The association regarding the exposure to pets, especially cats and dogs, and the prevalence of allergic diseases is inconsistent.
ObjectiveWe analyzed the role played by early exposure to dogs or cats in the prevalence of allergic diseases amongst school-aged children.
MethodThrough a cross-sectional study, we examined 756 children, aged 6–7; these candidates were selected through cluster sampling. We inquired about the exposure that these children had had to dogs and cats, and whether these pets spent most of their time indoors or outdoors during the first year of the child's life. In order to identify the prevalence of allergic diseases and their symptoms, each child's parent completed the International Study of Asthma and Allergies in Childhood questionnaire.
ResultsExposure to outdoor dogs was associated to nocturnal coughing, odds ratio (OR) 0.64, with a confidence interval of 95% (95% CI) 0.43–0.95 and with atopic dermatitis (OR: 0.39; 95% CI: 0.20–0.76). Interestingly, exposure to outdoor cats was associated to nocturnal coughing (OR: 0.51; 95% CI: 0.32–0.83) and current rhinitis symptoms (OR: 0.59; 95% CI 0.36–0.97). After carrying out the multivariate analyses, only exposure to dogs, both indoor and outdoor, was significantly associated to a decrease in the prevalence of atopic dermatitis OR 0.40 (95% CI: 0.20–0.79) and OR 0.38 (95% CI: 0.18–0.83), respectively.
ConclusionOur findings suggest that exposure to dogs, whether they be indoor or outdoor pets, is associated to a decreased prevalence in atopic dermatitis.
On a global level, there is controversy regarding the role that interaction with dogs or cats plays in the development of allergic diseases. Through epidemiological studies have proven that pets are a risk factor when it comes to the development of asthma, allergic rhinitis and atopic dermatitis1,2; on the other hand, there is also evidence that has demonstrated that pets actually act as protective agents3–5; moreover, there are additional studies that have found pets to be irrelevant factors in the matter.6,7
There is also discrepancy concerning the type of pet that could be associated to the development of these allergic diseases, since there are places in the world where farm animals are considered children's pets,8 in some cases fish, birds and rodents act as childhood companions2,7; yet, only cats and dogs have been studied consistently. In Mexico, the role that cats and dogs play in the prevalence of allergic diseases has only been studied a handful of times.
In Mexico, the role that the exposure to dogs and cats plays in the development of the prevalence of allergic diseases has rarely been studied.2,8–11 In our country, the most common household pets are cats and dogs, notably the interaction with these pets can vary, as some Mexican families tend to allow their pets to live indoors. The study at hand aims to evaluate how early exposure to dogs or cats affects the prevalence of allergic diseases amongst school-aged children, and whether it makes a difference if these pets reside indoors or outdoors.
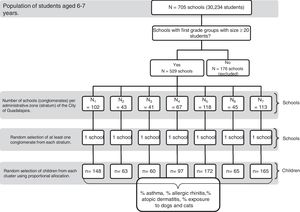
MethodsDesign and sample sizeFor this cross-sectional study, we included boys and girls, aged 6–7, all of whom attended primary schools in the city of Guadalajara, Mexico. The study universe consisted of 30,234 children from the 2013 to 2014 school year, distributed throughout 705 public and private schools.
