Benzodiazepines are a group of psychoactive drugs whose core chemical structure is the fusion of a benzene ring and a diazepine ring. They are widely used as anaesthetics, hypnotics, anxiolytics, anticonvulsants, and muscle relaxants. In general, benzodiazepines are safe. The most common adverse reactions are neurological and gastrointestinal disorders and skin manifestations are rare.1,2
We present the case of a 79-year-old man referred to our department because one month before he had presented a muscular contracture and he started treatment with ibuprofen 600mg each eight hours and tetrazepam 50mg per day. After four days taking both drugs simultaneously, he complained of widespread itchy micropapular rash. He stopped using the drugs and was admitted to the emergency room of our hospital, where he was treated with oral antihistamines and oral corticosteroids. The symptoms resolved completely after two weeks with scaling. The patient denied personal or familial history of atopy.
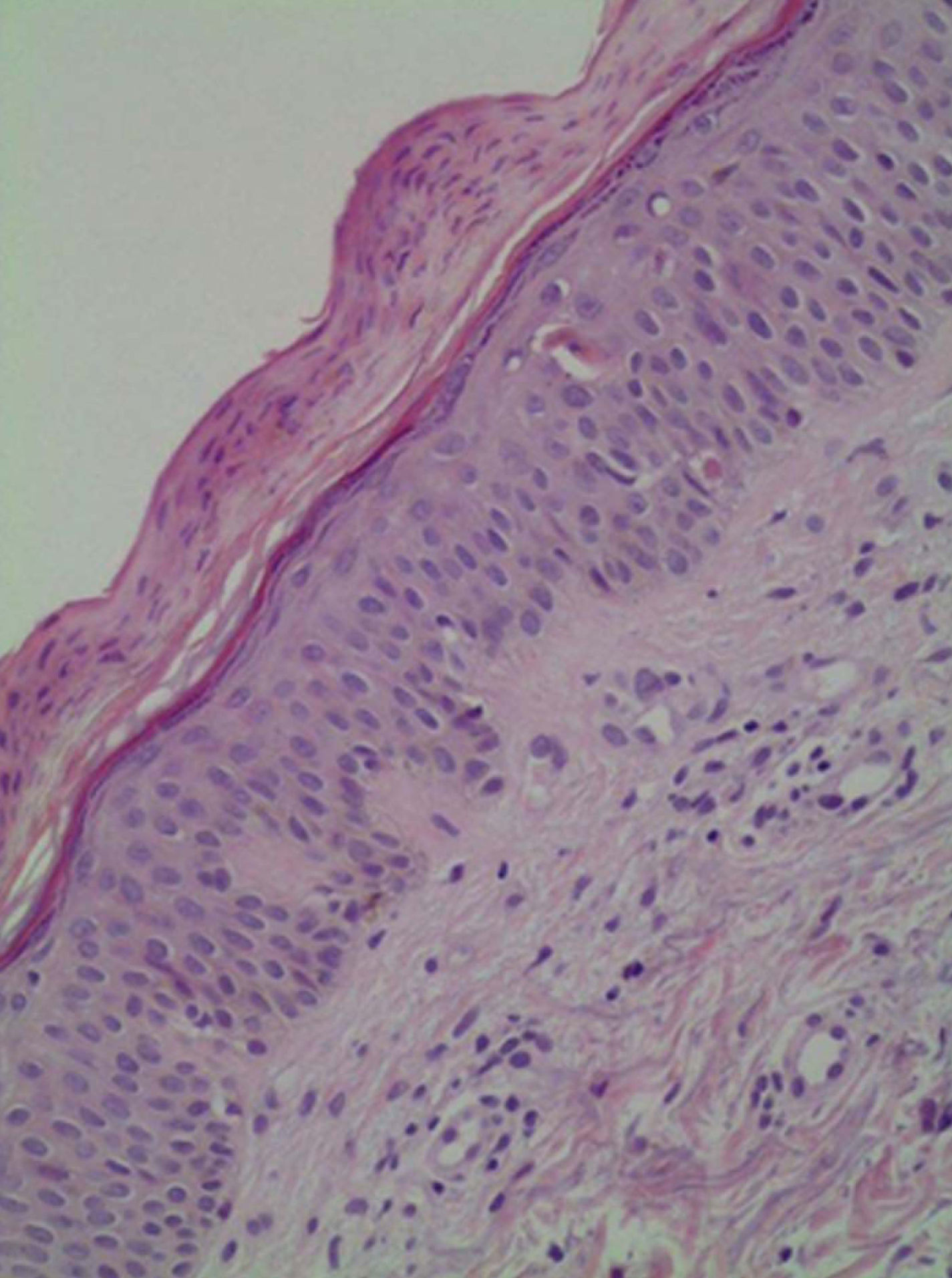
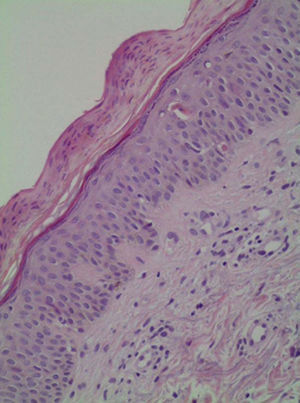
Histological analysis of a punch biopsy of affected skin showed parakeratosis of stratum corneum with vacuolar degeneration and diskeratinocytes, and isolated eosinophils in superficial dermis with no other inflammatory components (Fig. 1). Those findings suggest an eczematous dermatitis caused by drug.
