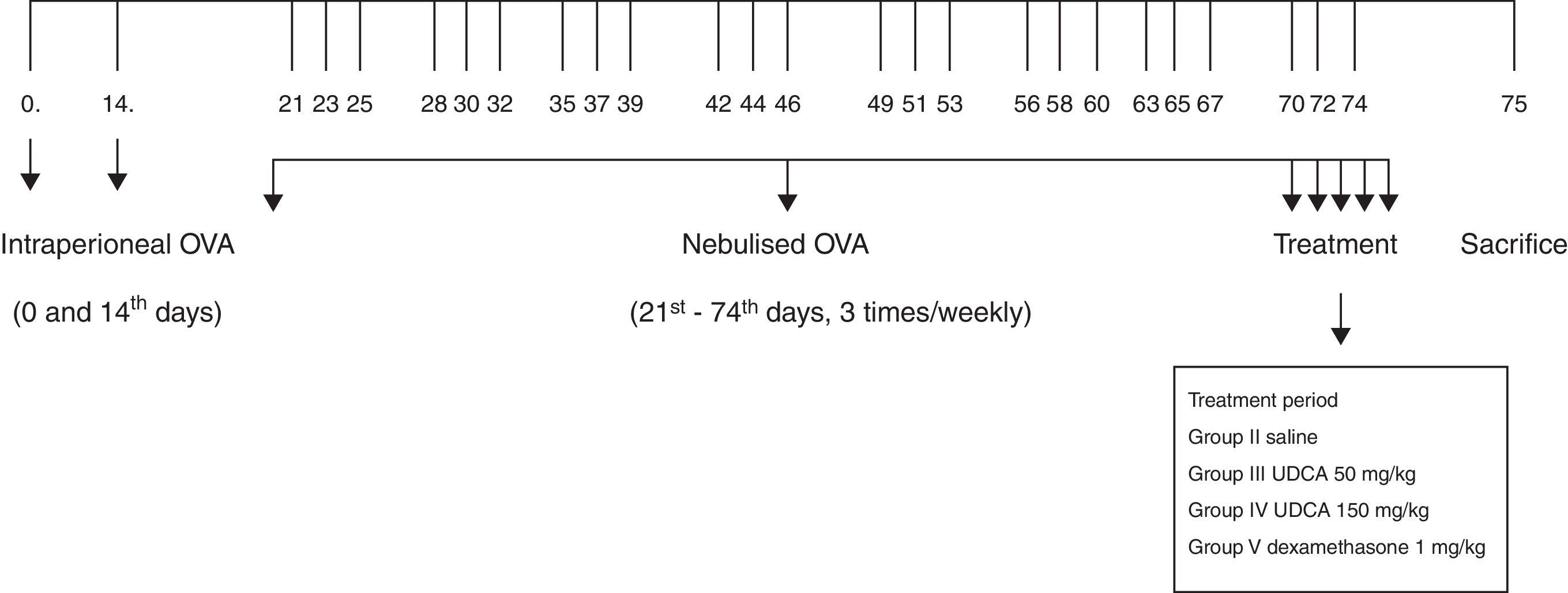
Mice were divided into five groups: PBS-Control; OVA-Placebo; OVA-50mg/kg UDCA; OVA-150mg/kg UDCA; and OVA-Dexamethasone. The PBS-Control group was exposed to saline only. Mice in the groups OVA-Placebo, OVA-50mg/kg UDCA, OVA-150mg/kg UDCA, OVA-Dexamethasone were sensitised by an intraperitoneal (IP) injection of ovalbumin (10μg/0.1ml, 2 weeks apart, i.e. Days 0 and 14) consisting of chicken egg albumin (ovalbumin, grade V, ≥98% pure, Sigma, St. Louis, MO, USA) with alum adjuvant as described by Temelkovski et al.14 The mice in study OVA-Placebo, OVA-50mg/kg UDCA, OVA-150mg/kg UDCA, OVA-Dexamethasone were then exposed to aerosolised ovalbumin (5ml, 2.5%) for 30min per day (three days per week) for eight weeks, beginning from the 21st day of the study (Fig. 1). The mice in PBS-Control group were intraperitoneally administered with normal saline with alum on Days 0 and 14 of the experiment and exposed to aerosolised saline without alum for 30min per day (three days per week) for eight weeks, beginning from the 21st day of the study. Exposures were carried out in a whole-body inhalation exposure system in a Plexiglas chamber measuring 40×60×120 designed for the placement of cages, in all groups. Temperature and relative humidity were maintained between 20–25°C and 40–60%, respectively. A solution of 2.5% ovalbumin in normal saline was aerosolised by the delivery of compressed air to a sidestream jet nebuliser injected into a chamber with a flow rate of 6L/min (Medicair, UK). The aerosol generated by this nebuliser comprised >80% particles with a diameter of <4μm. Particle concentration was maintained in the range of 10–20mg/mm3 in the chamber. Thus, it was predicted that more than 90% of the particles would remain in the mouse airways, which would be enough for the development of the asthma model.15 During the last five days of the challenge period, mice in group OVA-Placebo received saline, mice in group OVA-50mg/kg UDCA received UDCA (Sigma Aldrich, St. Louis, MO, USA) at dose of 50mg/kg, mice in group OVA-150mg/kg UDCA received UDCA at dose of 150mg/kg, mice in group OVA-Dexamethasone received dexamethasone (Dekort; Deva Holding AS, Istanbul, Turkey) at dose of 1mg/kg by orogastric tube, once a day.15,16 Animals were sacrificed by an intraperitoneal injection of ketamine hydrochloride (200mg/kg) 24h after the last drug administration.
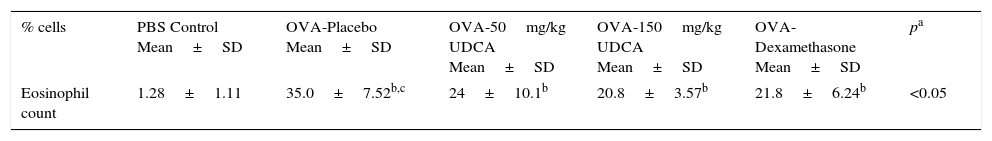
Histopathological analysisFor the histological study, mid-zone lung tissues were obtained and fixed in buffered 10% formalin and embedded in paraffin wax. Five-micron-thick serial sections were obtained and the first 10 sample stained with haematoxylin and eosin (H&E). General tissue features of these samples were examined and the thicknesses of epithelium and sub-epithelial smooth muscle layers of the medium and small airways were measured. In order to evaluate the thicknesses of epithelium and sub-epithelial smooth muscle layers, measurements were performed from four points of each airway. Considering that each section contained approximately two to three airways, around 20 or more airways were evaluated for each mouse. Photomicrographs were taken by Olympus DP71 camera (Japan), which adapted on Olympus DP70 model microscope (Olympus Optical, Tokyo, Japan). Measurements were carried out with UTHSCSA Image Tool for Windows Version 3.00 software.