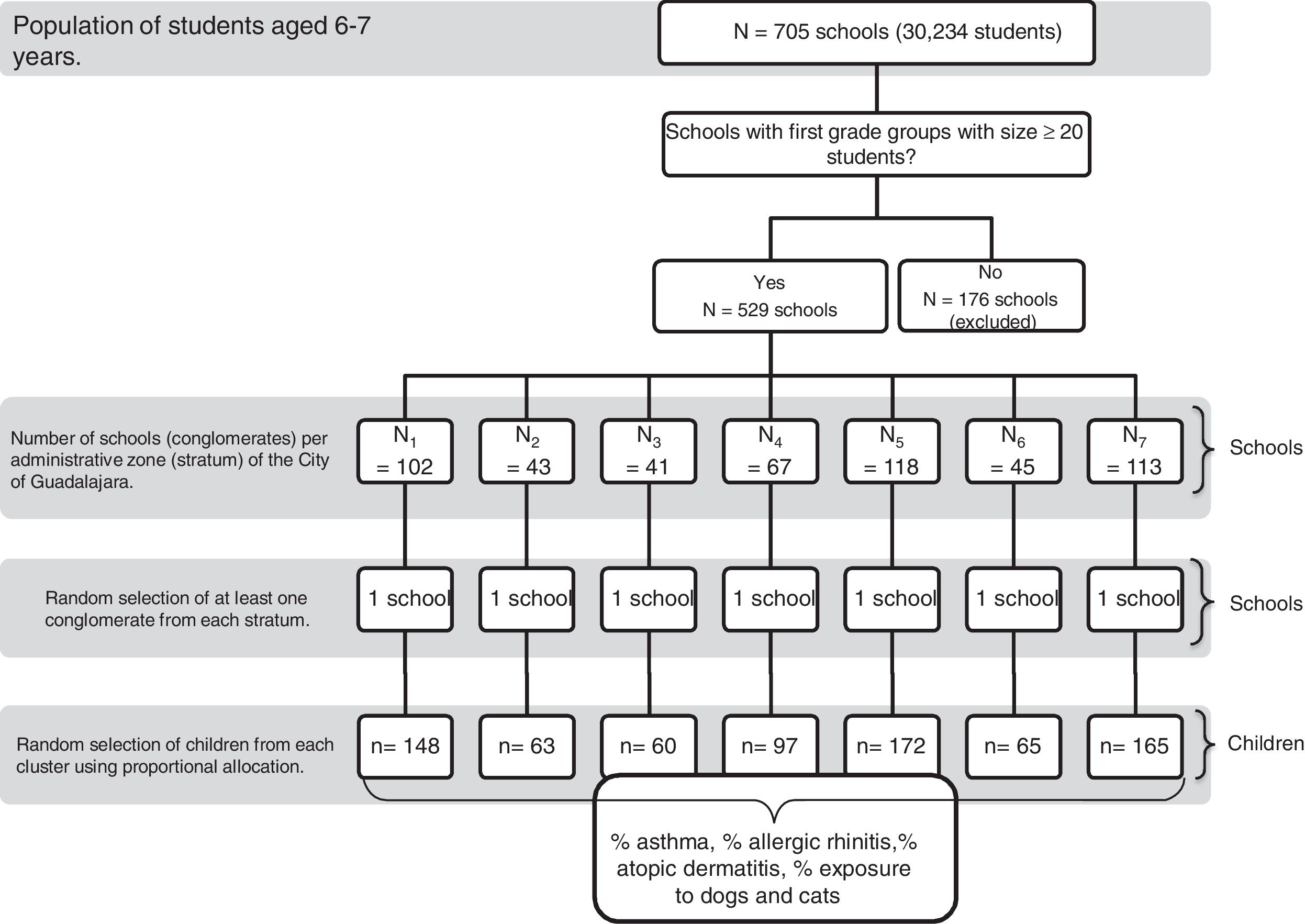
Sampling procedureFor a detailed description of the sampling procedure, read above.12 In brief, children were incorporated into our study through stratified conglomerated sampling, from April to December of 2014, Fig. 1. The city of Guadalajara is divided into seven administrative districts, each of these regions was contemplated as a stratum; through the proportional assignment technique we obtained a sub-sample from each area, we then multiplied the total sample size by the proportion of registered students in each district. Through random selection, we chose at least one school (conglomerate) within each district (stratum), and when it was necessary, we selected more schools in order to obtain the required sub-sample size.
QuestionnaireOur inquiry form was structured, and it included questions regarding each family's medical history of allergic diseases for both parents, as well as any previous medical diagnoses of atopic diseases for each child. In order to identify children with allergic diseases, we applied The International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire to parents of the children. We also asked whether or not each child had been exposed to dogs or cats during the first year of life, and whether this pet had been a predominantly indoor or outdoor pet.
EthicsThis study was approved by the Ethics and Research Committees at The Hospital Civil de Guadalajara Dr. Juan I. Menchaca; furthermore, this study received support from the Secretaría de Educación del Estado de Jalisco. Most importantly, each parent or guardian, along with his or her child, signed a written consent form in order to participate.
AnalysisThe prevalence of allergic diseases and their symptoms was estimated by dividing the number of subjects that answered each question affirmatively in The International Study of Asthma and Allergies in Childhood questionnaire, by the total number of subjects in the study group, additionally, we estimated confidence intervals for proportions. In order to identify a possible association between allergic diseases and the exposure to dogs and cats, we calculated the odds ratio (OR) and their respective Confidence Intervals to measure the magnitude of this association. We employed logistic binary regression to estimate the adjusted OR (ORa), in which the dependent variable was atopic dermatitis and the independent covariates were: exposure to dogs (indoor or outdoor), sex, family history of atopy, personal history of atopy, a cesarean birth, and breastfeeding. The values p≤0.05 served as a means to establish statistical significance. Analysis of the data was performed by using the IBM SPSS program, version 20.0 for Windows (Armonk, NY, USA).
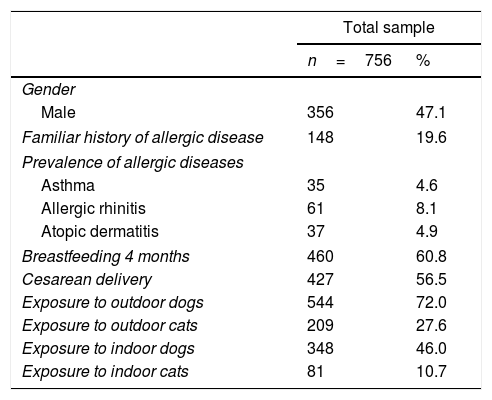
ResultsWe included 756 children in our study sample, of whom, 356 were male (47.1%), Table 1. The prevalence for asthma, allergic rhinitis and atopic dermatitis were: 4.6%, (95% CI: 3.3–6.4), 8.1% (95% CI: 6.3–10.2) and 4.9% (95% CI: 3.5–6.7), respectively. The frequency of previous maternal breastfeeding for at least four months was 61%, for cesarean section deliveries it was 56%. Children interacted with outdoor dogs and cats in 72% and 27.6% of the cases, they were exposed to indoor pets at a frequency of 46% and 10.7%, respectively.
