When a child is diagnosed with a food allergy, prevention and patient education are the key interventions for maintaining the child's health and quality of life and that of his or her whole family. However, health education activities for the families of children with food allergies are very limited, and most of these activities have not been evaluated. Therefore, the objectives of the present study were to develop an educational programme, to empower its participants through workshops, and to evaluate its results.
MethodsSeveral types of educational materials were created specifically for the programme, called “Proyecto CESA” (“STOP-FAR Project: Stop Food-Induced Allergic Reactions”). The programme was carried out in seven Spanish cities and was attended by parents and caregivers. The workshops were led by physicians specialising in allergies and by expert patients. Afterwards, participant learning and satisfaction were evaluated based on questionnaires that were completed both before and after the workshops.
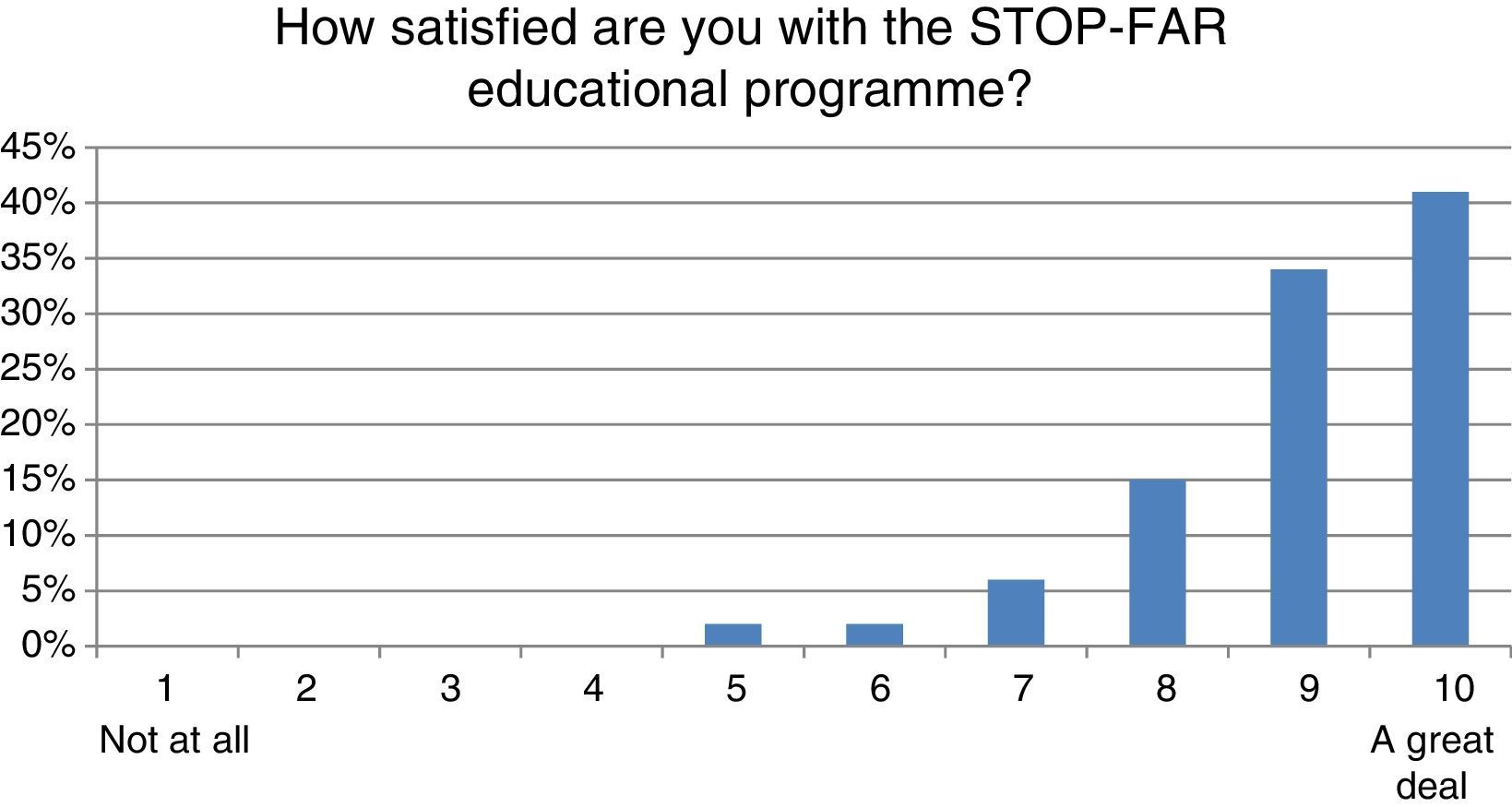
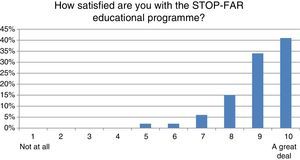
ResultsA significant improvement was observed in 29 items out of 40 (McNemar's test). Participant satisfaction with the programme was also very high: 90% rated the course between 8 and 10 points out of a possible 10 (41% rated it as a 10).