The consecutive 10 sections were stained with toluidine blue and the other 10 sections were stained with periodic acid-Schiff (PAS). Photomicrographs were randomly taken from five fields of each section which were stained with toluidine blue. For mast cell enumeration, a standard transparent counting frame representing an area of 16,400μm2 was manually used and eight fields in each photograph were examined for each mouse. Goblet cells stained with PAS were enumerated in 10 sections of each mouse. In each section, three to five randomly selected airways were photographed. Circumferences of all airways were measured and goblet cell numbers in these areas were recorded. For standardisation, goblet cell numbers in 100μm were analysed by dividing the total goblet cell number to the total length of airway circumferences and multiplying the result by one hundred.
Measurement of cytokines in lung homogenatesLungs were removed and washed with cold PBS three times in order to remove the blood. Lung tissues were taken into 2ml microcentrifuge tubes and stored at −80°C until analysis. On the study day, frozen lung tissues were thawed, weighed (60–80mg), transferred into different tubes on ice containing 5ml of stainless beads, 0.1% SDS protease inhibitor cocktail (Sigma–Aldrich, St. Louis, MO, USA) and 0.1mg/ml phenylmethanesulfonyl fluoride (PMSF) in PBS. Microcentrifuge tubes were transferred to pre-cooled Tissuelyser LT racks and placed into Tissuelyser (Qiagen, Germany) homogenisator. Time and frequency were set to 5 and 50min, respectively. The homogenates were then centrifuged at 15,000×g for 1h at 4°C and supernatants were obtained. Levels of IL-4, IL-5, IL-13 cytokines were quantified in the supernatants of the lung tissue by standard ELISA protocols by using commercial Mouse IL-4, IL-5, IL-13 (eBioscience Mouse ELISA kit, USA). Detection levels were 4pg/ml for IL-4 and IL-5, 2.8pg/ml for IL-13.
Measurement of NO in lung homogenatesNitric oxide levels were measured by ELISA in accordance with the manufacturer's recommendations in supernatants obtained from the lung tissue homogenates (Invitrogen Grıess Reagent). Griess Reagent (A: 1-naphthyethylene-diamine dihydrochloride, 0.1%; B: sulfanilic acid 1%) and samples were mixed with an equal volume in microtiter plates (Greiner) and they were stored at room temperature for 30min. Results were determined at 548nm (BioTek Synergy HT, USA) by using spectrophotometric methods.17
Measurement of serum OVA specific IgE in serumSerum levels of OVA specific IgE were measured by using the ELISA commercial kit (Sun Red Biological Technology, Shanghai, China).
Immunohistochemical detectionsCaspase-3 (AB3623, Millipore, Temecula, CA, USA, Polyclonal antibody), TUNEL (DeadEnd Colorimetric TUNEL system kit, Roche, Germany), MMP9 (anti-MMP-9 mouse monoclonal antibody, Santa Cruz Biotech, Inc., Germany), VEGF (anti-VEGF mouse monoclonal antibody, Santa Cruz Biotech, Inc., Germany), TGF-β (anti-TGF-β mouse monoclonal antibody, Santa Cruz Biotech, Inc., Germany) antibodies were used in immunohistochemistry experiments. After deparaffinisation and rehydration, sections were treated with trypsin (Cat No: 00-3008 Digest All 2A, Zymed, San Francisco, CA, USA) at 37°C for 15min (for TUNEL, MMP9, VEGF, TGF-β antibodies). For caspase-3, samples were treated with 10mM citrate buffer (Cat No. AP-9003-125 Labvision) for 5min to unmask antigens by using the heat treatment. Slides cooled in buffer for 20min. For all sections, sections were incubated in a solution of 3% H2O2 for 15min and then with normal serum blocking solution to inhibit endogenous peroxidase activity. Sections were again incubated in a humid chamber for 18h at +4°C with primer antibodies, thereafter with biotinylated IgG, and then with streptavidin conjugated to horseradish peroxidase for 15min as per kit instructions (85-9043, Invitrogen Corporation, Camarillo, UK). Sections were finally stained with DAB (diaminobenzidine) (1718096, Roche, Mannheim, Germany) and counter-stained with Mayer's haematoxylin. Samples were analysed using a light microscope.18
Semi-quantification of immunostaining dataSemi-quantitative grading system was used to score the quantity of primer antibody positive staining in the sections.19 The score was defined as follows: 0: no immunoreactivity; 1: remarkably little positive staining; 2: moderate positive staining; 3: strong positive staining evenly distributed across the whole image. Each section was graded by two individuals blind to the treatments, and the average score was taken.
Statistical analysisAll values were expressed as the mean±standard deviation (SD). The Kruskal–Wallis (between all groups) and Mann–Whitney U-test (for two groups) was used to compare staining intensity values between groups. All statistical analyses were performed using the SPSS software for Windows, Version 15.0 (SPSS, Chicago, IL, USA). The significance was accepted when the p value was lower than 0.05 (p<0.05).
