Anaphylaxis is a “severe, life-threatening, generalised or systemic hypersensitivity reaction” as reported by the systematic review on its epidemiology in Europe.1 The diagnostic criteria are well defined and generally accepted.2 In general, anaphylaxis incidence ranges from 1.5 to 7.9 per 100,000 person-years, so 0.3% of the population may experience anaphylaxis in their lives. Food, drugs, stinging insects, and latex are the most common triggers. The updated World Allergy Organization Guidelines focus on its diagnosis and management.3 Infants and teenagers have increased vulnerability to anaphylaxis; comorbidity with severe or uncontrolled asthma, mastocytosis, and concurrent use of some medications increase the risk of severe or fatal anaphylaxis. Food is the most important trigger in childhood.4 Food anaphylaxis typically occurs after ingestion, more rarely after skin contact or inhalation. Clinical diagnosis is based on consideration of presenting signs and symptoms and on excluding other sudden-onset multisystemic diseases. Clinical history and serum allergen-specific IgE and/or skin prick test remain the cornerstone for diagnosing food allergy. In this regard, attempts have been made in order to define a level of IgE that might be a predictor of food allergy, as oral challenge must be avoided in patients with anaphylaxis.5 Recently, molecular-based allergy diagnostics, based on assessment of molecular components (recombinant or purified) of single allergens, improved the work-up, as it allows defining the profile of allergenic proteins involved in sensitisation and is useful to stratify the potential risk of inducing a severe allergic reaction.6 Fortunately, only few kinds of food, mainly including egg, milk, peanut, fish, soybean and wheat are usually the cause of anaphylaxis in children and adolescents. Their relevance depends on the age of patients and, of course, on dietetic habits, which are different in each country. In this regard, there are some studies that addressed this topic, also considering the different anaphylaxis symptoms.7–10
For these reasons, we report the clinical data of children and adolescents visited at Allergic Disease Center of the Istituto Giannina Gaslini (the most important paediatric hospital in Northern Italy) for anaphylaxis during the previous year, with the aim of: (i) defining clinical factors that might have an influence on the development of the disease; and (ii) describing the most relevant foods causing anaphylaxis.
Diagnosis of food anaphylaxis was based on validated criteria,1–3 such as: (i) suggestive clinical history, (ii) allergen-specific IgE detection for suspected food, and (iii) symptoms consistent with sensitisation, i.e. the demonstration of a cause/effect dependence between ingestion of sensitising food allergen and occurrence of anaphylaxis clinical features (post hoc ergo propter hoc). Cardiovascular features were: hypotension, impairment of conscious state, pale and floppy presentation; respiratory features were: breathlessness, tongue or throat swelling, throat tightness, stridor, talking difficulty, wheezing, cough, and tachypnoea; gastrointestinal features were: vomiting, colic, and diarrhoea; skin features were: angio-oedema, urticaria, itching, and erythema.
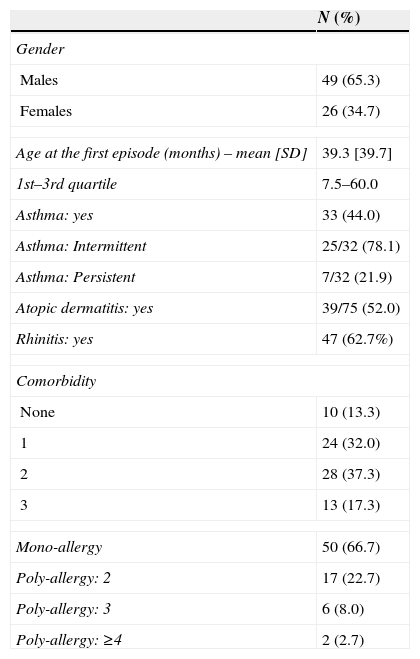
Globally, 75 patients were visited for anaphylaxis. Males (49, 65.3%) were more than females (Table 1). The mean age at the first episode of anaphylaxis was 39.3 months (interquartile range 7–5 – 60 months). Comorbidity with allergic disorders, including allergic rhinitis, atopic dermatitis, and asthma was detectable in most patients: 86.7%; 37.3% had two comorbidities and 17.3% had three. Mono-allergy was diagnosed in about 2/3 of patients. On the contrary, poly-allergy to more foods was present in 1/3 of the patients. About 30% of the patients experienced two or more episodes of anaphylaxis.