ConclusionThe face-to-face workshops, which included utilisation of educational materials, had positive results in terms of learning as well as in levels of satisfaction in participating families.
Food allergy is one of the most common chronic diseases in childhood, affecting 4–8% children.1–3 In certain cases, its symptoms are serious and even life-threatening,1,4,5 causing a noticeable decrease in quality of life (QoL) as it relates to health.6 However, with education and appropriate care, food allergy-related morbidity in children is generally low, and mortality is relatively rare.7
Although the principal treatment for food allergy still consists in avoiding the allergen, oral desensitisation may be recommended in certain cases.8–10 Following diagnosis, parents and children often experience a period of adaptation and psychosocial reckoning.11 In particular, the whole family's activities are limited because of the child with food allergy. Additionally, Sicherer et al. found that parents’ perceptions of their family's general health diminished if they had a child with food allergy when compared with parents of children in the general population.12
To avoid allergic reactions, parents and caregivers must have information about certain tools to manage the condition.1,13 Therefore, when a child is diagnosed with food allergy, patient education is a key intervention for maintaining the health and QoL of the child and of his or her whole family.1,14
The objective of education about food allergies is to train parents and children to manage the condition.4 This entails giving them the knowledge and skills needed both to prevent reactions and to know how to treat these reactions in the event that they do occur.3,4 Although school-aged children are able to learn self-management skills for their allergies, they need their parents to share responsibility for managing the condition.15
The principal frustrations that parents experience include a lack of social comprehension, inconsistent medical information, and inadequate product labelling.12
Patient education for the families of children with food allergies should be offered as a standard part of treatment. Nevertheless, for various reasons, patient education is often unavailable or insufficient.16–18 In reality, health education programmes are either very limited or non-existent in the majority of the health centres where these patients are seen.19
Greenhawt et al.20 remind us that as allergy specialists, our responsibilities must also include preparing families to face the difficult task of raising a child with a food allergy. In the school context, it is also necessary to promote collaboration with the non-allergic community to better keep allergic children safe while at the same time imposing the lowest number of restrictions possible.
Families occasionally turn to patient organisations or perform Internet searches in order to meet their needs for information and support. Thus, in many cases, information is acquired in a haphazard way or without the patients having established clear goals. However, the materials used in educational activities are rarely evaluated by professionals.17,21 The objectives of the present study were to develop an educational programme, to empower its participants through workshops, and to evaluate its results.
Materials and methodsStudy toolThis educational programme is part of a programme known as “Proyecto CESA” (“STOP-FAR Project: Stop Food-Induced Allergic Reactions”). CESA is a Spanish acronym representing four words: Know, Avoid, Symptoms, and Epinephrine. Workshops were held in seven major Spanish cities (Madrid, Barcelona, Valencia, La Coruña, Murcia, Granada, and Málaga) over two consecutive weekends in November 2012.