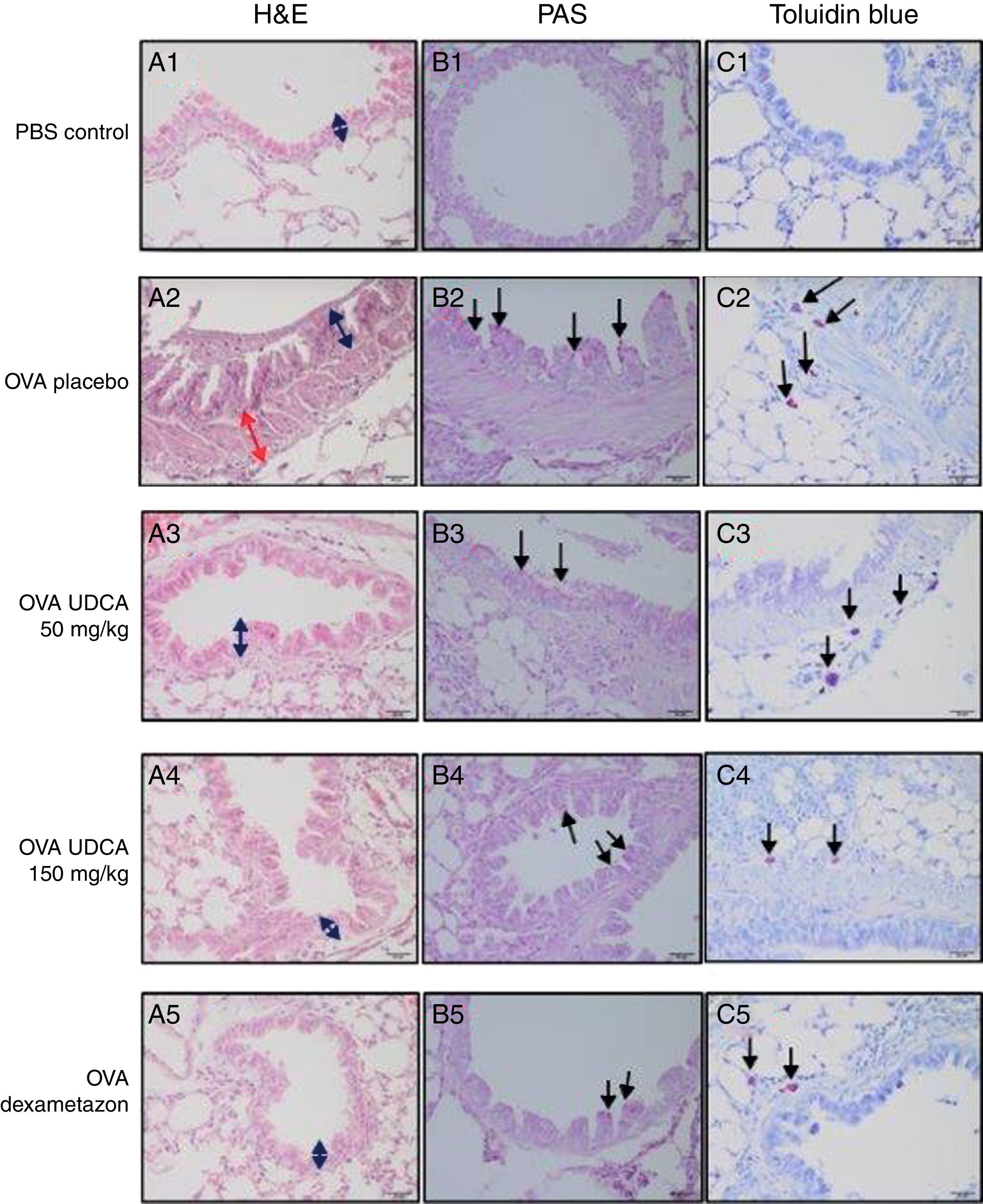
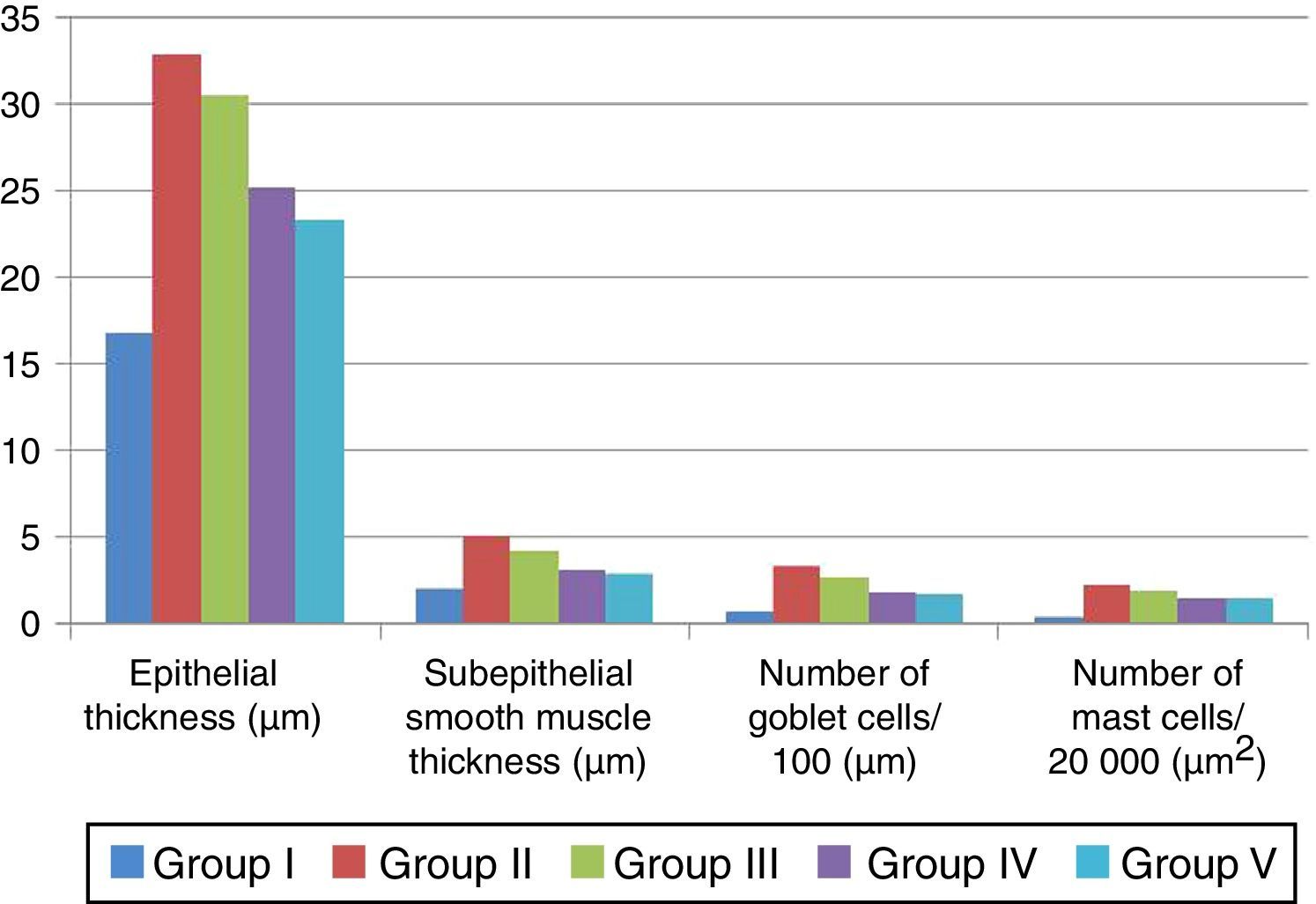
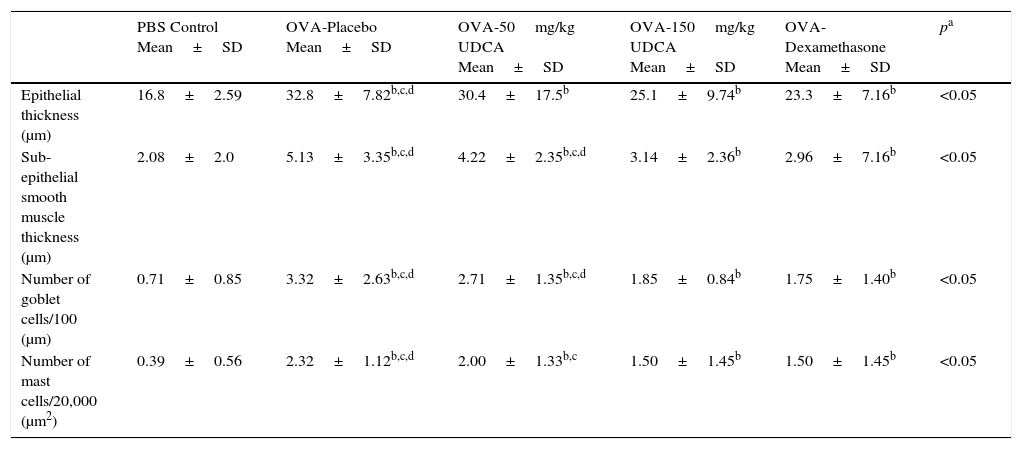
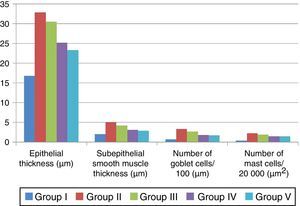
ResultsComparison of the histopathological findings of the study groupsThe light microscopic examinations revealed normal findings in the PBS-Control group (Table 1). We compared the histopathological features of the control group with the placebo group in order to show that the asthma model was successfully established. In the placebo group, thicknesses of epithelium and smooth muscle layers as well as numbers of mast cells and goblet cells were significantly higher compared to the control group. According to these findings, the chronic asthma model was successfully established. Sub-epithelial smooth muscle and epithelial thicknesses, mast cell and goblet cell numbers were significantly lower in the OVA-150mg/kg UDCA treated group compared to the OVA-placebo group. There was no difference between the OVA-150mg/kg UDCA treated and OVA-Dexamethasone treated groups in terms of epithelial thickness, sub-epithelial smooth muscle, mast and goblet cell numbers. In the OVA-50mg/kg UDCA treated group, all histopathological findings except for