The objective was to estimate the incidence of asthma in young adults from 13–15 years old to 23–25 years old, and associated factors.
MethodsIn 2012, a population-based prospective cohort study was carried out in Castellon from the cohort who had participated in the International Study of Asthma and Allergy in Childhood in 1994 and 2002. A telephone survey was undertaken using the same questionnaires. A new case of asthma was defined as a participant free of the disease in 2002 who suffered asthma, was diagnosed with asthma, or took medications against asthma based on self-report from 2002 to 2012.
ResultsThe mean age of participants was 24.9±0.6 with a follow-up of 79.1%. Asthma cumulative incidence was 3.4%: 44 new cases occurred among 1280 participants. The incidence was higher in females than males with relative risk (RR)=2.02 (95% confidence interval [CI] 1.1–3.8). A significant decrease of asthma incidence density was observed (8.2 cases to 3.5 cases per 1000 person/year). Factors associated with the incidence of asthma were allergic rhinitis (RR=4.05; 95% CI 1.7–9.6), bronchitis (RR=2.13; 95% CI 1.0–4.5), mother's age at time of birth (RR=0.87; 95% CI 0.8–0.9) and a pet other than a dog or cat (RR=0.42; 95% CI 0.2–0.9). For gender, some variations in the risk factors were observed.
ConclusionsA significant decrease in the incidence of asthma was observed. Several risk and protective factors were found.
Asthma is the most common respiratory disease of the lower respiratory tract in children worldwide, and is becoming one of the most prevalent chronic diseases and causes of morbidity today. According to data obtained in the International Study of Asthma and Allergy in Childhood (ISAAC) phase III worldwide,1 in schoolchildren the asthma prevalence stands at 11.7%, increasing to 14.1% in the case of teenagers. In Castellon, the latest data on prevalence stands at 9% for adolescents.2
Few published studies have evaluated the trend in asthma incidence among the same population from school age to adulthood. A study based on the European Community Respiratory Health Study (ECRHS) estimated a cumulative incidence of 3.9% among adults aged 20–44 years.3 In Castellon, the incidence among adolescents (13–15 years old) was 6.4% (108 new cases) between 1994 and 2002.4
In this context, the objective of the present study was to follow up the cohort of schoolchildren in Castellon from 2002 (13–15 years old) to 2012 (23–25 years old) in order to estimate the incidence of asthma and its risk factors, and to compare it with the period 1994–2002.
Patients and methodsA population-based prospective cohort study was carried out on the cohort of schoolchildren who had participated in the ISAAC phases I (6–7 years old) and III (13–15 years old) in 1994 and 2002, respectively. During January–June 2012, the same period and the same questionnaires from the previous studies were used with some additional questions. The information was obtained by telephone interviews with participants conducted by staff at the Public Health Centre of Castellon and other health institutions. The questionnaire included items on asthma, eczema and allergic rhinitis following the ISAAC methodology. In addition, information about risk factors for asthma was based on specific questionnaires completed by the parents of participants in the ISAAC phases I and III in 1994 and 2002, respectively.
Definition of asthma was based on a positive response to at least one of the following questions.
Have you ever had asthma?
Do you take any medication for asthma?
Has the doctor diagnosed asthma?
From 3607 schoolchildren who participated in the ISAAC phase I in 1994, 1805 schoolchildren took part in 2002 in the ISAAC phase III,4 and 1435 (79.5%) adolescents were follow-up to 2012; 370 (20.5%) adolescents were lost to follow-up. Of the 1435 follow-up participants, 1280 were free of asthma in 2002.
Statistical analysisThe cumulative incidence of asthma was estimated considering the new cases divided by the follow-up participants with a 95% confidence interval (CI), considering a binomial distribution. Asthma incidence density (AID) was estimated from the person – years of follow-up. Chi2 and Fisher tests were used to compare qualitative variables, and Kruskal–Wallis test was used for quantitative variables. Poisson regression models were used in the bivariate and multivariate analysis to study the relationship between asthma and risk or protective factors by the relative risk (RR) with 95% CI. For the multivariate analyses, independent covariates associated with asthma and an alpha value less than p<0.20 were included in the model to arrive at a model with all the covariates with a significant association. No interactions were observed among significant variables and all models had an adequate goodness-of-fit. Population attributable risk (PAR), the percentage of cases reduced by removal of a risk, and population prevented fraction (PPF), the percentage of cases prevented with an intervention, were calculated following the formulas proposed by Kleinbaum et al.5 The Stata® programme (version 12) was used in the statistical analysis.
The study was approved by the Ethics Committee of the General Hospital of Castellon and informed consent was obtained from each participant.
