CD27, a lymphocyte specific member of the Tumour Necrosis Factor- Receptor (TNF-R) family is expressed on the majority of peripheral blood T cells. Activation of T cells via TCR/CD3 induces high CD27 surface expression and release of a soluble form (sCD27) of the molecule. sCD27 level increases in patients suffering from a variety of chronic inflammatory diseases. In the present study we aimed to measure both the serum sCD27 levels and CD27 expression on T cells in asthmatic patients, to evaluate the state of this molecule in allergic inflammation.
MethodsForty-three patients with asthma were included in to the study. CD27 molecule expression and soluble form of this molecule were analysed in atopic asthmatic (n:17) and non-atopic asthmatic (n:13) patients receiving inhaled corticosteroid treatment, in asthmatic patients whose treatment ceased at least for 6 months (n:13) and healthy control subjects (n:14).
ResultsThere were no differences in the expression of CD27 molecule on peripheral blood lymphocyte nor in its soluble form sCD27 levels in sera between the atopic asthmatic and non-atopic asthmatic patients receiving ICS treatment, treatment free asthmatic patients and healthy control subjects.
ConclusionsNeither the soluble form of CD27 nor its expression on T cells seem to be a reliable marker of atopic or non-atopic asthmatic inflammation.
Asthma is a chronic inflammatory disease of airways. T lymphocytes play an important role in the pathogenesis of asthma.1 Increased numbers of activated CD4+ T lymphocytes have been found both in blood and bronchoalveolar lavage fluid of asthmatic patients.2
CD27 and CD27 ligand (CD70) both belong to tumour necrosis factor receptor (TNF-R) superfamily, and appear to be related to functional differentiation programmes of T and B cells.3–6 CD27 is expressed on the majority of peripheral blood T and B cells.7,8 Although the function of the CD27 molecule is not known, in a previous study it has been reported that CD27/CD70 interaction augmented IgE production from CD27 B cells by enhancing B cell proliferation and differentiation into plasma cells9 and several experimental findings indicate that this molecule could play an important role in T cell activation.10,11 Moreover, activation of T cells via TCR/CD3 induces high CD27 surface expression. After prolonged activation in vitro, CD27 becomes gradually switched off.7,12 Antigen specific T cell activation also induces the release of a soluble form of CD27 (sCD27), probably as a result of proteolytic cleavage of CD27 transmembrane molecule.13,14 High levels of sCD27 have been detected in biological fluids taken from patients with B cell malignancies; chronic viral infections, such as HIV; and autoimmune disorders involving T cell hyperactivity, such as rheumatoid arthritis and systemic lupus erythematosus.15–17,8 Patients with multiple sclerosis also have increased levels of sCD27 in the cerebrospinal fluid.18 These findings suggest that sCD27 may be a useful marker in disorders where immune activation plays an important role.
Chronic inflammation of airways as a result of immune activation is a hallmark of asthma. Therefore analysis of the expression of activation antigen CD27 on peripheral blood T cells and its soluble form sCD27 may provide the state of this molecule in allergic inflammation. The aim of the present study was to evaluate the levels of soluble CD27 in sera together with the expression of CD27 on peripheral blood T cells in childhood asthma.
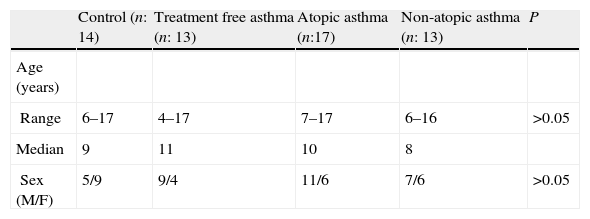
MethodsStudy PopulationForty-three patients with asthma who have been followed up at Ankara University, Paediatric Immunology-Allergy Department were prospectively studied. Seventeen atopic stable asthmatic and 13 non-atopic asthmatic patients receiving inhaled corticosteroid treatment (n:30) and 13 asthmatic patients whose treatment ceased at least for six months were included in the study. Atopic and non-atopic asthmatic patients were put together and named as ICS treated group. The characteristics of the study group are summarised in Tables 1 and 2.
Asthma diagnosis was based on International Paediatric Asthma Consensus Group Reports. Atopic status of these patients was defined by positive skin prick tests to extracts of common aeroallergens and/or serum specific Immunoglobulin E by ELISA (Adaltis, Rome, Italy). None of the patients had an acute asthma attack or a respiratory tract infection within the four weeks preceding the study and they have not been taking systemic steroids and/or immunotherapy during the study.