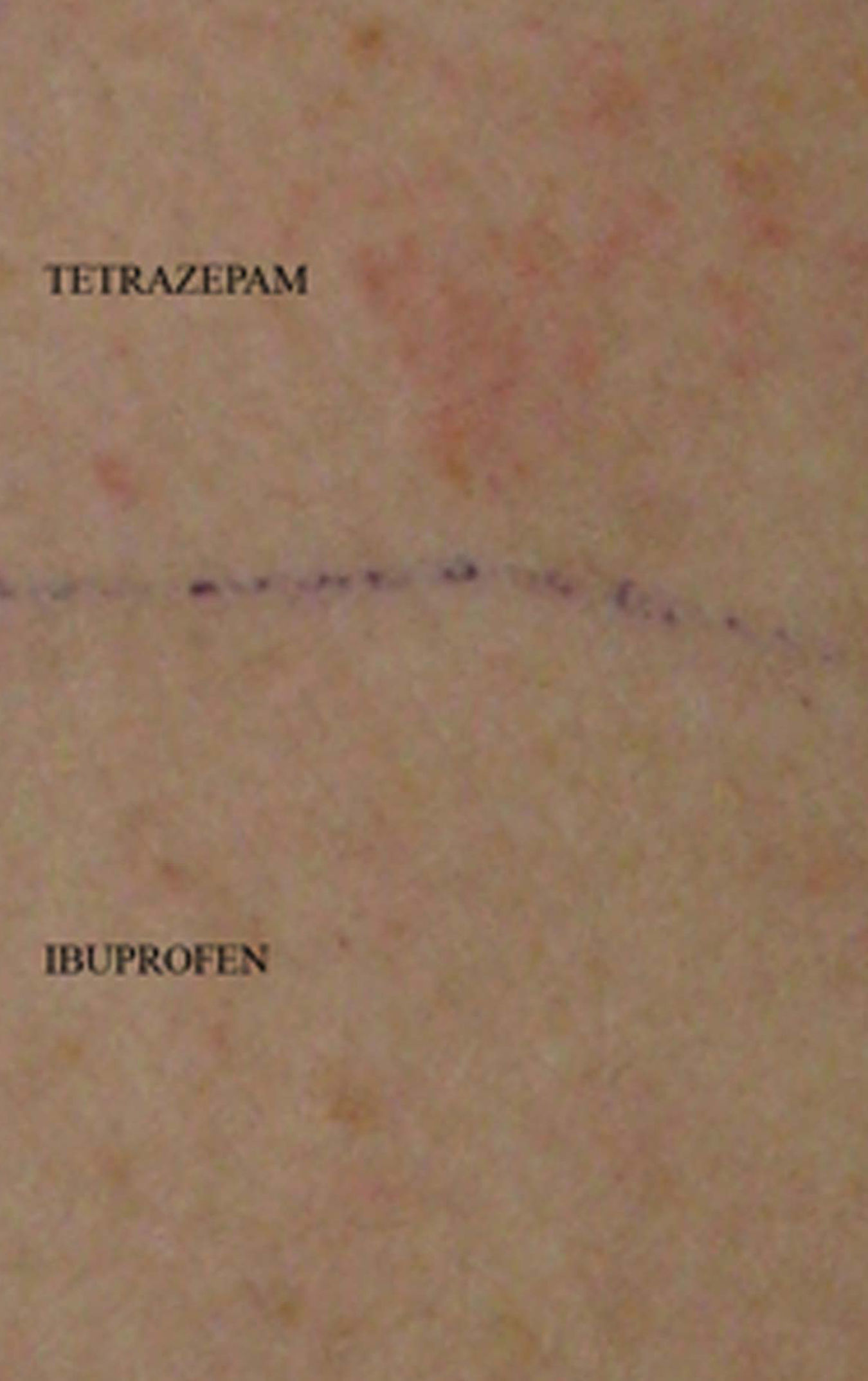
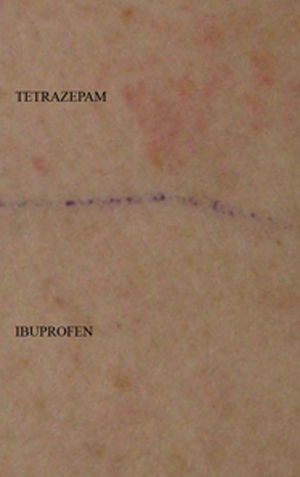
Patch tests were performed with the standard series (by True Test®, Mekos Laboratories ApS, Hillerod, Denmark) and with ibuprofen, tetrazepam, diazepam, clonazepam, midazolam, bromazepam, lorazepam, and lormetazepam (5% petrolatum). They were read at 48 and 96h and were applied to the skin on his upper back. Patch testing with tetrazepam (+++) was positive (Fig. 2), showing a negative result to all the standard series and to the rest of the drugs tested.
The patient gave his consent for challenge tests. A single-blind placebo-controlled drug challenge performed with 600mg ibuprofen was negative.
To investigate a possible cross-reactivity between benzodiazepines, we also performed oral challenge on different days with diazepam 5mg, lorazepam 5mg, and midazolam 7.5mg with negative result. Therefore, we recommended the use of those drugs for future treatments.