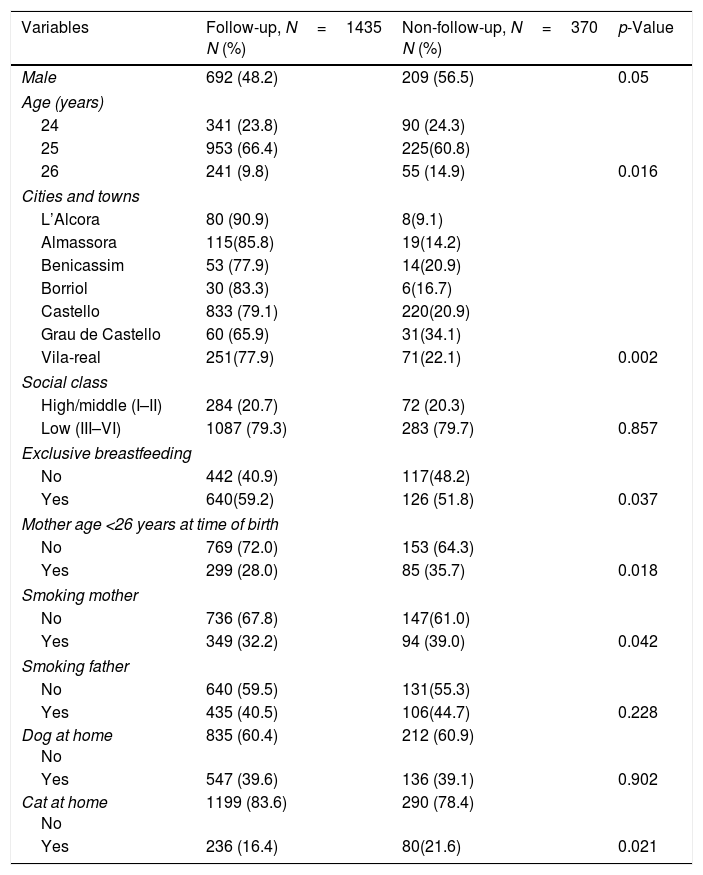
ResultsThe follow-up rate from 2002 to 2012 was 79.5% (1435/1805); 743 were female and 692 male; the mean age was 24.9±0.6 years. Some significant differences between the follow-up group and non-follow-up group are shown in Table 1. Participation was higher among females than males, in younger than older participants, and in small-town residents than city residents. Variables such as mother's age at time of birth, smoking mother, and cat at home were associated with lower participation. On the other hand, exclusive breastfeeding was associated with higher participation.
Characteristics of Castellon cohort: comparison of follow-up group with non-follow-up group.
| Variables | Follow-up, N=1435 N (%) | Non-follow-up, N=370 N (%) | p-Value |
|---|---|---|---|
| Male | 692 (48.2) | 209 (56.5) | 0.05 |
| Age (years) | |||
| 24 | 341 (23.8) | 90 (24.3) | |
| 25 | 953 (66.4) | 225(60.8) | |
| 26 | 241 (9.8) | 55 (14.9) | 0.016 |
| Cities and towns | |||
| L’Alcora | 80 (90.9) | 8(9.1) | |
| Almassora | 115(85.8) | 19(14.2) | |
| Benicassim | 53 (77.9) | 14(20.9) | |
| Borriol | 30 (83.3) | 6(16.7) | |
| Castello | 833 (79.1) | 220(20.9) | |
| Grau de Castello | 60 (65.9) | 31(34.1) | |
| Vila-real | 251(77.9) | 71(22.1) | 0.002 |
| Social class | |||
| High/middle (I–II) | 284 (20.7) | 72 (20.3) | |
| Low (III–VI) | 1087 (79.3) | 283 (79.7) | 0.857 |
| Exclusive breastfeeding | |||
| No | 442 (40.9) | 117(48.2) | |
| Yes | 640(59.2) | 126 (51.8) | 0.037 |
| Mother age <26 years at time of birth | |||
| No | 769 (72.0) | 153 (64.3) | |
| Yes | 299 (28.0) | 85 (35.7) | 0.018 |
| Smoking mother | |||
| No | 736 (67.8) | 147(61.0) | |
| Yes | 349 (32.2) | 94 (39.0) | 0.042 |
| Smoking father | |||
| No | 640 (59.5) | 131(55.3) | |
| Yes | 435 (40.5) | 106(44.7) | 0.228 |
| Dog at home No | 835 (60.4) | 212 (60.9) | |
| Yes | 547 (39.6) | 136 (39.1) | 0.902 |
| Cat at home No | 1199 (83.6) | 290 (78.4) | |
| Yes | 236 (16.4) | 80(21.6) | 0.021 |
Social class: I, professional; II, managerial and technical; III, skilled non-manual; IV, skilled manual; V–VI, partially skilled and unskilled.