Fourteen healthy age-matched children (mean age: 6–17 years, 5 males, 9 females) without any atopic and infectious disease were enrolled as control group.
Laboratory StudiesSerum samples were taken from patients and healthy donors, by mean of venous puncture. While samples of flow cytometry were determined in the same day others were stored at −20°C for further use.
Soluble CD27 (U/ml) in sera was measured using a commercial ELISA kit (Bender MedSystems Diagnostics, Vienna, Austria), according to the manufacturer’s instructions.
CD27 expression (% of total lymphocytes) on different T cell subpopulations were analysed by double colour flow cytometry (EPICS XL-MCL, Coulter Coorp. Miami, FL, USA) using whole blood lysis method.
100μL of peripheral blood was put in to the 12×75mm sterile polystyrene tubes (Falcon Labware, Meylan Cedex, France) and incubated in dark at room temperature for 15min with appropriate monoclonal antibodies. Then red blood cell lysis, leukocyte stabilisation and fixation was done with Immunoprep A, B and C solutions at Coulter-Q-Prep Epics Immunology Workstation (Coulter Corb., 4235825-B, Hialeah, FI, USA) and analysed by double colour staining flow cytometry (EPICS XL-MCL, Coulter Coorp. Miami, FL, USA). Figures illustrating the gating strategy are shown in Figures 1 and 2. The monoclonal antibodies used in this study were CD27-PE (clone number; 1A4CD27), CD3-FITC/CD27-PE (clone number; UCHT1), CD4-FITC/CD27-PE (clone number; 13B8.2), CD8-FITC/CD27PE (clone number, B9.11.) CD19-FITC/CD27-PE (clone number; J4.119) CD45RA-FITC/CD27–PE (clone number; ALB11) and CD45RO-FITC/CD27-PE (clone number; UCHL1) (Immunotecht, Marseille, France). IgG1-FITC/IgG1-PE (clone number; 679.1Mc7) and IgG2a-FITC/IgG1-PE (clone number; U7.27/679.1Mc7) (Immunotecht, Marseille, France) were used as negative controls.
Statistical analysisSPSS 9.0 statistical pocket program was used for evaluation. Kruskal-Wallis and Oneway Anova tests were used to compare the groups.
ResultssCD27 levelsThere were no differences in sCD27 levels between the non-atopic asthmatic (89.7±46.5 n:13) and the atopic asthmatic patients (97.2±59.8 n:17) receiving inhaled corticosteroid (ICS) treatment, the asthmatic patients whose treatment had ceased for at least 6 months (84.3±21.9 n:13) and the healthy control group (70.7±18.3 n:14) (Fig. 3, Table 3).
CD27 molecule expression on various T cell populations (Percentage of total lymphocytes) and sCD27 levels
| Non-atopic asthma (n: 13) | Atopic asthma (n: 17) | Treatment free asthma (n:13) | Asthmatic Patients on treatment of ICS (The sum of atopic and nonatopic asthmatic (n: 30) | Healthy controls (n: 14) | P | |
| % of Total Lymphocyte (x±SD) | ||||||
| CD27+ | 46.9±9.9 | 49.2±5.2 | 44.3±6.5 | 48.2±7.6 | 44.3±6.5 | >0.05 |
| CD3+CD27+ | 47.9±7.1 | 48.4±5.6 | 44.7±6.8 | 47.3±6.3 | 45.5±9.3 | >0.05 |
| CD4+CD27+ | 30.2±4.6 | 31.2±5.08 | 27.8±3.1 | 30.8±4.8 | 31.6±8.3 | >0.05 |
| CD4+CD27− | 9.5±2.5 | 9.4±2.4 | 9.3±2.9 | 9.4±2.4 | 8.6±2.4 | >0.05 |
| CD8+CD27+ | 11.9±3.0 | 14.3±2.5 | 14.0±4.8 | 13.2±2.9 | 11.8±3.4 | >0.05 |
| CD19+CD27+ | 2.1±0.7 | 2.4±0.7 | 2.0±0.4 | 2.3±0.7 | 2.1±0.6 | >0.05 |
| CD45RA+ | 72.9±10.4 | 71.4±15.7 | 74.6±10.0 | 71.4±15.7 | 77.1±5.2 | >0.05 |
| CD45RA+CD27+ | 36.1±11.0 | 40.1±5.8 | 37.4±6.1 | 38.6±8.4 | 39.2±9.1 | >0.05 |
| CD45RO+ | 19.4±7.2 | 20.9±5.9 | 18.0±5.8 | 20.2±6.4 | 16.0±5.5 | >0.05 |
| CD45RO+CD27+ | 10.0±3.6 | 11.3±2.8 | 9.9±3.2 | 10.7±3.2 | 8.2±2.9 | >0.05 |
| CD45RO+CD27− | 9.1±4.2 | 9.2±3.8 | 7.6±3.1 | 9.1±3.9 | 7.4±2.9 | >0.05 |
| sCD27 (U/ml) (x±SD) | ||||||
| sCD27 (U/ml) | 89.7±46.5 | 97.2±59.8 | 84.3±21.9 | 93.9±53.7 | 70.7±18.3 | >0.05 |
Atopic and non-atopic asthmatic patients were put in the same group as receiving ICS treatment and compared to asthmatic patients whose treatment ceased at least 6 months before and the control group. There were no differences in sCD27 levels between the asthmatic patients on (93.9±53.2 n:30) or off (84.3±21.9 n:13) ICS treatment and the healthy control subjects (70.7±18.3 n:14) (Table 3).