The project team was composed of researchers, health professionals, nurses, doctors specialising in allergy treatment, and expert parents of patients (parents of allergic children) who were members of the main Spanish patient associations: AEPNAA, Immunitas Vera, and Elikalte. The team, in keeping with the Participative Medicine model,22 shared in decision-making,23 held a number of meetings to design the study, developed the educational materials and questionnaires used, and discussed and evaluated the results.
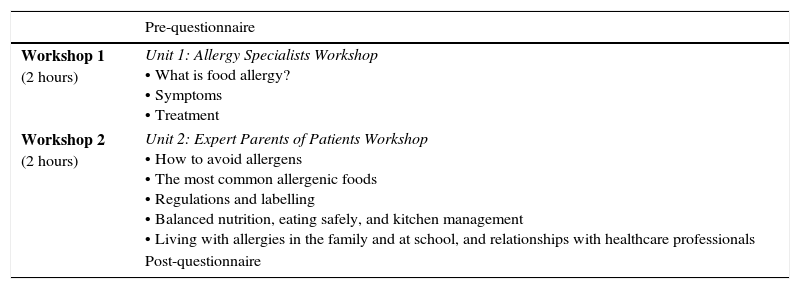
Educational materialsA variety of materials was created specifically for this project, including seven educational videos and additional video support for parents and caregivers, which were developed by physicians specialising in allergies and by expert parents of patients, using the Participative Medicine methodology. These materials were based on a bibliographic review and on expert opinions in allergy and education. All materials used were the same in every city and covered different topics, from clinical aspects to general management of the condition (labelling or school, and so on) (see Table 1). All the items in the evaluation questionnaires were explicitly addressed in the materials.
Units of the educational programme.
| Pre-questionnaire | |
|---|---|
| Workshop 1 (2 hours) | Unit 1: Allergy Specialists Workshop • What is food allergy? • Symptoms • Treatment |
| Workshop 2 (2 hours) | Unit 2: Expert Parents of Patients Workshop • How to avoid allergens • The most common allergenic foods • Regulations and labelling • Balanced nutrition, eating safely, and kitchen management • Living with allergies in the family and at school, and relationships with healthcare professionals |
| Post-questionnaire | |
In addition, an illustrated story was created for children to explain the most important concepts related to food allergies using age-appropriate language. Four storytelling videos and other educational activities were also developed for children. Children were not evaluated in our study. All materials are available on our online platform for future editions of the educational programme.
Study populationThe participants in the study were parents of children with food allergy, from seven different cities in Spain. They were recruited using patient association communication channels, including web sites and social networks. A total of 184 participants were included and participated in the first workshop; 174 of whom finished the programme in the second workshop and were included in the data analysis.
Intervention: workshopsThe programme's content was divided into two units (see Table 1). One unit was covered per workshop, on two consecutive weekends. The first included health information and clinical aspects of the disease and was led by allergy specialists, and the second covered practical skills for managing food allergies and was led by expert parents of patients. Each workshop lasted approximately two hours, including a question-and-answer period led by local allergists and expert parents from each city. The same materials and activities were used in all of the cities.
Expert patients are typically defined as people living with chronic conditions who are able to take more control over their health by understanding and managing their conditions, leading to an improved QoL. There is evidence that people with experience in self-management tend to be more confident and less anxious.24 Empowered patients also make fewer visits to the doctor, can communicate better with health professionals, take less time off from work, and are less likely to suffer acute episodes requiring hospital admission.25
Even though children's learning was not evaluated, educational activities were also organised for children (led by monitors from the patient associations). These activities were not subject to evaluation, given that any assessment was likely to have been unreliable, due to the young age of the children in the sample.
EvaluationTrial design: Pre-test/post-test study. Due to the complete lack of instruments developed for this purpose in the literature, evaluation was carried out via ad hoc questionnaires created for the programme based on a bibliographic review and on expert opinion in allergy and education. The questionnaire used to evaluate food allergy knowledge had 40 items. All the items in the evaluation questionnaires were explicitly addressed in the educational materials. To assess satisfaction with the educational programme, a five-item Likert-scale inventory, ranging from “not at all” to “a great deal,” was used. A space for comments was also included.