Characteristics of study population.
| Total sample | ||
|---|---|---|
| n=756 | % | |
| Gender | ||
| Male | 356 | 47.1 |
| Familiar history of allergic disease | 148 | 19.6 |
| Prevalence of allergic diseases | ||
| Asthma | 35 | 4.6 |
| Allergic rhinitis | 61 | 8.1 |
| Atopic dermatitis | 37 | 4.9 |
| Breastfeeding 4 months | 460 | 60.8 |
| Cesarean delivery | 427 | 56.5 |
| Exposure to outdoor dogs | 544 | 72.0 |
| Exposure to outdoor cats | 209 | 27.6 |
| Exposure to indoor dogs | 348 | 46.0 |
| Exposure to indoor cats | 81 | 10.7 |
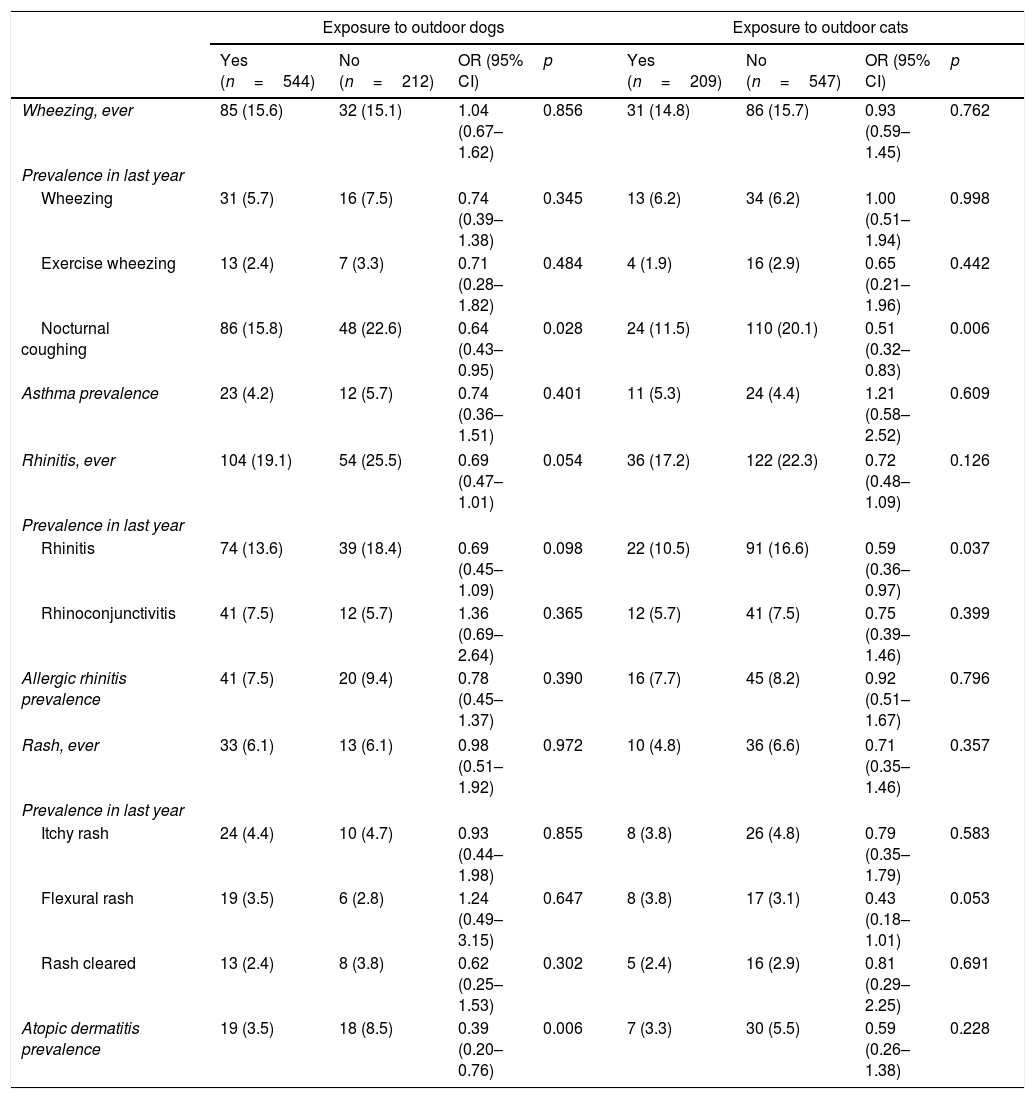
Children with exposure to outdoor dogs had a significantly decreased prevalence of nocturnal coughing that was unassociated to respiratory infection, one year prior to our study (OR=0.64; 95% CI: 0.43–0.95, p=0.028), Table 2. Similarly, this was the case regarding the prevalence of atopic dermatitis (OR=0.39; 95% CI: 0.20–0.76, p=0.006). Notably, contact with outdoor cats also presented a statistically significant negative association to nocturnal coughing and rhinitis, both during the year prior to our study, (OR=0.51; 95% CI: 0.32–0.83, p=0.006 and OR=0.59; 95% CI: 0.36–0.97, p=0.037, respectively).