Skin reactions caused by tetrazepam are unusual, but maculopapular exanthema,2,3 systemic dermatitis,1 fixed drug eruption, urticaria,3 erythematous rash,4 photodermatitis reactions,4 contact dermatitis,5,6 leukocytoclastic vasculitis, toxic epidermal necrolysis, generalised pustulosis,2 erythema multiforme,7 and Stevens–Johnson6,8 syndrome have been reported in association with tetrazepam. No cases of chronic eczematous dermatitis have been described.
Epicutaneous patch testing is a useful tool to confirm tetrazepam allergy.2,9 In our case, tetrazepam patch test was positive but the rest of tested benzodiazepines were negative.
Previous reports2 suggest that there is no cross-reactivity among benzodiazepines. Diazepam is the most similar benzodiazepine to tetrazepam, the only difference between them is the presence at position 5 on the diazepine ring of phenyl in diazepam and clohexen in tetrazepam, and this cyclohexene conformation could explain tetrazepam sensitisation.9 Our patient also tolerated oral administration of diazepam and other benzodiazepines. Due to the biopsy result and the positive patch test, an oral challenge with tetrazepam was not performed.
We have reported a type IV hypersensitivity reaction confirmed by biopsy as an unusual chronic eczematous reaction caused by tetrazepam with probed tolerance to other benzodiazepines.