Allergy to propolis seems to be rare and little is known about it.
ObjectiveThe aim of the study was to survey a subset of affected beekeepers to determine aspects such as time of onset of disease, comorbidity, and possible methods of prevention.
MethodsWith the help of two German journals for beekeepers we contacted 41 beekeepers with propolis allergy. They were sent a questionnaire which assessed several aspects of the disease and was based on the current literature.
Results70.7% returned our questionnaire and had clear signs of propolis allergy with positive testing by their local allergologists. They reported that allergy had developed after an average of 9.5 years beekeeping. We also found a high prevalence of other allergies (72.4%). Interestingly, there were also systemic reactions to propolis in some beekeepers but not necessarily when using propolis as a medication against other diseases. Beekeepers believed that solvents used to clean the hands could play a role in the development of the disease.
ConclusionThis study provides new insights into allergy to propolis. The hypothesis that solvents used to clean the hands could play a role in the development of the disease should be addressed in future studies.
In 1915, the first case of propolis allergy was described in a beekeeper. Today there are many reports on the subject of propolis allergy in the literature and its incidence may be increasing, because propolis is an ingredient of many ‘over the counter’ products, including cosmetics, toothpastes and ointments, and it is increasingly used as a dietary supplement. The frequency of propolis allergy in patients with contact allergy from unknown causes is reported to be 1.2 to 6.6% and there is a possible link to pollen allergy1,2. A recent case series on propolis allergy in beekeepers showed that beekeepers often do not recognise the problem and continue their hobby without protecting themselves from contact with the substance3. It also found that allergic beekeepers even use propolis as a medication for other disorders and identified the presence of benign lung diseases, allergies other than propolis, and psychological instability as factors associated with the likelihood of suffering from propolis allergy3. Regarding lung diseases, a recent publication showed that topical spread of propolis on nasal mucosa as an adjuvant therapy for asthma for 6 months mimicked lung cancer due to the development of a pulmonary tumour in the left lower lobe with satellite nodules, mediastinal lymphadenopathy, and even an increase in the tumour marker CEA4.
Since our earlier study did not specifically focus on propolis allergy we initiated a new study in order to gain a better understanding of the problems associated with it5.
MethodsStudy questionnairesAs there were no previous studies except our own we developed the “QABH-propolis allergy”, which supplemented the previously used Questionnaire for the Assessment of Beekeepers’ Health (QABH)3,5,6. The questionnaire was tested in 10 volunteers for intelligibility. A copy of the questionnaire is available from KM.
SubjectsWe asked readers of the major beekeeping journals Die Biene, Der Imkerfreund, ADIZ, and the Deutsches Bienenjournal with an allergy to propolis to contact us, if they were prepared to complete the questionnaires. A total of 41 beekeepers contacted us. They were sent a questionnaire based on the current literature and which assessed several aspects of the disease. Furthermore, they were asked if they were willing to allow us to contact their treating physician if further clarification was required.
Statistical analysisSPSS version 14.0 (SPSS, Chicago) was used for data management and statistical analysis. A p-value of less than 0.05 was considered significant.
Ethical approvalThe study was submitted to the ethics committee of the Justus-Liebig-University Giessen, Germany. The project was approved on September 19th, 2006 (application number 113/06).
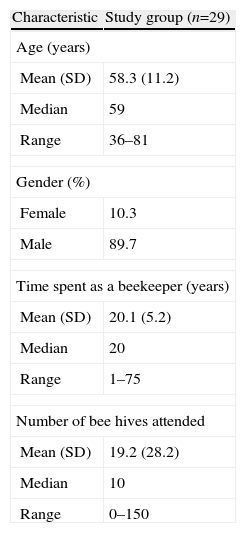
ResultsWe were contacted by 41 beekeepers. Twenty-nine of these (70.7%) returned the questionnaire and had clear signs of propolis allergy. The characteristics of the responding beekeepers are given in the Table 1.
Demographic characteristics of the beekeepers with allergy to propolis
| Characteristic | Study group (n=29) |
| Age (years) | |
| Mean (SD) | 58.3 (11.2) |
| Median | 59 |
| Range | 36–81 |
| Gender (%) | |
| Female | 10.3 |
| Male | 89.7 |
| Time spent as a beekeeper (years) | |
| Mean (SD) | 20.1 (5.2) |
| Median | 20 |
| Range | 1–75 |
| Number of bee hives attended | |
| Mean (SD) | 19.2 (28.2) |
| Median | 10 |
| Range | 0–150 |
Beekeepers had suffered from allergy to propolis for 7.4 years on average (SD 6.2; range 1–23 years). However, beekeepers were not confronted with the disease when they first began beekeeping. On average, allergy to propolis started after 9.5 years of beekeeping (SD 9.0; range 0.1–35.0 years). In most cases, the diagnosis was verified by skin tests. Interestingly, one person reported that he had had repeated skin reactions on his hands although the skin test failed to verify the allergy to propolis. In two cases (6.9%) family members were also allergic to propolis. Two beekeepers (6.9%) suffered from atopic dermatitis and 21 (72.4%) were allergic to other substances as well, most frequently to grass pollen (n=6; 20.7%), bee venom (n=4; 13.8%), and perubalsam (n=3; 10.3%). Allergy to bee dust was not found in this group.