Association between outdoor cats and dogs to the prevalence of allergic diseases and their symptoms.
| Exposure to outdoor dogs | Exposure to outdoor cats | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n=544) | No (n=212) | OR (95% CI) | p | Yes (n=209) | No (n=547) | OR (95% CI) | p | |
| Wheezing, ever | 85 (15.6) | 32 (15.1) | 1.04 (0.67–1.62) | 0.856 | 31 (14.8) | 86 (15.7) | 0.93 (0.59–1.45) | 0.762 |
| Prevalence in last year | ||||||||
| Wheezing | 31 (5.7) | 16 (7.5) | 0.74 (0.39–1.38) | 0.345 | 13 (6.2) | 34 (6.2) | 1.00 (0.51–1.94) | 0.998 |
| Exercise wheezing | 13 (2.4) | 7 (3.3) | 0.71 (0.28–1.82) | 0.484 | 4 (1.9) | 16 (2.9) | 0.65 (0.21–1.96) | 0.442 |
| Nocturnal coughing | 86 (15.8) | 48 (22.6) | 0.64 (0.43–0.95) | 0.028 | 24 (11.5) | 110 (20.1) | 0.51 (0.32–0.83) | 0.006 |
| Asthma prevalence | 23 (4.2) | 12 (5.7) | 0.74 (0.36–1.51) | 0.401 | 11 (5.3) | 24 (4.4) | 1.21 (0.58–2.52) | 0.609 |
| Rhinitis, ever | 104 (19.1) | 54 (25.5) | 0.69 (0.47–1.01) | 0.054 | 36 (17.2) | 122 (22.3) | 0.72 (0.48–1.09) | 0.126 |
| Prevalence in last year | ||||||||
| Rhinitis | 74 (13.6) | 39 (18.4) | 0.69 (0.45–1.09) | 0.098 | 22 (10.5) | 91 (16.6) | 0.59 (0.36–0.97) | 0.037 |
| Rhinoconjunctivitis | 41 (7.5) | 12 (5.7) | 1.36 (0.69–2.64) | 0.365 | 12 (5.7) | 41 (7.5) | 0.75 (0.39–1.46) | 0.399 |
| Allergic rhinitis prevalence | 41 (7.5) | 20 (9.4) | 0.78 (0.45–1.37) | 0.390 | 16 (7.7) | 45 (8.2) | 0.92 (0.51–1.67) | 0.796 |
| Rash, ever | 33 (6.1) | 13 (6.1) | 0.98 (0.51–1.92) | 0.972 | 10 (4.8) | 36 (6.6) | 0.71 (0.35–1.46) | 0.357 |
| Prevalence in last year | ||||||||
| Itchy rash | 24 (4.4) | 10 (4.7) | 0.93 (0.44–1.98) | 0.855 | 8 (3.8) | 26 (4.8) | 0.79 (0.35–1.79) | 0.583 |
| Flexural rash | 19 (3.5) | 6 (2.8) | 1.24 (0.49–3.15) | 0.647 | 8 (3.8) | 17 (3.1) | 0.43 (0.18–1.01) | 0.053 |
| Rash cleared | 13 (2.4) | 8 (3.8) | 0.62 (0.25–1.53) | 0.302 | 5 (2.4) | 16 (2.9) | 0.81 (0.29–2.25) | 0.691 |
| Atopic dermatitis prevalence | 19 (3.5) | 18 (8.5) | 0.39 (0.20–0.76) | 0.006 | 7 (3.3) | 30 (5.5) | 0.59 (0.26–1.38) | 0.228 |
Values in parentheses represent %.
OR: odds ratio; CI: confidence interval.