numbers of mast cells were similar to the OVA-placebo group. All histological parameters were significantly lower in the OVA-Dexamethasone treated group compared to the OVA-placebo group (Table 1, Figs. 2 and 3).
Comparison of the histopathological findings of study groups (mean±SD).
| PBS Control Mean±SD | OVA-Placebo Mean±SD | OVA-50mg/kg UDCA Mean±SD | OVA-150mg/kg UDCA Mean±SD | OVA-Dexamethasone Mean±SD | pa | |
|---|---|---|---|---|---|---|
| Epithelial thickness (μm) | 16.8±2.59 | 32.8±7.82b,c,d | 30.4±17.5b | 25.1±9.74b | 23.3±7.16b | <0.05 |
| Sub-epithelial smooth muscle thickness (μm) | 2.08±2.0 | 5.13±3.35b,c,d | 4.22±2.35b,c,d | 3.14±2.36b | 2.96±7.16b | <0.05 |
| Number of goblet cells/100 (μm) | 0.71±0.85 | 3.32±2.63b,c,d | 2.71±1.35b,c,d | 1.85±0.84b | 1.75±1.40b | <0.05 |
| Number of mast cells/20,000 (μm2) | 0.39±0.56 | 2.32±1.12b,c,d | 2.00±1.33b,c | 1.50±1.45b | 1.50±1.45b | <0.05 |
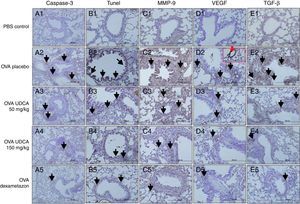
Histopathological findings of study groups. PBS Control (n:5), OVA-placebo (n:5), OVA-50mg/kg UDCA (n:6), OVA-150mg/kg UDCA (n:6), OVA-dexamethasone (n:5) A: H&E, B: PAS, C: toluidine blue staining. (A) Arrow with two heads; epithelial thickness (black arrow), sub-epithelial smooth muscle thickening (red arrow), (B) arrows; goblet cells, (C) arrows; mast cells.