Reactions to propolis occurred after various time intervals ranging between 5min and 48h (mean 10.9h, SD 13.9h, median 5h). The various types of reactions reported are shown in Figure 1. This shows that allergy to propolis in beekeepers is not only a local problem but may cause systemic reactions as well. These may be less severe (urticaria and difficulty swallowing) or more severe (dyspnoea). The symptoms lasted for different time intervals ranging from 5h to 20 days (mean 4.6 days, SD 4.7 days, median 3 days). Symptoms in beekeepers worsened over time in seven cases (24.1%), improved in six cases (20.7%) and remained the same in the remaining cases. In four cases (13.8%) symptoms were more severe or less severe in spring after beekeepers had less contact with propolis.
We asked the beekeepers what measures they took in order to prevent the problems of propolis allergy. All of them proved to be effective. The majority always wore rubber gloves (n=12; 41.4%) or leather gloves (n=5; 17.2%), some wore gloves only occasionally (n=10; 34.5%), and two never wore gloves (6.9%). In the latter two cases, sensitivity to propolis was present but not when in contact with the hands. Six (20.7%) beekeepers regularly used protective ointments on the hands prior to working on the bees, and four (13.8%) used ointments only occasionally. Only one beekeeper (3.4%) tried to keep hives with low propolis production and four intentionally did not do so because they collected propolis for their own medical purposes.
Beekeepers who consulted a physician were counselled to give up beekeeping in 37.5% (9/24) of cases or to wear protective gloves (54.2% (13/24)). The beekeepers were also asked how they would advise other beekeepers with propolis allergy. Three (10.3%) would advise quitting beekeeping and 19 would advise wearing protective clothing (gloves).
In our earlier study we found that a considerable number of beekeepers use propolis as an unconventional medication for several illnesses5. In this study, eight (27.6%) beekeepers used propolis as an oral medication to a lesser or greater extent. When taken in the form of an ethanolic extract these beekeepers did not experience side effects.
Twenty-two beekeepers (75.9%) wished that physicians and beekeeper organisations would provide more information or were better informed about propolis allergy. We also asked the beekeepers what means helped them with propolis allergy. Unconventional treatment approaches such as homoeopathy and apitherapy were not considered to be effective. Finally, they were asked what they believed to be the cause of propolis allergy. An interesting answer was that they considered the solvents used to remove propolis from the hands to be responsible for the allergy and suggested that no organic solvents should be used.
DiscussionThis study confirms that some beekeepers continue beekeeping even when confronted with propolis allergy. It also shows that the development of contact dermatitis to propolis can develop even after many years and can both worsen and improve over time. Interestingly, we found that contact dermatitis to propolis is not necessarily a generalised phenomenon but may be restricted to certain parts of the body only and may not affect the ingestion of propolis as a potential medical treatment. On the other hand, propolis allergy may also cause systemic reactions. Beekeepers who continue beekeeping mainly wear protective gloves in cases of propolis allergy of the hands.
Today, questions remain on how to deal with propolis allergy. Like other contact allergies there is no treatment such as that available for systemic allergies like bee sting allergies. Thus, the only option is to avoid the antigens, which is practised by most affected beekeepers already. In spite of the possibility of severe reactions, beekeepers continue with their hobby. Unfortunately there is no information on the percentage of beekeepers continuing and those quitting their hobby. However, such behaviour is not surprising as similar behaviour has been observed previously in cases of bee venom allergy3,6–10.
This study confirms our earlier study and a very recent one which focused on propolis allergy associated with the presence of other allergies which may also cause systemic reactions2,3. In the cases studied, these reactions occurred during the administration of propolis-containing solutions for the treatment of upper respiratory tract infections2. These solutions are most likely to be ethanolic, which could perhaps partially support the hypothesis presented by the beekeepers, who considered that the solvents used to clean the hands facilitated the development of contact allergy. This hypothesis may explain how the antigen is transported into the deeper layers of the skin where it can lead to sensitisation. It is also in accordance with a study on the epidermal penetration of parabens depending on the type of solvent, and work which shows that propolis is absorbed after oral ingestion11,12. This hypothesis should be addressed in future studies in order to avoid the development of allergy to propolis.