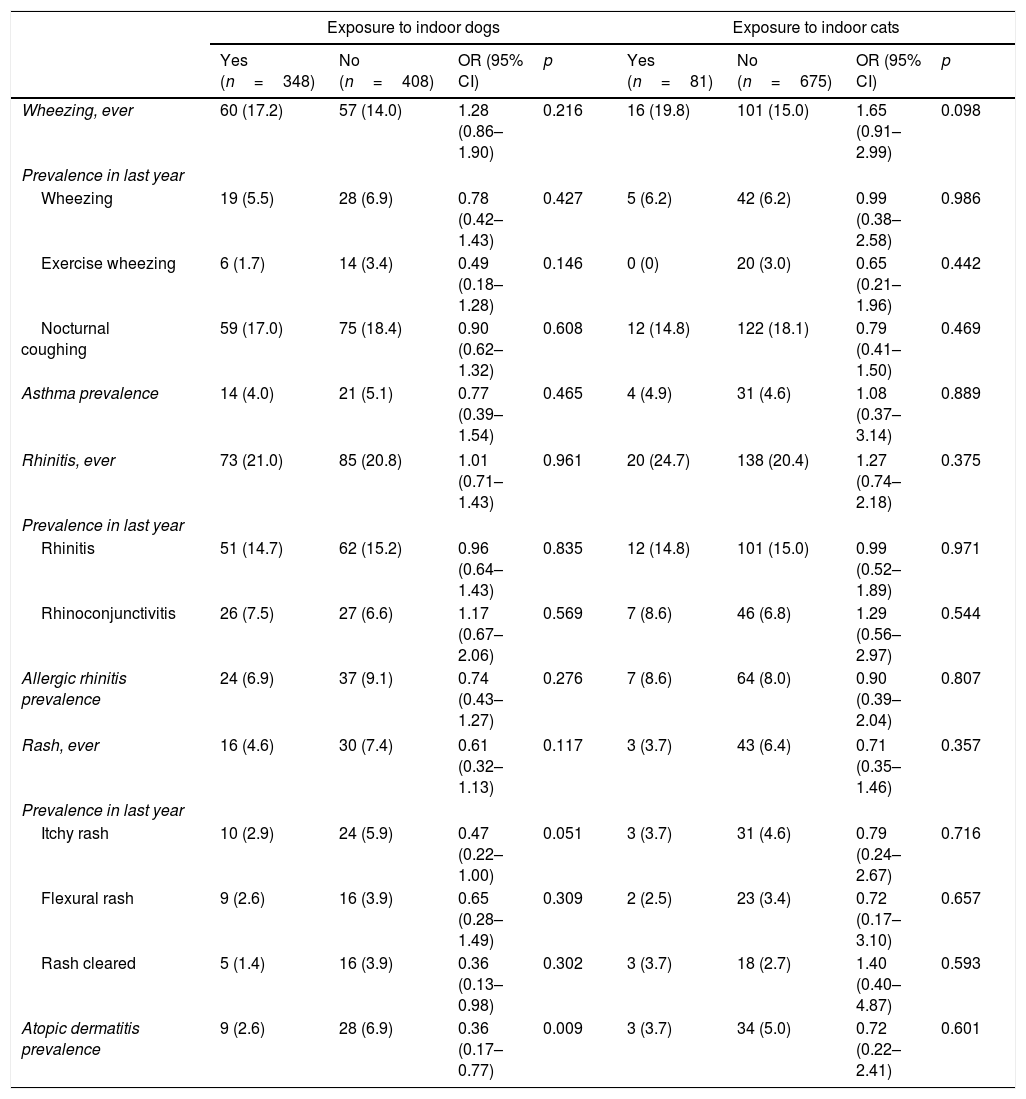
When we analyzed exposure to indoor pets, contact with dogs was also significantly associated to a decreased prevalence of atopic dermatitis (OR=0.36; 95% CI: 0.17–0.77, p=0.009), Table 3. However, there was no observed association of this occurrence with indoor cats.
Association between indoor cats and dogs to the prevalence of allergic diseases and their symptoms.