CD27 expression on peripheral blood T lymphocyteAs shown in Table 3, in non-atopic asthmatics and atopic asthmatics receiving ICS treatment, asthmatic patients whose treatment had ceased for at least 6 months and the control group CD27+ T cells, CD3+CD27+ T cells, CD4+CD27+ T cells, CD4+CD27− T cells, the CD8+CD27+ T cells, CD19+CD27+ B cells, CD45RA+ T cells, CD45RA+CD27+ T cells, the CD45RO+ T cells, CD45RO+CD27+ T cells, CD45RO+CD27− T cells were similar for each parameter.
The same parameters above were also compared in asthmatic patients receiving ICS treatment (this group is the sum of atopic and non-atopic asthmatic patients receiving ICS treatment), asthmatic patients whose treatment had ceased for at least 6 months and the control group as tree groups. No differences were found in asthmatic patients receiving ICS treatment, asthmatic patients whose treatment ceased at least 6 months and the control group in CD27+ T cells, CD3+CD27+ T cells, CD4+CD27+ T cells, CD4+CD27− T cells ratio, CD8+CD27+ T cells ratio, CD19+CD27+ B cells, CD45RA+ T cells, CD45RA+CD27+ T cells, CD45RO+ T cells, CD45RO+CD27+ T cells, CD45RO+CD27− T cells (Table 3).
CorrelationNo correlation was observed between the sCD27 levels in sera and the expression of CD27 on different T lymphocyte subtypes.
DiscussionRelatives of tumour necrosis factor receptor family prove to be of crucial importance for an effective immune response as well as maintenance of homeostasis. The diagnostic and prognostic value of the occurrence of these receptors and their soluble forms is becoming increasingly apparent. Lesser known CD27 is a lymphocyte specific member of the TNF receptor superfamily. In vitro experiments show that T cell stimulation via the TCR/CD3 complex results in a transient increase in CD27 expression and a subsequent decrease in the expression of CD27.7,12 After persistent antigenic stimulation CD45RO+CD27+ T cells convert to CD45RO+CD27−.3
In this present study CD27 molecule expression and soluble form of this molecule were analysed in atopic asthmatic and non-atopic asthmatic patients receiving ICS treatment (separately or together), in asthmatic patients whose treatment had ceased for at least 6 months and healthy control subjects; and no differences were found in CD27 membrane expression on peripheral blood T lymphocyte between the groups.
As far as we know there was no other report which evaluated the CD27 molecule expression on peripheral blood T lymphocyte in asthmatic children in literature. It has been reported that a large number of CD4+CD27+ T cells in the rheumatoid synovial perivasculer lymphocytic infiltrate a relative increase in the percentage of CD27–T cells in the diffuse lymphocytic infiltrate, and an increased percentage of CD4+ CD27− cells in synovial fluid. This might suggest a continuous influx of preactivated CD4+CD45RO+CD27+ cells from the peripheral blood into the synovial tissue of patients with rheumatoid arthritis and subsequent further activation and differentiation to CD4+CD45RO+CD27− cells in situ followed by migration to the synovial fluid.17 Similar results were also reported by Gattarno et al. in juvenile idiopathic arthritis.19 An increase in the percentage of CD27− cells within the CD4+ subset has been observed in the bronchoalveolar lavage fluid in comparison with peripheral blood of patients with sarcoidosis.20 In all these reports the CD27 expression was also evaluated in target tissue.