Demographic and clinical characteristics.
| N (%) | |
|---|---|
| Gender | |
| Males | 49 (65.3) |
| Females | 26 (34.7) |
| Age at the first episode (months) – mean [SD] | 39.3 [39.7] |
| 1st–3rd quartile | 7.5–60.0 |
| Asthma: yes | 33 (44.0) |
| Asthma: Intermittent | 25/32 (78.1) |
| Asthma: Persistent | 7/32 (21.9) |
| Atopic dermatitis: yes | 39/75 (52.0) |
| Rhinitis: yes | 47 (62.7%) |
| Comorbidity | |
| None | 10 (13.3) |
| 1 | 24 (32.0) |
| 2 | 28 (37.3) |
| 3 | 13 (17.3) |
| Mono-allergy | 50 (66.7) |
| Poly-allergy: 2 | 17 (22.7) |
| Poly-allergy: 3 | 6 (8.0) |
| Poly-allergy: ≥4 | 2 (2.7) |
About clinical features, skin symptoms dominated (94%), followed by respiratory complaints (82%), gastrointestinal features (49%), and cardiovascular symptoms (9%).
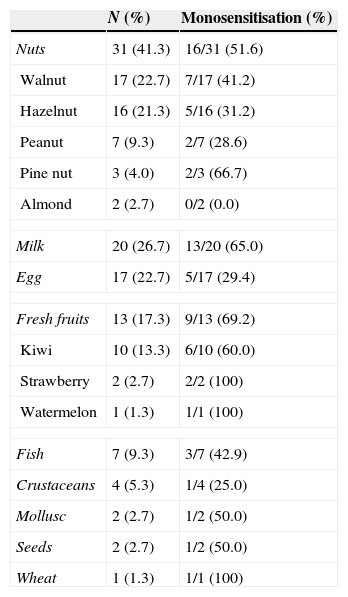
Regarding trigger foods (Table 2), nuts family was the most relevant food cause of anaphylaxis, as 31 patients (41.3%) were allergic to nuts, 16 of them (51.6%) were mono-allergic. In particular, walnut allergy was the most prevalent with 17 cases (seven (41.2%) were mono-allergic). Hazelnut allergy was the second cause of nut allergy: 16 patients, five of them (31.2%) were mono-allergic. Peanut allergy was diagnosed in seven patients (9.3%), two were mono-allergic (20%). Three patients were allergic to pine-nut, and two to almond.
Trigger foods for anaphylaxis.
| N (%) | Monosensitisation (%) | |
|---|---|---|
| Nuts | 31 (41.3) | 16/31 (51.6) |
| Walnut | 17 (22.7) | 7/17 (41.2) |
| Hazelnut | 16 (21.3) | 5/16 (31.2) |
| Peanut | 7 (9.3) | 2/7 (28.6) |
| Pine nut | 3 (4.0) | 2/3 (66.7) |
| Almond | 2 (2.7) | 0/2 (0.0) |
| Milk | 20 (26.7) | 13/20 (65.0) |
| Egg | 17 (22.7) | 5/17 (29.4) |
| Fresh fruits | 13 (17.3) | 9/13 (69.2) |
| Kiwi | 10 (13.3) | 6/10 (60.0) |
| Strawberry | 2 (2.7) | 2/2 (100) |
| Watermelon | 1 (1.3) | 1/1 (100) |
| Fish | 7 (9.3) | 3/7 (42.9) |
| Crustaceans | 4 (5.3) | 1/4 (25.0) |
| Mollusc | 2 (2.7) | 1/2 (50.0) |
| Seeds | 2 (2.7) | 1/2 (50.0) |
| Wheat | 1 (1.3) | 1/1 (100) |
Milk allergy was diagnosed in 20 patients (26.7%), and 13 children (65%) were mono-allergic to cow milk.