| Exposure to indoor dogs | Exposure to indoor cats | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n=348) | No (n=408) | OR (95% CI) | p | Yes (n=81) | No (n=675) | OR (95% CI) | p | |
| Wheezing, ever | 60 (17.2) | 57 (14.0) | 1.28 (0.86–1.90) | 0.216 | 16 (19.8) | 101 (15.0) | 1.65 (0.91–2.99) | 0.098 |
| Prevalence in last year | ||||||||
| Wheezing | 19 (5.5) | 28 (6.9) | 0.78 (0.42–1.43) | 0.427 | 5 (6.2) | 42 (6.2) | 0.99 (0.38–2.58) | 0.986 |
| Exercise wheezing | 6 (1.7) | 14 (3.4) | 0.49 (0.18–1.28) | 0.146 | 0 (0) | 20 (3.0) | 0.65 (0.21–1.96) | 0.442 |
| Nocturnal coughing | 59 (17.0) | 75 (18.4) | 0.90 (0.62–1.32) | 0.608 | 12 (14.8) | 122 (18.1) | 0.79 (0.41–1.50) | 0.469 |
| Asthma prevalence | 14 (4.0) | 21 (5.1) | 0.77 (0.39–1.54) | 0.465 | 4 (4.9) | 31 (4.6) | 1.08 (0.37–3.14) | 0.889 |
| Rhinitis, ever | 73 (21.0) | 85 (20.8) | 1.01 (0.71–1.43) | 0.961 | 20 (24.7) | 138 (20.4) | 1.27 (0.74–2.18) | 0.375 |
| Prevalence in last year | ||||||||
| Rhinitis | 51 (14.7) | 62 (15.2) | 0.96 (0.64–1.43) | 0.835 | 12 (14.8) | 101 (15.0) | 0.99 (0.52–1.89) | 0.971 |
| Rhinoconjunctivitis | 26 (7.5) | 27 (6.6) | 1.17 (0.67–2.06) | 0.569 | 7 (8.6) | 46 (6.8) | 1.29 (0.56–2.97) | 0.544 |
| Allergic rhinitis prevalence | 24 (6.9) | 37 (9.1) | 0.74 (0.43–1.27) | 0.276 | 7 (8.6) | 64 (8.0) | 0.90 (0.39–2.04) | 0.807 |
| Rash, ever | 16 (4.6) | 30 (7.4) | 0.61 (0.32–1.13) | 0.117 | 3 (3.7) | 43 (6.4) | 0.71 (0.35–1.46) | 0.357 |
| Prevalence in last year | ||||||||
| Itchy rash | 10 (2.9) | 24 (5.9) | 0.47 (0.22–1.00) | 0.051 | 3 (3.7) | 31 (4.6) | 0.79 (0.24–2.67) | 0.716 |
| Flexural rash | 9 (2.6) | 16 (3.9) | 0.65 (0.28–1.49) | 0.309 | 2 (2.5) | 23 (3.4) | 0.72 (0.17–3.10) | 0.657 |
| Rash cleared | 5 (1.4) | 16 (3.9) | 0.36 (0.13–0.98) | 0.302 | 3 (3.7) | 18 (2.7) | 1.40 (0.40–4.87) | 0.593 |
| Atopic dermatitis prevalence | 9 (2.6) | 28 (6.9) | 0.36 (0.17–0.77) | 0.009 | 3 (3.7) | 34 (5.0) | 0.72 (0.22–2.41) | 0.601 |
Values in parentheses represent %.
OR: odds ratio; CI: confidence interval.
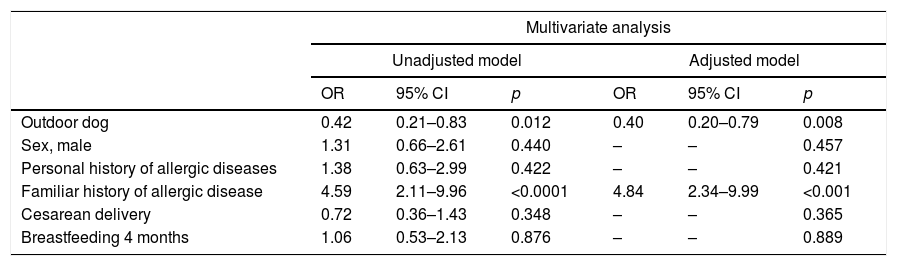
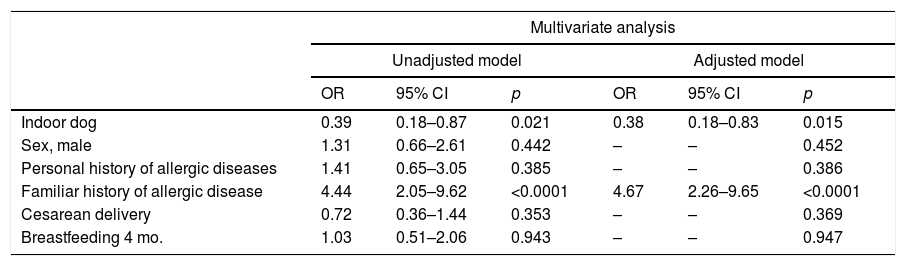
Multivariate analyses showed that atopic dermatitis was significantly linked to contact with outdoor dogs (ORa=0.40; 95% CI: 0.20–0.79, p=0.008) and to a personal history of atopy (ORa=4.84; 95% CI: 2.35–9.99, p<0.001), Table 4. This behavior was constant when atopic dermatitis was associated to contact with indoor dogs and a personal history of atopy (ORa= 0.38, p=0.015 and OR=4.67, p<0.0001), Table 5.
Association between exposure to an outdoor dog during the first year of life and the prevalence of atopic dermatitis.
| Multivariate analysis | ||||||
|---|---|---|---|---|---|---|
| Unadjusted model | Adjusted model | |||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Outdoor dog | 0.42 | 0.21–0.83 | 0.012 | 0.40 | 0.20–0.79 | 0.008 |
| Sex, male | 1.31 | 0.66–2.61 | 0.440 | – | – | 0.457 |
| Personal history of allergic diseases | 1.38 | 0.63–2.99 | 0.422 | – | – | 0.421 |
| Familiar history of allergic disease | 4.59 | 2.11–9.96 | <0.0001 | 4.84 | 2.34–9.99 | <0.001 |
| Cesarean delivery | 0.72 | 0.36–1.43 | 0.348 | – | – | 0.365 |
| Breastfeeding 4 months | 1.06 | 0.53–2.13 | 0.876 | – | – | 0.889 |
OR: odds ratio; CI: confidence interval;
OR obtained by logistic regression.