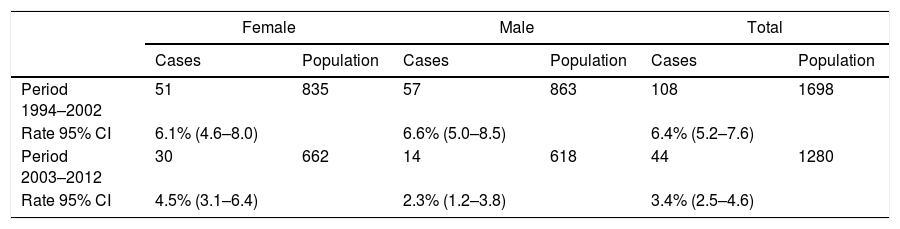
The comparison of the 1994–2002 and 2003–2012 periods is presented in Table 2. The cumulative incidence of asthma for the total, decreased from 6.4% (108 new cases/1698 participants) in the first period to 3.4% (44 new cases/1280 participants) in the second. A significant decrease is also observed for the AID. The AID obtained in our study was 3.5 cases per 1000 person – years, lower than the previous period, 8.2 cases per 1000 person – years (RR=0.43; 95% CI 0.3–0.6, p=0.000). For females, 7.9 and 4.6 cases per 1000 person – years (RR=0.59; 95% CI 0.38–0.92, p=0.021); for males 8.5 and 2.3 per 1000 person – years (RR=0.27; 95% CI 0.15–0.48, p=0.000), respectively.
Cumulative incidence of asthma by gender and age in the Castellon cohorts 1994–2002 and 2003–2012.
| Female | Male | Total | ||||
|---|---|---|---|---|---|---|
| Cases | Population | Cases | Population | Cases | Population | |
| Period 1994–2002 | 51 | 835 | 57 | 863 | 108 | 1698 |
| Rate 95% CI | 6.1% (4.6–8.0) | 6.6% (5.0–8.5) | 6.4% (5.2–7.6) | |||
| Period 2003–2012 | 30 | 662 | 14 | 618 | 44 | 1280 |
| Rate 95% CI | 4.5% (3.1–6.4) | 2.3% (1.2–3.8) | 3.4% (2.5–4.6) | |||
CI: confidence interval.
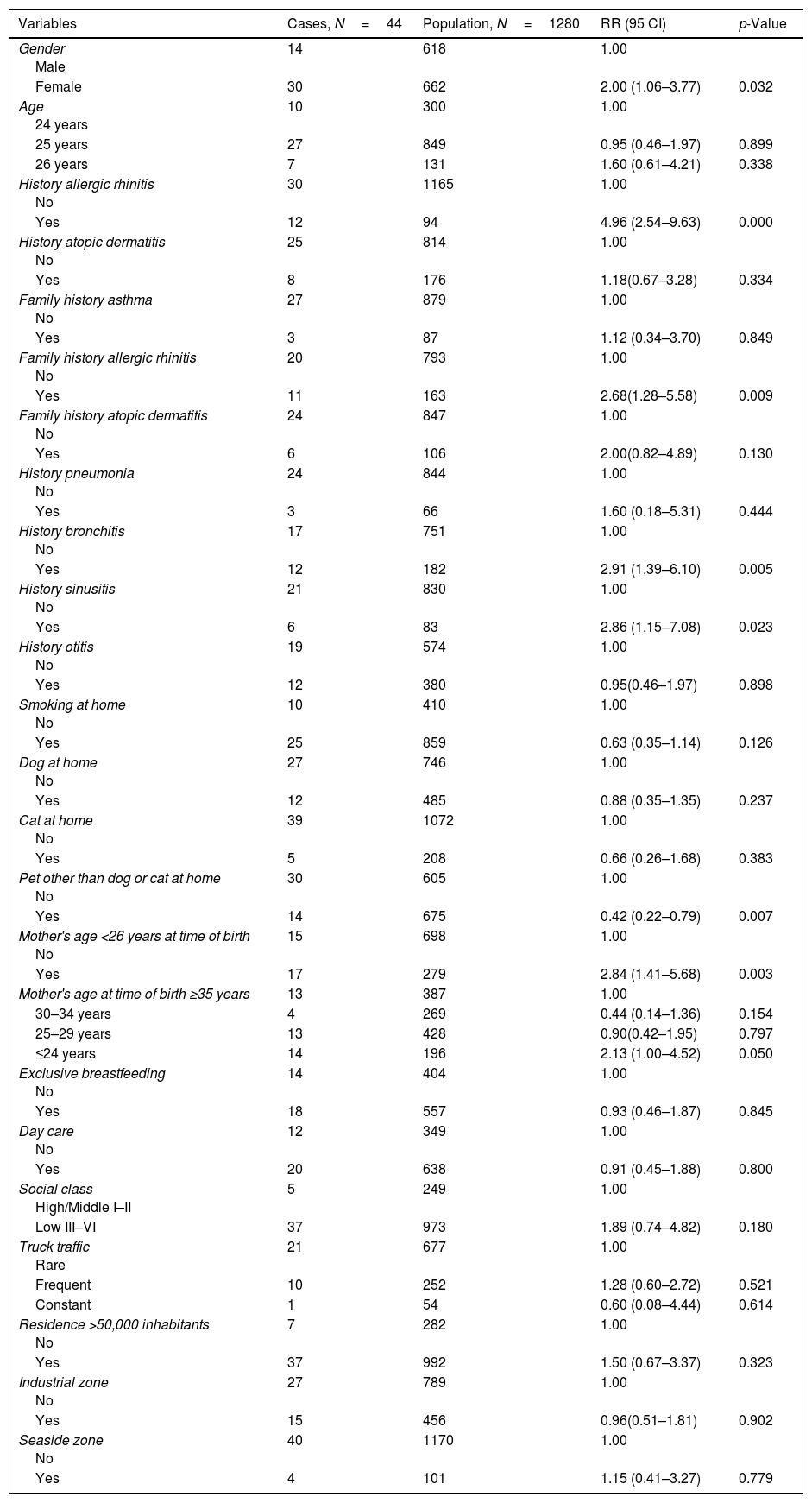
The bivariate analysis of risk and protective factors of asthma is presented by Poisson regression (Table 3). The asthma incidence was higher in females than males with a significant difference (RR 2.00; 95% CI 1.06–3.77, p=0.032). The significant factors associated with asthma were history of allergic rhinitis, family history of allergic rhinitis, history of bronchitis, history of sinusitis, mother's age at time of birth, and pet other than a dog or cat at home.