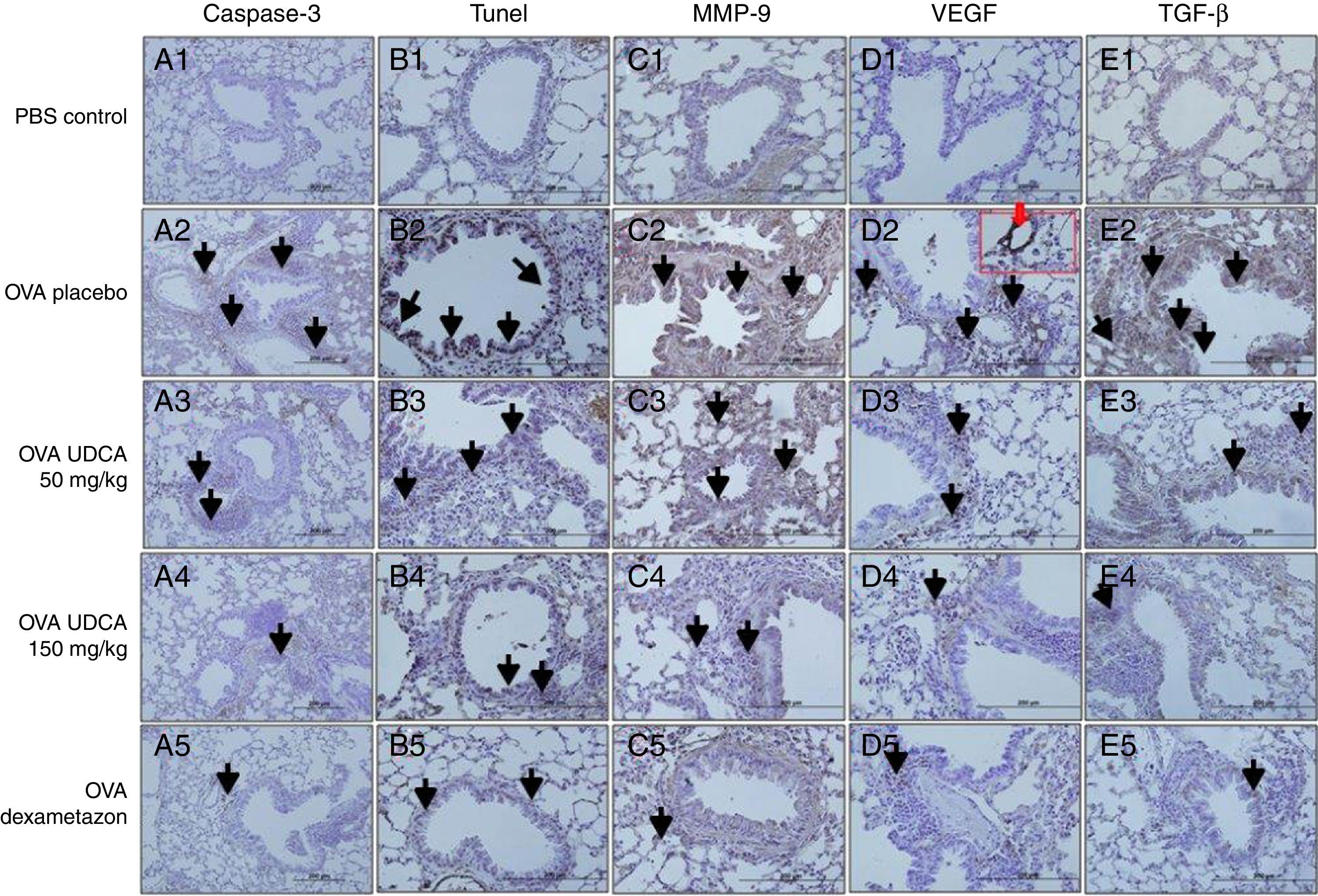
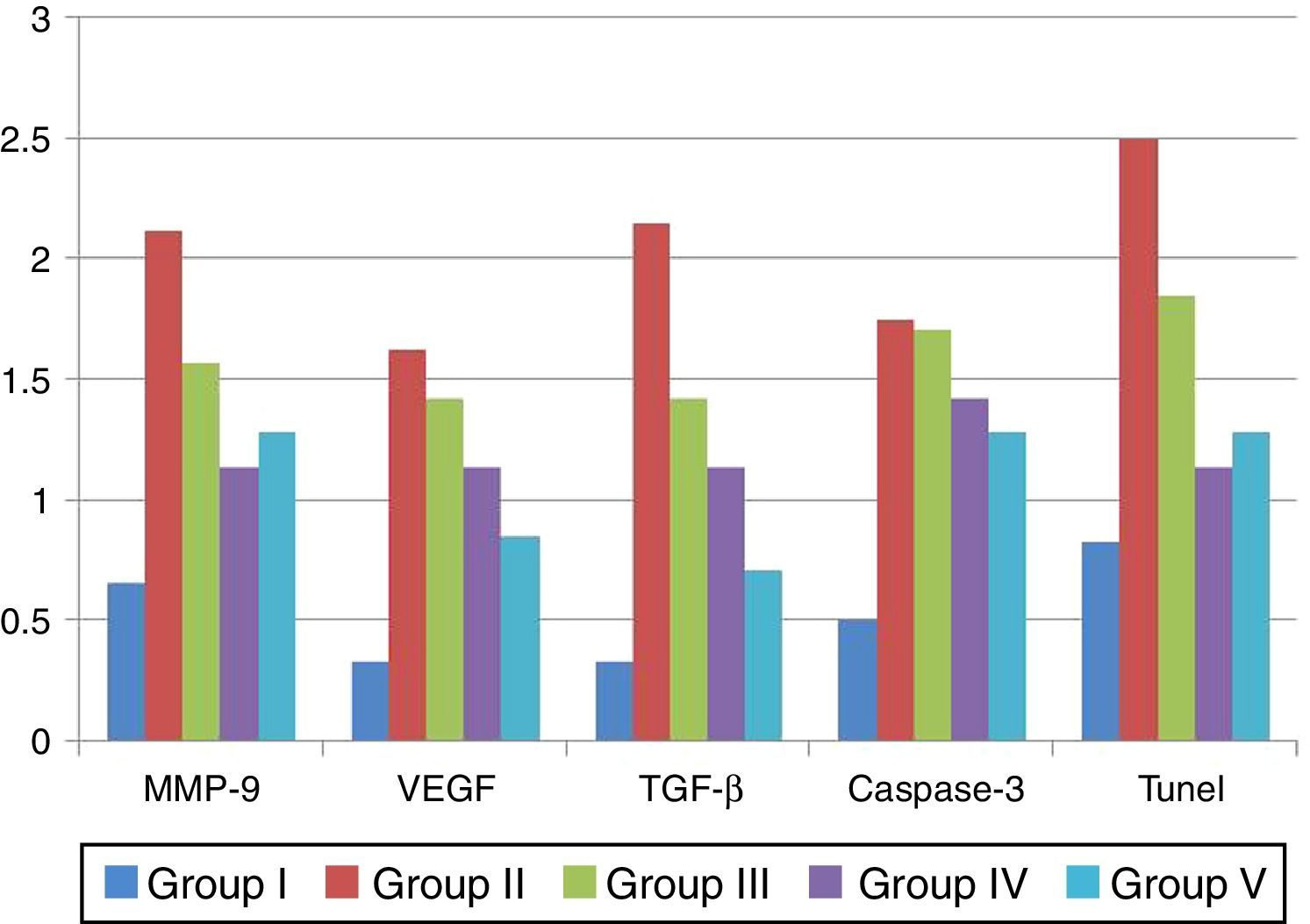
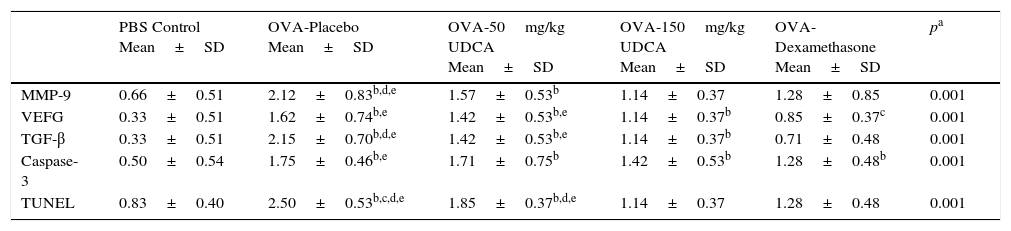
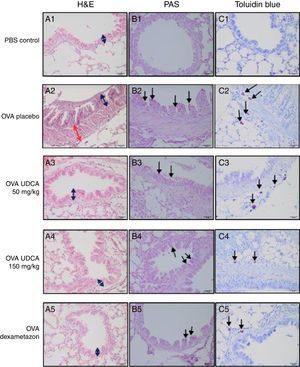
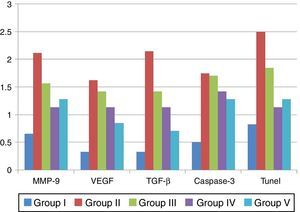
Immunohistochemical scoring of MMP-9, VEGF, TGF-β, TUNEL and caspase-3 were found lower in the PBS-Control group compared to the OVA-placebo group. In OVA-150mg/kg UDCA treatment group, only immunohistochemical scoring of TGF-β, MMP-9 and TUNEL were lower than the OVA-placebo group. Dexamethasone treatment led to lower immunohistochemical scoring of MMP-9, VEGF, TGF-β, TUNEL and caspase-3 compared to the OVA-placebo group. We also observed that immunohistochemical scoring of the both OVA-150mg/kg UDCA treatment and OVA-Dexamethasone groups were similar. In the OVA-50mg/kg UDCA treatment group, only immunohistochemical scoring of TUNEL was lower than in the OVA-placebo group. When both OVA-UDCA treatment groups were compared to each other, only immunoscoring of TUNEL was significantly lower in OVA-150mg/kg UDCA treatment group compared to the OVA-50mg/kg UDCA treatment group (Table 2, Figs. 4 and 5).