OR for variables that were used to adjust the model were not contemplated.
Association between exposure to an indoor dog during the first year of life and the prevalence of atopic dermatitis.
| Multivariate analysis | ||||||
|---|---|---|---|---|---|---|
| Unadjusted model | Adjusted model | |||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Indoor dog | 0.39 | 0.18–0.87 | 0.021 | 0.38 | 0.18–0.83 | 0.015 |
| Sex, male | 1.31 | 0.66–2.61 | 0.442 | – | – | 0.452 |
| Personal history of allergic diseases | 1.41 | 0.65–3.05 | 0.385 | – | – | 0.386 |
| Familiar history of allergic disease | 4.44 | 2.05–9.62 | <0.0001 | 4.67 | 2.26–9.65 | <0.0001 |
| Cesarean delivery | 0.72 | 0.36–1.44 | 0.353 | – | – | 0.369 |
| Breastfeeding 4 mo. | 1.03 | 0.51–2.06 | 0.943 | – | – | 0.947 |
OR: odds ratio; CI: confidence interval.
OR obtained by logistic regression.
OR for variables that were used to adjust the model were not contemplated.
This study shows that exposure to dogs, but not cats, during the first year of life is associated with a decreased prevalence of atopic dermatitis in children aged 6–7, this was more notable when the dog remained indoors. It also demonstrates that a family history of atopy is a factor that is significantly associated to the prevalence of atopic dermatitis. To our knowledge, thus far, no other studies have evaluated whether the child interacts with indoor or outdoor pets and how this affects allergic diseases.
The attempt to quantify the association between pets and allergic diseases has produced contradictory findings, furthermore, there is no consistency regarding the types of pets that might be associated to such diseases. For example, one study carried out in Iran, factored in farm animals such as cows, pigs, goats and sheep as pets: in their study the children presented a reduced frequency of wheezing fits, coughing, sneezing, rhinorrhea or nasal obstruction and epidermal itchiness during the year prior to their study,8 and while those animals lived with the children.
In our country, given the structural characteristics of our homes, the majority of cats and dogs, tend to live outdoors, that is to say, they live in open garages, patios or roof tops, yet, they can also reside indoors, sometimes they even sleep inside their owners’ bedrooms. Thus, the level of exposure to pets is a variable factor, such variances can directly influence the development of allergic diseases.
In regard to asthma, a recent study showed that exposure to dogs or pets (cattle or sheep), during the first year of life, was associated to a reduced rate of asthma incidences in pre-school to school-aged children.4 After analyzing the data obtained in exclusively European cohort studies (11 studies), there was no documented association between exposure to dogs or cats and asthma amongst school-aged children.7 In China, a study that included more than 13 thousand children, aged 4–6, demonstrated that interaction with pets acted as a risk factor for asthma prevalence.2 In our study, exposure to dogs and cats was associated to a reduced frequency in coughing, during the 12 months prior to our study, however, this was only the case when pets remained outside the home, nevertheless, this effect disappeared when the interaction with dogs or cats was indoor. The rest of the asthma symptoms, or those previously associated to asthma, were no longer documented as a factor.
When it comes to allergic rhinitis, and its symptoms, our analysis of exposure to outdoor cats showed that these pets acted as protective agents against the presence of rhinitis during the year prior to our study; however, this agent disappeared when the family cat lived indoors. Phase III of the ISAAC study, which included data from various international research centers, provided contradicting results when it came to the association between dogs or cats and the symptoms of allergic diseases; this was the case for children aged 6–7 and adolescents, allergic rhinitis and allergic rhino-conjunctivitis appeared to be more prevalent as a result of exposure to cats during the first year of life; however, dogs did not have this effect on the adolescent group.1 In Latin America, the rhino-conjunctivitis symptoms amongst Bolivian schoolchildren, did not increase in relation to their exposure to dogs or cats, but it did rise with exposure to farm animals.6 On the other hand, Chinese children that were exposed to dogs during birth were at greater risk of being diagnosed with allergic rhinitis, when compared to children that were not exposed to dogs during birth.2 Recently, an independent cohort study observed that indoor exposure to dogs was strongly associated to a decreased risk of developing atopic dermatitis at the age of three, notably, this decrease was dose-dependent.5 In a meta-analysis that only included cohort studies, a 25% decreased risk of atopic dermatitis was observed in children that were exposed to dogs; contrastingly, cats offered no observable protection.3 In our study, which is not a cohort study, the findings were similar to those in the meta-analysis. We observed a 60% decrease in the prevalence of atopic dermatitis when children maintained contact with a dog during the first year of their lives, regardless of whether the dog lived indoors or outdoors.