In contrast, in this present study, CD27 molecule expression was analysed only in peripheral blood T lymphocyte instead of in comparison with bronchoalveolar lavage fluid in different groups because of ethical issues. As a result the expression or lack of CD27 could not be evaluated on target tissue. Lacking of CD27 membrane expression might be restricted to the end organ. That might be an explanation for similar results of lacking of CD27 molecule expression on peripheral blood between the different groups.
There is evidence that in atopic asthmatic patients, atopic Th cells subgroup occurs as a result of persistent allergen exposure. Atopic Th cells which have been persistently stimulated by antigen accumulate within the CD4+CD45RO+CD27− subset.21,22 According to this, increasing in CD27− cells subset might be expected in atopic asthmatic patients. Here we analysed the CD27− cells as CD4+CD27− and CD45RO+CD27− cells. There were no differences in atopic and non-atopic asthmatic patients and in healthy control group in the mean of CD4+CD27− and CD45RO+CD27− T cells. Although a kind of difference is observed in clinical presentation in atopic and non-atopic asthma, the immunopathological changes are similar. Similar Th2 cytokine profiles have been shown in airway biopsies in atopic and non-atopic asthmatic patients.23 Since they share the common immunopathology, no differences were observed between the atopic and non-atopic asthmatic children in the mean of CD4+CD27− and CD45RO+CD27− T cells.
In this report both atopic and non-atopic asthmatic children receiving ICS were stable asthmatic. The asthmatic patients whose treatment ceased at least 6 months since their asthma symptoms were already under control were served as treatment free asthmatic patients. Accordingly inflammation was under control in all groups. This might be another explanation for similar results observed in CD27 membrane expression between the groups and in comparison to healthy control subjects.
The present study was conducted to evaluate the potential usefulness of sCD27 in sera of children with asthma. There were no differences in sCD27 levels in sera not only between the atopic and non-atopic asthmatic patients but also between the patients receiving ICS treatment and treatment free asthmatic patients in comparison to healthy subjects. There is only one report evaluating the sCD27 levels in sera of asthmatic adults according to our review of the literature. In this previous study significantly higher levels of sCD27 were found in patients with asthma.24 Reasonable sCD27 levels were also significantly higher in active asthmatic patients. Active asthmatic and inactive asthmatic patients were put into the same group and compared to the healthy control group. Consequently the higher sCD27 levels in active asthmatic patients resulted with higher sCD27 levels in asthmatic patients in comparison to healthy control subjects. Unfortunately it was seen that there were no significant differences between the stable asthmatics and the control group.
Higher sCD27 levels in sera of active SLE patients have been reported in comparison to in remission SLE patients and higher sCD27 levels in sera of juvenile idiopathic arthritis patients than in healthy controls.16,19 As mentioned above, all asthmatic patients presented in this study were stable asthmatic with or without ICS treatment. It seems reasonable for similar sCD27 levels to result between the groups.
Consequently, there were no differences in the expression of CD27 molecule on peripheral blood lymphocyte nor in its soluble form sCD27 levels in sera between the atopic asthmatic and non-atopic asthmatic patients (separately or together) receiving ICS treatment, the treatment free asthmatic patients and the healthy control subjects.
A limitation of this study was the use of two colour staining protocol for flow cytometry. To minimise the mistakes related to the T-cell measurements1; all evaluations were done in lymphocyte gate which is confirmed by CD45/CD14 gating strategy2 isotype control was used for each and every experiment,3 to be sure of the cells, in other words to check CD4 or CD8 molecule expressions on T lymphocytes a double-colour T lymphocyte protocol; CD3+CD4+ and CD3+CD8+ were added in some of the studies. On those patients it has been shown that the percentage of CD3+CD4+ or CD3+CD8 double-positive cells were almost equal to CD4 or CD8 molecule expression in CD4+CD27 or CD8+CD27 double-colour studies. A more recent technology, three-colour staining, would have been more appropriate in defining T-cells and this is planned as a further study.
In conclusion, neither the soluble form of CD27, nor its expression on T cells seem to be reliable markers of Th2 type inflammation. More importantly, these parameters may not be considered as a marker of defect in the immunoregulation of stable asthma.
Further research needs to focus on CD27 expression in bronchoalveolar lavage fluid and sCD27 levels in sera of symptomatic patients for asthma to evaluate the role of this molecule in asthma pathogenesis.
Conflict of interestNone of the authors has a financial or proprietary interest in any method or material mentioned in the text.
None of the authors has a financial or proprietary interest in any method or material mentioned in the text.