Comparison of the immunohistochemical scorings of study groups (mean±SD).
| PBS Control Mean±SD | OVA-Placebo Mean±SD | OVA-50mg/kg UDCA Mean±SD | OVA-150mg/kg UDCA Mean±SD | OVA-Dexamethasone Mean±SD | pa | |
|---|---|---|---|---|---|---|
| MMP-9 | 0.66±0.51 | 2.12±0.83b,d,e | 1.57±0.53b | 1.14±0.37 | 1.28±0.85 | 0.001 |
| VEFG | 0.33±0.51 | 1.62±0.74b,e | 1.42±0.53b,e | 1.14±0.37b | 0.85±0.37c | 0.001 |
| TGF-β | 0.33±0.51 | 2.15±0.70b,d,e | 1.42±0.53b,e | 1.14±0.37b | 0.71±0.48 | 0.001 |
| Caspase-3 | 0.50±0.54 | 1.75±0.46b,e | 1.71±0.75b | 1.42±0.53b | 1.28±0.48b | 0.001 |
| TUNEL | 0.83±0.40 | 2.50±0.53b,c,d,e | 1.85±0.37b,d,e | 1.14±0.37 | 1.28±0.48 | 0.001 |
MMP-9, matrix metallo proteinase-9; VEGF, vascular endothelial growth factor; TGB β, transforming growth factor-β; TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP nick endlabeling and caspase-3, cysteine-dependent aspartate-specific proteases.
Immunohistochemical staining results of study groups. PBS Control (n:5), OVA-placebo (n:5), OVA-50mg/kg UDCA (n:6), OVA-150mg/kg UDCA (n:6), OVA-dexamethasone (n:5). (A) Caspase-3, (B) TUNEL, (C) MMP-9, (D) VEGF, (E) TGF-β. Black arrows show positive staining with caspase 3, TUNEL, MMP-9, VEGF and TGF-β, respectively. Red arrow shows positive staining with VEGF more detailed. VEGF, vascular endothelial growth factor; MMP-9, matrix metallo proteinase-9, TGB-β, transforming growth factor-β, TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP nick endlabeling and caspase-3, cysteine-dependent aspartate-specific proteases.
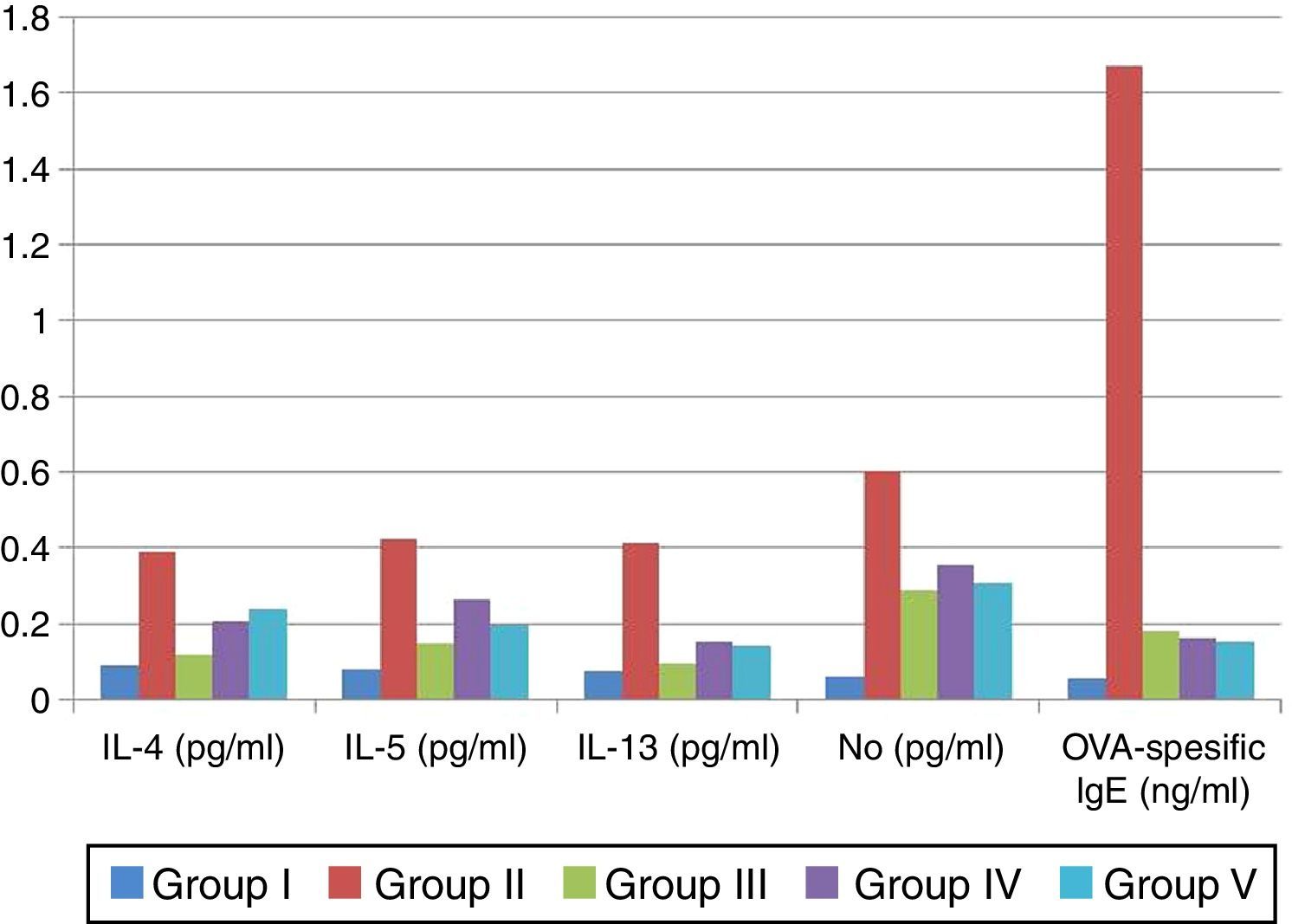
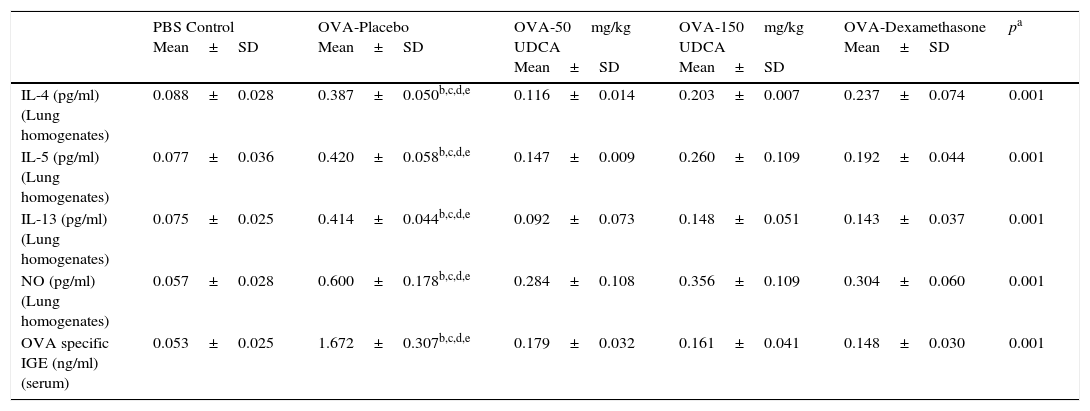
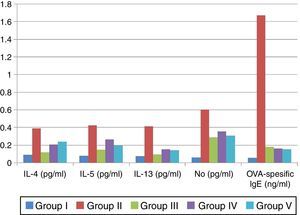
IL-4, IL-5, IL-13, NO levels in lung homogenates and OVA specific IgE levels in serum samples were significantly lower in PBS-Control group compared to the OVA-placebo group.
All cytokine levels (IL-4, IL-5, IL-13, NO) in lung homogenates and OVA-specific IgE level in serum samples were significantly lower in both OVA-UDCA treated groups and the OVA-Dexamethasone treated group compared to the OVA-placebo group (p<0.05) (Table 3, Fig. 6).
Comparison of the cytokine levels in lung homogenates and OVA-specific IgE in serum samples (mean±SD).
| PBS Control Mean±SD | OVA-Placebo Mean±SD | OVA-50mg/kg UDCA Mean±SD | OVA-150mg/kg UDCA Mean±SD | OVA-Dexamethasone Mean±SD | pa | |
|---|---|---|---|---|---|---|
| IL-4 (pg/ml) (Lung homogenates) | 0.088±0.028 | 0.387±0.050b,c,d,e | 0.116±0.014 | 0.203±0.007 | 0.237±0.074 | 0.001 |
| IL-5 (pg/ml) (Lung homogenates) | 0.077±0.036 | 0.420±0.058b,c,d,e | 0.147±0.009 | 0.260±0.109 | 0.192±0.044 | 0.001 |
| IL-13 (pg/ml) (Lung homogenates) | 0.075±0.025 | 0.414±0.044b,c,d,e | 0.092±0.073 | 0.148±0.051 | 0.143±0.037 | 0.001 |
| NO (pg/ml) (Lung homogenates) | 0.057±0.028 | 0.600±0.178b,c,d,e | 0.284±0.108 | 0.356±0.109 | 0.304±0.060 | 0.001 |
| OVA specific IGE (ng/ml) (serum) | 0.053±0.025 | 1.672±0.307b,c,d,e | 0.179±0.032 | 0.161±0.041 | 0.148±0.030 | 0.001 |