A statistical analysis was initially carried out through a descriptive analysis of the sample. For data analysis, pre- and post-workshop questionnaire answers were compared using SPSS statistical software. McNemar's test was used to detect statistically significant differences between the proportions of correct and incorrect answers between pre-test and post-test knowledge, taking a significance level of p<0.05.
STOP-FAR Project is a broad-scale educational programme, but in this paper we have included only the results of the workshops.
EthicsThe research project met all methodological requirements and was approved by the Research Ethics Committee of the La Paz University Hospital, Madrid (Spain). The project also received the joint approval of scientific societies involved in the treatment of this condition, such as the Spanish Allergy Society (SEAIC, http://www.seaic.org/), the Society for Clinical Paediatric Allerology and Immunology (SEICAP, http://www.seicap.es/), and the Spanish Association of Paediatrics (AEP, http://www.aeped.es/).
ResultsThe initial study population included 184 parents and caregivers from the cities of Madrid (28), Barcelona (40), Valencia (25), Murcia (24), La Coruña (25), Málaga (23), and Granada (19). They were accompanied by 103 boys (55.7%) and 82 girls (44.3%) with allergies and an average age of 4.86 years. The participants included 103 mothers (56%), 72 fathers (39.1%), and nine caregivers (4.9%). Participation was considered satisfactory; the objective was to have a sample with a similar number of participants for every city and region of Spain.
A total of 174 parents and caregivers completed the educational programme's pre-workshop questionnaire (first workshop), as well as completing the second workshop and the post-workshop questionnaire. We lost only ten parents from the study sample, primarily because they were unable to attend the second workshop.
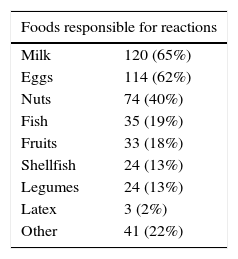
The foods most frequently responsible for reactions (see Table 2) were milk (65%), eggs (62%), nuts (40%), fish (19%), fruit (18%), shellfish (13%), legumes (13%), latex (2%), and other foods (22%), which is consistent with the most common allergenic foods among children in Spain (36).
Before the workshop, participants were asked if they had received sufficient training on food allergies, and 111 participants (60.3%) answered affirmatively. The principal sources of information were healthcare professionals (physicians and nurses) (70%), Internet searches and forums (57%), patient associations (57%), books and other written materials (28%), and other sources (2%).
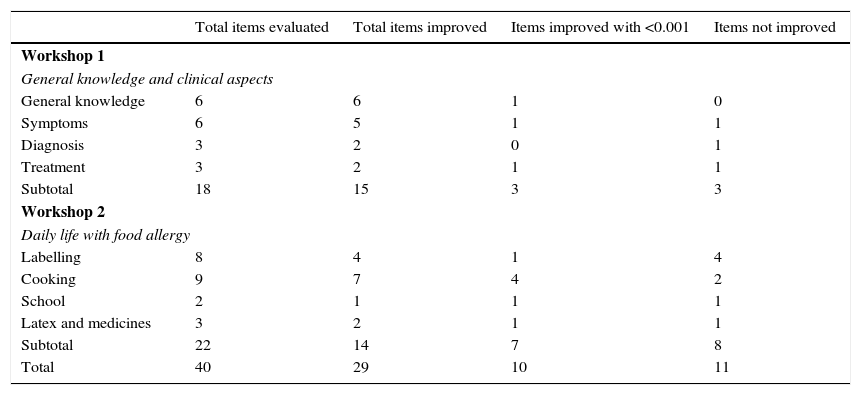
Evaluation of food allergy knowledge was carried out via an ad hoc questionnaire with 40 items. All of the items were explicitly addressed in the educational materials. For the first workshop there were 18 items related to general knowledge of food allergy (six items), symptoms (6), diagnosis (3), and treatment (3). In the second workshop there were 22 items related to the parents’ daily life, with questions about labelling (8), cooking (9), school (2), and latex and medicines (3).
