INTRODUCTION
Recent advances in the understanding of the urticaria and chronic angioedema pathogenesis suggest that there may be an underlying autoimmune condition in many cases.
Since Leznoff et al (1) reported the association of chronic urticaria and angioedema with thyroid autoimmunity for the first time in 1983, several publications (2, 3) have verified this association. Thus, there is growing evidence that some cases of chronic urticaria and angioedema are associated with thyroid autoimmunity and that a subset of these patients can respond rapidly to thyroid hormone administration (6).
We present the case of a patient with unilateral facial edema associated to positive thyroid antibodies.
CASE REPORT
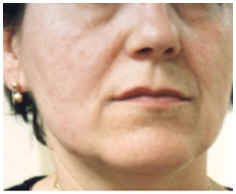
The case of a 42-year of patient with no significant family background, in whom arterial hypertension which is under treatment with bisoprolol stands out among her personal background, is presented. Two months prior to consulting her physician, she began with swelling in the right hemiface as well as mild swelling in the right half of the upper lip, that persisted when she came to the consultation (fig. 1).
Figure 1.
No other skin or respiratory symptoms were reported. She had no facial paralysis or glossitis migrans and there was no goiter.
ALLERGOLOGIC STUDY
Some skin tests were performed with a standard series of pneumoallergens (ALK-Abello®) and with a series of foods (Bial-Aristegui®) that were negative. Epicutaneous tests were performed with a standard series of contact allergens (True Test-ALK-Abello®) that were negative.
Laboratory analyses were performed and included a complete blood count, ESR, biochemistry study, proteinogram, coagulation study, complement, rheumatoid factor, anti-nuclear antibodies, hydatidosis and hepatitis serologies, urine sediment and stool parasitology, which were within the normality limits. A chest X-ray, that was normal, was also performed. The TSH value was normal. The thyroglobulin antibodies were positive: 492 IU/ml (ELISA) (reference values for our laboratory < 150), the microsomal antibodies being negative. The patient refused to undergo a biopsy in the skin zone involved.
The facial edema did not respond to treatment with cetirizine and as an edema related with thyroid autoimmunity was suspected, treatment was initiated with 100 mcg/day of thyroxin that was maintained for 2 months.
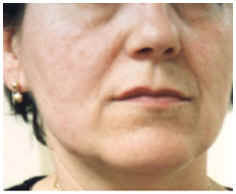
After initiating this treatment with thyroxin, the facial edema began to decrease until it had almost disappeared when the treatment was completed (fig. 2).
Figure 2.
At one month of initiating treatment, a mild decrease occurred in the thyroglobulin antibody values up to 394 IU/ml, and the TSH, T3 and free T4 remained within the normal limits. At the end of the 2-month treatment cycle, the thyroglobulin antibody values increased to 683 IU/ml, while the TSH decreased to 0.14 m IU/ml (reference values for our laboratory, 0.25-5), and the T3 and T4 values remained normal. One month after completing treatment, the antibody value remained at 635 IU/ml, while the TSH was within the normal limits (1.55 m IU/ml) again. The patient continued to be clinically well, without any recurrence of the facial edema.
Three months after discontinuing the thyroxin, the patient presented a new facial edema having the same characteristics as previously, although less intense. This coincided with an increase in the thyroglobulin antibody values up to 1,063 IU/ml, and the TSH, T3 and T4 remained within the normal limits. A decision was made to reinitiate treatment with thyroxin at a dose of 100 mcg/day, which led to a new remission of the facial edema.
DISCUSSION
In 1983, Leznoff et al (1) made the first report on the association of chronic urticaria and angioedema with the presence of thyroid antibodies, which were positive in 17 patients out of a total of 140 consecutive patients with chronic urticaria and angiodema.
After Leznoff and Sussman (3) published a series of 624 patients with chronic urticaria and angioedema, 90 of whom showed evidence of thyroid autoimmunity. Of these 90 patients, 3 presented isolated angioedema without associated urticaria. A total of 46 patients were treated with thyroxin, 8 of whom presented remission of the disease in 4 weeks.
In the Turktas et al (6) study, 11 out of 94 patients with chronic urticaria and angioedema had positive thyroglobulin antibodies and 9 had positive microsomal antibodies, with significant differences in regards to the healthy controls.
Granier et al (2) reported one case of chronic urticaria associated with Hashimoto's thyroiditis with a significant increase in microsomal antibodies. The biopsy of the skin lesions showed leukocytoclastic vasculitis changes.
Peltz et al (7) reported the case of a 56-year old woman with recurrent episodes of angioedema of the tongue associated with pernicious anemia and with positive thyroid antibodies, increase in TSH and decrease in the free thyroxin index, who was diagnosed of Hashimoto's thyroiditis. The angioedema episodes disappeared after initiating treatment with thyroxin.
According to Rumbyrt et al (8), 7 patients with chronic urticaria and positive thyroid antibodies, whose thyroid hormone values were normal, responded to treatment with thyroxin with the disappearance of their urticaria. After a minimum of 4 weeks of treatment, the thyroxin was discontinued, after which two patients remained in remission and the other 5 presented recurrence of the disease. The latter group responded again when treatment was re-initiated with thyroxin.
In 1996, Dreyfus et al (9) reported the case of a 9-year old boy with severe chronic urticaria which was resistant to treatment with antihistamines and steroids and in whom slightly increased levels of thyroid microsomal antibodies, with normal thyroid hormones, were detected. The patient presented total remission of his symptoms at 4 weeks of treatment with thyroxin.
We present the case of a female patient with chronic unilateral facial edema associated to the presence of positive thyroglobulin antibodies, whose thyroid function was normal, and who responded to 2-months of treatment with thyroxin with the disappearance of her facial edema. She remained in remission up to 3 months after having discontinued treatment, at which time the edema reappeared. This responded again to treatment with thyroxin. In spite of we couldn't make a skin biopsy, we think it's not a Melkersson-Rosenthal syndrome because the lack of facial paralysis or glossitis migrans and the response to tiroxin treatment.
The mechanisms by which thyroid autoimmunity and chronic urticaria and angioedema are associated are scarcely known. It has been published that the skin lesions in cases of chronic urticaria and angioedema are characterized by the appearance of activated CD4 + T lymphocytes, monocytes, neutrophils and eosinophils. These inflammatory cells stimulate the mastocytes through the release of histamine releasing factors, granulocyte-macrophage colony stimulating factor, interleukin 1 and interleukin 3 (6). The thyroidal effects of many cytokins can explain the association of thyroid autoimmunity and chronic urticaria and angioedema. The interleukins 1 and 6 can worsen the thyroid cellular function, interferon-g together with the tumor necrosis factor are cytostatics for the rat thyroid cell lines, and isolated interferon-g decreases the T3 and thyroglobulin release by the thyroid cells in response to TSH (10).
On the other hand, the mechanism by which the thyroid hormone improves urticaria and angioedema in patients with thyroid autoimmunity is presently an enigma.
It should be stressed that there was no correlation between the clinical response of the patient to the treatment with thyroxin and the level of thyroglobulin antibodies in our case, there being an initial decrease and then a later increase to levels greater than the initial ones. This finding is consistent with that reported by Rumbyrt et al (9), since 2 out of the 4 patients in whom the thyroglobulin antibody levels were repeated showed an increase in spite of their clinical improvement.