OVA, ovalbumin; IL, interleukin; NO, nitric oxide; UDCA, ursodeoxycholic acid.
The number of eosinophils in BAL fluid was significantly reduced in the OVA-50mg/kg UDCA and OVA-150mg/kg UDCA groups when compared to the OVA-Placebo group (Table 4).
DiscussionBronchial asthma is a chronic inflammatory disease of the airways that is characterised by chronic airway inflammation, airway hyperresponsiveness, and airway remodelling.20,21 Hallmarks of the structural changes in the airways include goblet cell hyperplasia, sub-epithelial fibrosis, increased smooth muscle mass, and angiogenesis.22 Current anti-inflammatory treatment of asthma is predominately based on the use of inhaled corticosteroids. Even though these drugs are highly effective in preventing life threatening consequences of asthma,23 their effect is limited in modulating the airway remodelling.24 Novel therapeutic strategies which do not have side effects and which can suppress the airway inflammation and remodelling are still needed.
Asthma model which mimics the remodelling process in humans are successfully well established in animal studies. The asthma model used in our study is a widely-used model.14 In our study, principal features of remodelling including sub-epithelial smooth muscle thickness, epithelial thickness, the number of mast and goblet cells were found significantly higher in the placebo group compared to the control group. These findings indicate that chronic changes associated with the features of remodelling have been generated successfully in an animal asthma model.
UDCA (ursodeoxycholic acid) is currently the most widely used therapeutic agent for the treatment of hepatopathies of a cholestatic nature, such as PBC (primary biliary cirrhosis).25 In previous studies, immunomodulatory effect of UDCA via suppression of eosinophil activation and degranulation,12 inhibition of mast cell activation,13 inhibition of the IgG, IgA, IgM, and cytokine production by mononuclear cell,13 reduction of the aberrant expression of class 1 human leukocyte antigens (HLA 1) on hepatocytes,26 has been shown in hepatic diseases. Willart et al. conducted a study on immunomodulatory effects of UDCA outside the gastrointestinal tract, such as eosinophilic airway inflammation seen in asthma. The group investigated the effect of UDCA in vivo, in an ovalbumin (OVA)-driven eosinophilic airway inflammation mouse model. They observed that UDCA had the potency to suppress the eosinophilic inflammation by inhibiting the function of dendritic cells through the nuclear farnesoid X receptor.27 In our study, we firstly demonstrated the beneficial effects of UDCA on airway remodelling including epithelial thickness, sub-epithelial smooth muscle thickness and goblet cell hyperplasia. Furthermore, we also indicated the regulation of Th-2 immune response which led to lower levels of OVA specific IgE in serum and samples IL-4, 5, 13 in lung homogenates. We also observed the epithelial apoptosis in a murine model of asthma.