The outcomes demonstrate a significant improvement in the parents’ knowledge (see Table 3). After evaluating knowledge acquisition following participation in the programme by the 174 participants who completed both the pre- and the post-programme questionnaires, a significant improvement in McNemar's Test was observed in 29 items out of 40 (72.5%) with ten items with <0.001 significance (25%). In the first workshop, parents improved in 15 out of 18 items (83.3%) with three items showing <0.001 significance (16.6%) and in the second workshop, there was improvement in 14 items out of 22 (63.6%) with seven items with <0.001 (31.8%).
Summary of results.
| Total items evaluated | Total items improved | Items improved with <0.001 | Items not improved | |
|---|---|---|---|---|
| Workshop 1 | ||||
| General knowledge and clinical aspects | ||||
| General knowledge | 6 | 6 | 1 | 0 |
| Symptoms | 6 | 5 | 1 | 1 |
| Diagnosis | 3 | 2 | 0 | 1 |
| Treatment | 3 | 2 | 1 | 1 |
| Subtotal | 18 | 15 | 3 | 3 |
| Workshop 2 | ||||
| Daily life with food allergy | ||||
| Labelling | 8 | 4 | 1 | 4 |
| Cooking | 9 | 7 | 4 | 2 |
| School | 2 | 1 | 1 | 1 |
| Latex and medicines | 3 | 2 | 1 | 1 |
| Subtotal | 22 | 14 | 7 | 8 |
| Total | 40 | 29 | 10 | 11 |
Parents did not improve their knowledge in three items (7.5%) related to general and clinical aspects of food allergy in Workshop 1 and in eight items (20%) about daily life with their children in Workshop 2. Labelling is the topic with the lowest learning increase in our outcomes. Parents improved in four items out of eight (50%).
To evaluate participant satisfaction with the programme, we asked three questions (regarding general improvement in knowledge, how to avoid allergic foods, and identifying symptoms) and one additional question aimed at evaluating overall satisfaction with the programme. The majority of parents and caregivers (87%) gave their improvement in general knowledge about food allergies a rating of seven or more points (mean of 8.32) on a scale from 1 to 10 (0 is considered “not satisfied,” and 10 is considered “very satisfied”). Regarding their knowledge of how to avoid allergenic foods, 81% of participants scored their knowledge with seven or more points (mean of 7.91), and on the topic of how to better recognise a child's symptoms, 84% of participants scored their knowledge with seven or more points (mean of 8.18).
Overall satisfaction with the educational programme (see Fig. 1) received an average rating of 9.03; in particular, 90% of participants rated the course between 8 and 10 points, and 41% gave it 10 points.
DiscussionThis article describes the development and evaluation of an educational programme designed to improve the competence of parents and caregivers of children with food allergies by offering health education workshops for parents and children. The patients, represented by their associations, participated with healthcare professionals and researchers in all phases of the project. This type of collaboration among all the parties involved, including healthcare professionals and patients, is a vital part of supporting a growing awareness of the social repercussions of food allergies.26 For us, this was one of the most important initial goals, that is, to create a real network between patients and professionals, working together to develop new ideas, with the common aim of improving quality of life for families with children living with food allergy.
The workshops were carried out in larger Spanish cities because these cities were also where patient associations are well-established; in addition, it was simpler to recruit patients and the professionals who taught the workshops in these cities.