In households where fish are favored as indoor pets, these appear to act as a risk factor for asthma, allergic rhinitis or allergic dermatitis symptoms; however, these symptoms varied based on the stage of life during which the child was exposed to fish.2 Birds or rodents are other pets that families choose to adopt; interestingly, according to the meta-analysis, exposure to these animals appear to neither increase nor decrease the risk of developing asthma or allergic rhinitis amongst schoolchildren.7 Our study did not encompass exposure to pets such as fish, birds or rodents and their possible association to allergic diseases, thus, we are unaware of how these animals might affect our population.
Various explanations have been proposed when exposure to dogs or cats has acted as a protective agent against the development of allergic diseases; of these explanations, the hygiene hypothesis is one of the most well-known, it is said that fewer family members, better domestic services, and hygiene, have decreased the number of contagions, consequently, the expression of atopic diseases has increased13; nevertheless, this hypothesis seems to leave out the exposure to animals that have fur, which is why this would not be the most comprehensive justification when it comes to the roles that pets might play in the prevalence of allergic diseases. Furthermore, it has been observed that children who live in rural areas or farms, have a lower chance of manifesting allergic diseases, when compared to children that live in an urban setting.14–17 In our country, it appears that living in a rural area or being exposed to farm animals does not offer any allergic protection.18 When researchers have attempted to explain a rural environment as a protective mechanism, endotoxins are usually credited for this phenomenon. In fact, there is evidence that has proven that exposure to endotoxin reduces the risk of atopic dermatitis.19 Interestingly, the presence of dogs, but not cats, has been associated to an increased variety of microbiome bacteria where these animals live20; however, researchers have also detected a higher amount of endotoxin bacteria in household dust;21 thus, early exposure to dogs might influence the child's immune response, and consequently, reduce the frequency of atopic diseases.
An area that has seldom been explored concerns the role that the attachment theory plays in the development of allergic diseases. According to Bowlby, attachment is a child's willingness to seek proximity and contact with an individual22; from this perspective, children are likely to form attachments to their pets, especially to a dog, and when this companionship is established during the first years of life; thus, the coexistence with a pet would allow a child to obtain psychological and social benefits.23 Similarly, an overall sensation of wellbeing might be attained by having a pet, this could stimulate the production of oxytocin, a neuropeptide that has been associated to social behavior in human beings.24 Recently, it has been proven that oxytocin is not only produced in the pituitary gland, but that it can also be produced and released through keratinocyte and fibroblasts in the skin; which is why the lack of expression from the oxytocin receptor, on the keratinocyte surface, has been linked to the release of IL-6, CCL5 and CXCL10; all of these cytokines have pro-inflammatory activity.25 Thus, close contact with dogs, especially during the early stages of life, regulates an immunological response in the skin through oxytocin, resulting in a reduced prevalence of atopic dermatitis.
One of the factors that has been consistently associated to allergic diseases regards the genetic predisposition of an individual.9,26–28 In our study, a family history of atopy was notably associated to the prevalence of atopic dermatitis. Notably, in our population, factors such as breastfeeding or a cesarean delivery, do not seem to be associated to allergic diseases.27,29
In our study there were additional limitations to those that are inherent to cross sectional studies. It is necessary to make note of the fact that we did not analyze the number of dogs in each household; as previously noted, when there are more dogs, there is a reduced likelihood of atopic dermatitis. As far as each family's dogs, we are unaware of what their characteristics were; it is likely that a dog's size, fur, or sex could influence the development of allergic diseases. Furthermore, we did not inquire about the amount of time that each child might have spent directly with their dogs or cats, or whether this contact had been established during gestation, nor did we ask if they had maintained contact with a pet until the time of our investigation. Likewise, we did not ask about exposure to farm animals, as we assumed that children in an urban setting are unlikely to be in contact with them. Conversely, one of this study's strengths lies in the fact that we did give importance to where these pets spent most of their time; the latter is a relevant matter when studying how pets can affect the development of allergic diseases. An additional strength in our study regards the sampling procedure, which allowed us to incorporate children from all socioeconomic strata, different school schedules and every geographic area within the city of Guadalajara.
ConclusionsIn conclusion, this study proves that exposure to dogs during the first year of life, whether they are indoor or outdoor pets, is associated to a reduced prevalence of atopic dermatitis in schoolchildren.
To date, there is no uniformity in the results that have been obtained from the various approaches to the research projects that have evaluated the association between pets and allergic diseases. Moreover, there is no regularity when it comes to the types of pets that might be acting as protective agents against these diseases.
Lastly, it is important to note that a personal history of the allergic disease favored its manifestation.
FundingNone.
Conflict of interestThe authors have no conflict of interest to declare.
As authors of this study, we wish to express our gratitude to the parents and children that kindly chose to partake in our Project; as well as the teachers at all participating schools.
We would also like to thank Pharmacist Sandra Vega Villamar for her help with the design of the flowchart.