Egg allergy was diagnosed in 17 patients (22.7%), but only five egg-allergic children (29.4%) were mono-allergic.
Fresh fruits caused anaphylaxis in 13 patients (17.3%), and the most important fruit was kiwi as 10 patients (13.3%) were allergic to this fruit and six (60%) were mono-allergic.
Fish allergy was present in seven patients and crustacean allergy in four.
About age at the anaphylaxis onset, milk allergy usually starts within the first year, immediately followed by egg anaphylaxis. Nut allergy and fresh fruit allergy begin around 3–4 years. Then, fish and crustacean allergy occur.
Our findings are substantially consistent with a French survey that reported a prevalence of milk allergy ranging between 30 and 15%, egg allergy 25–5%, fruit allergy between 10 and 25%, and seafood allergy between 17 and 14% in children and adolescents (7). A five-year retrospective review of paediatric anaphylaxis, conducted in Australia, demonstrated that peanut allergy (18%) was the most prevalent, followed by cashew allergy (13%), milk allergy (11%), egg allergy (9%), fruit (5%), and seafood (4%); noteworthy, 28% of the children had poly-allergy.8 Data from the paediatric anaphylaxis registry of German-speaking countries demonstrated in 115 cases that peanut allergy was the most frequent (26 patients) cause of anaphylaxis, followed by: hazelnut (11 subjects), milk (11 subjects), egg (8 patients), cashew (5 cases); the other foods had a prevalence <5% (9).
A recent survey conducted in Piemonte region, which is close to Liguria region, reported some data consistent with the present study: nuts allergy affected 31.6% of the paediatric population with anaphylaxis; milk allergy was the cause of anaphylaxis in 14.4% of the cases; and egg allergy in 15.4% (10). On the contrary, conflicting findings concerned fresh fruit allergy: only 10.4% suffered from this type of food allergy (it is remarkable that no subject had kiwi allergy), 7.7% had fish allergy, and only 2.3% crustacean allergy. This discrepancy, partially few explainable as Piemonte and Liguria are border regions, could be attributable to different diet habits; for example, walnut sauce and pesto sauce (including as ingredient pine nut) are very popular in Liguria. Another possible explanation might be that the present study was performed in a third level centre, whereas the Piemonte survey collected data also from peripheral centres (less equipped, such as with less available resources both concerning qualified and trained specialists and adequate lab).
Anyway, the most important outcome of the present study is that the anaphylaxis in paediatric age has peculiar characteristics: frequent comorbidity and poly-allergy. The presence of comorbidity underlined the concept that anaphylaxis often occurs when co-factors are expressed; in the present report, associated atopic disorders are very common. On the other hand, poly-allergy is frequent: about 1/3 of the children were allergic to more foods. This outcome may have a relevant clinical consequence: a considerable number of patients experienced more anaphylaxis episodes.
These aspects underline the concept that paediatric anaphylaxis is a complex and complicated disorder that should be carefully investigated and managed and deserves adequate attention as requires specific and in-depth competence.
The main limitation of the present experience is that it was based on a selected cohort of patients and there is no information on follow-up as it is at present ongoing. Moreover, further studies addressing the molecular profile of food allergens causing anaphylaxis are also ongoing. In addition, it is important to consider whether these findings may be unique to these paediatric patients with food-induced anaphylaxis or this is the overall trend of paediatric food allergy. In this regard, a study investigating this issue is ongoing.
In conclusion, the present study shows that paediatric anaphylaxis has peculiar characteristics, including comorbidity and poly-allergy, nuts and also kiwi are relevant causal food allergens, and a thorough work-up is mandatory.
Ethical disclosuresProtection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Patients’ data protectionConfidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
FundingPartially funded by Ricerca Corrente – Italian Ministry of Health.
Conflict of interestAll authors declare that have no conflict of interest concerning the present study.