The foods responsible for most of the allergies found in the present study correspond to those that are most prevalent among childhood food allergies in Spain,25 which indicates that our sample was representative of the general population. Milk (65%), eggs (62%), and nuts (40%) are the most common allergens related by our sample of patients. An educational intervention for teachers using a pre-test/post-test design was shown to significantly increase their knowledge about food allergy management.27 However, there has been little research on educational programmes for food allergies, possibly because of the great technical complexity of developing this type of programme. Improving the availability of clear and concise educational materials would likely reduce patient and family stress and anxiety, while at the same time improving their QoL.24
With respect to the sample, it is important to note that the majority of participants belonged to patient associations, and they initially indicated that they had enough information about food allergies (60% of parents). Our study can be seen as a new way to encourage additional research aimed at evaluating the impact of educational programmes on patients, especially on parents without previous healthcare information about food allergy. Vargas et al. observed that parents of children who had been recently diagnosed might have benefited the most from educational programmes.19
In the few educational programmes related to food allergies that have been evaluated,21 it has been observed that educating children and their families about the risks of their condition and improving their disease management skills (for example, by rejecting foods offered by other children, asking about foods at restaurants, and speaking with manufacturers) through educational activities can ease the burden of living with food allergies on children and their parents.21
Regarding our programme evaluation, the results obtained permit us to confirm that parents greatly improved their knowledge about all topics regarding food allergy. In our outcomes, we obtained an improvement in 29 items out of 40 (72.5%) with ten items with <0.001 significance (25%). This shows the great benefit derived from the educational programme.
Parents did not improve their knowledge about daily life with their children in eight items (36.3%) out of about 22; specifically, they did not learn the concepts in the labelling topic, where parents improved in four items out of eight (50%). Assuming that perhaps this part of the programme was not explained very well, parents may need more to put more effort into managing labelling. It is a very important aspect of their daily life. Further efforts are needed to improve knowledge regarding this point.
Parents in our workshops showed a great deal of interest in and asked many questions on topics related to their everyday life, such as labelling and the management of food allergy at school. It is important for them to know this, because allergists and other professionals normally do not have time, and may sometimes lack the necessary information, to explain all these issues to them.
Overall satisfaction with the programme was also positive on all scales. Participants considered the programme to be useful: 90% rated the course between eight and 10 points, and 41% rated it with 10 points. This is a very good result, which indicates the interest in such initiatives and encourages the team and other researchers to develop projects in order to empower patients and help them to improve their quality of life.
It can be said that these workshops addressed three types of challenges: preparing a programme and its materials, implementing it, and completing an evaluation of it. The materials that were created will remain available to the patient associations so that they can be used in the associations’ own educational activities. We also have an online educational platform with the same content; the outcomes of the parents of this study sample will be published soon.
With the knowledge obtained through this study, it is to be hoped that improved health education activities will be offered in the future.
Study limitationsIn future studies, an evaluation of children's learning could be carried out, even if the results are not highly reliable. However, QoL cannot be evaluated because of the absence of validated QoL questionnaires in Spanish.
Implications for clinical practice and further researchAccess to healthcare education, especially for those with chronic conditions, offers new ways for these diseases to be managed in the future. Empowering patients through programmes similar to ours offers them and their families benefits such as improved relationships with physicians, confidence, and autonomy. These programmes can also improve the healthcare system. Our educational project provides an example of the development of a health education programme for food allergies, as well as of a collaborative research project. In the context of education and research, educational materials for healthcare institutions, patient associations, and specialised healthcare professionals have been created. Our programme could thus provide worthwhile activities to counteract the lack of educational materials on this topic, while also offering instruments for evaluating the activities. In addition, our findings could be useful for the development of new materials and other educational initiatives in allergy units.Future studies must be developed, especially for parents with children who have been recently diagnosed.
Ethical disclosuresProtection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Patient data protectionThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all patients included in the study have received sufficient information and have given their informed consent in writing to participate in this study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of these documents.
FundingResearch has been funded by MEDA Pharma.
Conflict of interestsThis study was financed as an educational research project by the pharmaceutical company MEDA.
We thank the boards of directors of the patient associations and their volunteers, as well as the expert parents of patients, and the physicians who participated in the workshops.
The authors would like to acknowledge the parent members of patient associations and the professionals who voluntarily participated in the development of the workshops. Without their hard work and enthusiasm this research would not have been possible.