In the meantime it may be reasonable for beekeepers with a history of atopic diseases and other types of allergy not to use solvents to remove attached pieces of propolis.
We thank all participating beekeepers, the Deutscher Landwirtschaftsverlag and the Deutsche Bauernverlag for their support by printing our request for beekeepers to support our study as well as Dr. Christina Fischer and Christina Husemeyer for their support during the development of the questionnaire.
Conflict of interest
The authors have no conflict of interest to declare.




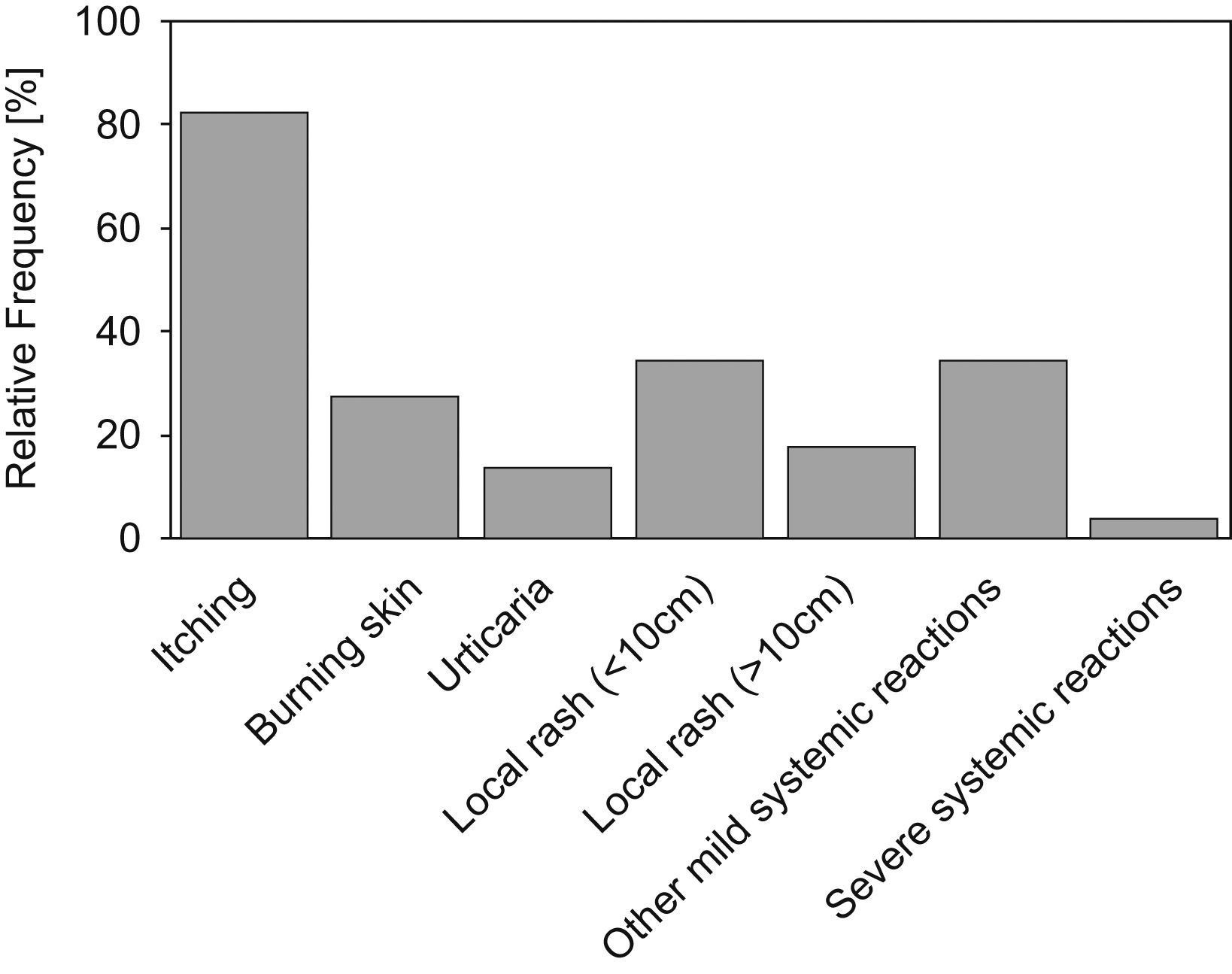
![Types of reactions reported by beekeepers with propolis allergy [n=29]. Types of reactions reported by beekeepers with propolis allergy [n=29].](https://static.elsevier.es/multimedia/03010546/0000003700000006/v2_201308271547/S0301054609000603/v2_201308271547/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