There is now strong evidence of the cytoprotective effects of UDCA in liver diseases because of its ability to reduce the apoptotic threshold in hepatocytes through modulation of classical mitochondrial pathways. The use of UDCA as an agent to treat non-liver diseases is associated with increased levels of apoptosis, such as neurodegenerative disorders, and it is a major consideration.28 In our study, we investigated effects of UDCA on the epithelial cell apoptosis in murine model of chronic asthma. We indicated that both doses of UDCA treatment had beneficial effects on the epithelial cell apoptosis compared to placebo, which was demonstrated by using TUNEL staining technique.
During the development of the asthma model, there is an infiltration of inflammatory cells. Inflammatory cells as well as structural cells secrete cytokines, including transforming growth factor (TGF-β), that regulate the airway remodelling process.29 TGF-β is a fibrogenic growth factor and it is particularly important because it plays a multifunctional role in the development of airway remodelling. TGF-β induces apoptosis in airway epithelial cells and it has a role in smooth muscle cells hyperplasia, enhancing goblet cell proliferation and mucus secretion during mucus hyper-secretion. Levels of TGF-β in the asthmatic airways are elevated and increased TGF-β expression is correlated with sub-epithelial fibrosis.30 Liang et al. studied the effect of ursodeoxycholic acid on TGF beta1/Smad signalling pathway in rat hepatic stellate cells. They suggested that UDCA can prevent the development of hepatic fibrosis via affecting the signalling pathway of TGFbeta1/Smad by inhibiting the expressions of TGF-beta1.31 In our study, we have shown that high-dose UDCA treatment significantly reduced the immunohistochemical scoring of TGF-β compared to the placebo in the lung tissue of the murine model of chronic asthma. In our opinion, the beneficial effects of high-dose UDCA treatment on airway remodelling and airway epithelial apoptosis may be a result of decreased synthesis of TGF-β in the lung tissue of murine model of chronic asthma. More detailed studies are needed for the clarification of its mechanisms in the lung tissue.
Matrix metalloproteinases, especially matrix metalloproteinase-9 (MMP-9), are extracellular proteases which degrade the extracellular matrix (ECM) during the remodelling of tissues. Han et al. indicated that MMP-9 was expressed by bronchial epithelium and it may be an important factor for airway eosinophil infiltration in asthma subjects.32 Studies with MMP-9-deficient mice challenged by allergen demonstrated that they had modest reductions in the peribronchial fibrosis. However, no reduction in mucus expression, smooth muscle thickness, or airway responsiveness was observed.33 In our study, we have shown that only a high dose of UDCA treatment significantly reduced the immunoscoring of MMP-9 in the lung tissue. In our opinion, high dose of UDCA can relieve the ECM deposition by inhibiting the smooth muscle thickening, goblet cell hyperplasia, and decreasing both immunohistochemical scoring of MMP-9 and TGF-b cytokines in the lung tissue of murine model of chronic asthma.
Angiogenesis is a prominent feature of the structural tissue remodelling that occurs in the chronic airway diseases, such as asthma.34 Vascular endothelial growth factor (VEGF) plays an important role in the vascular remodelling in the asthmatic airways. VEGF also induces allergic inflammation, enhances allergic sensitisation, and it has a role in Th2 type inflammatory responses.35 Sun et al. demonstrated that inhaled administration of budesonide triggered the anti-angiogenic activity through the inhibition of HIF-1α and VEGF expression in the murine model of asthma.36 Previous studies showed beneficial effects of UDCA on angiogenesis in different tissues. Suh et al. investigated effects of UDCA and its derivatives on anti-angiogenic activities by using the chick embryo chorioallantoic membrane. They demonstrated that the presence of UDCA or its derivatives inhibited the angiogenesis in a dose-dependent manner.37 In another study, Woo et al. suggested that systemically administered UDCA inhibited the choroidal neovascularisation in a laser-treated rat model.38 Our results showed no significant difference between UDCA treatments and placebo treatments in terms of immunohistochemical scoring of VEGF in the lung tissue of asthmatic mice.
Nitric oxide (NO) is a short-lived molecule that has been shown to have a number of important biological functions in various diseases, including asthma. In previous studies, anti-inflammatory effects of UDCA via inhibiting NO synthesis have been shown. Ma et al. investigated the effects of UDCA on NO production and the expression of inducible nitric oxide synthase (iNOS) on vascular smooth muscle cells isolated from adult rat aorta and rabbit coronary artery. They suggested that UDCA inhibited the induction of iNOS and then NO production in aortic and coronary artery smooth muscle cells, suggesting a possible mechanism for the cardiovascular protective effect of UDCA.39 In another study, Invernizzi et al. showed that UDCA can inhibit NO production in transformed human intestinal epithelial cells. They suggested that UDCA inhibited the induction of epithelial iNOS both in vitro and in vivo, and this effect may contribute to the anti-inflammatory and chemoprotective actions of UDCA in the colonic epithelium of rats treated with bacterial lipopolysaccharide.40 In our study, we found that both doses of UDCA suppressed NO levels in the lung homogenates of asthmatic mice.
No serious adverse effects of UDCA administration were reported in early controlled clinical trials in patients with gallstone disease41,42 or in long-term, large-scale, placebo-controlled trials in patients with cholestatic liver disease.43,44 A recent Cochrane review on UDCA in primary biliary cirrhosis revealed that there was no significant increase in total adverse events or severe adverse events in 10 controlled clinical trials.45 Diarrhoea was the single most frequent adverse event during UDCA treatment in patients with gallstone disease, and has been reported at an incidence of 2–9%.46,47 UDCA appears to be remarkably well tolerated.
There are some limitations of our study. We could not define the molecular mechanisms of UDCA on airway epithelium and we did not use any method for the evaluation of airway hyperresponsiveness. Instead, we histopathologically and serologically assessed the effects of UDCA on airway inflammation and remodelling.
In conclusion, although we could not evaluate the expression of cytokines and growth factors such as interleukins, NO, VEGF, TGF-β, MMP-9; we believed that the beneficial effect of UDCA on airway remodelling and epithelial apoptosis may be related to its ability to prevent synthesis of inflammatory cytokines and growth factors in the allergic airways. The ability of UDCA to modulate chronic asthma histopathology makes it a promising target for asthma therapy. However, further more detailed basic and clinical studies are needed for the evaluation of UDCA treatment in allergic airway diseases.
Conflict of interestWe, the authors of the manuscript, do not have any conflict of interest.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
We thank all authors of the study.
All procedures involving animal experiments which were performed in the study were in accordance with the ethical standards of the institution.