Bivariate analysis of risk factors for asthma in the Castellon cohort by Poisson regression.
| Variables | Cases, N=44 | Population, N=1280 | RR (95 CI) | p-Value |
|---|---|---|---|---|
| Gender Male | 14 | 618 | 1.00 | |
| Female | 30 | 662 | 2.00 (1.06–3.77) | 0.032 |
| Age 24 years | 10 | 300 | 1.00 | |
| 25 years | 27 | 849 | 0.95 (0.46–1.97) | 0.899 |
| 26 years | 7 | 131 | 1.60 (0.61–4.21) | 0.338 |
| History allergic rhinitis No | 30 | 1165 | 1.00 | |
| Yes | 12 | 94 | 4.96 (2.54–9.63) | 0.000 |
| History atopic dermatitis No | 25 | 814 | 1.00 | |
| Yes | 8 | 176 | 1.18(0.67–3.28) | 0.334 |
| Family history asthma No | 27 | 879 | 1.00 | |
| Yes | 3 | 87 | 1.12 (0.34–3.70) | 0.849 |
| Family history allergic rhinitis No | 20 | 793 | 1.00 | |
| Yes | 11 | 163 | 2.68(1.28–5.58) | 0.009 |
| Family history atopic dermatitis No | 24 | 847 | 1.00 | |
| Yes | 6 | 106 | 2.00(0.82–4.89) | 0.130 |
| History pneumonia No | 24 | 844 | 1.00 | |
| Yes | 3 | 66 | 1.60 (0.18–5.31) | 0.444 |
| History bronchitis No | 17 | 751 | 1.00 | |
| Yes | 12 | 182 | 2.91 (1.39–6.10) | 0.005 |
| History sinusitis No | 21 | 830 | 1.00 | |
| Yes | 6 | 83 | 2.86 (1.15–7.08) | 0.023 |
| History otitis No | 19 | 574 | 1.00 | |
| Yes | 12 | 380 | 0.95(0.46–1.97) | 0.898 |
| Smoking at home No | 10 | 410 | 1.00 | |
| Yes | 25 | 859 | 0.63 (0.35–1.14) | 0.126 |
| Dog at home No | 27 | 746 | 1.00 | |
| Yes | 12 | 485 | 0.88 (0.35–1.35) | 0.237 |
| Cat at home No | 39 | 1072 | 1.00 | |
| Yes | 5 | 208 | 0.66 (0.26–1.68) | 0.383 |
| Pet other than dog or cat at home No | 30 | 605 | 1.00 | |
| Yes | 14 | 675 | 0.42 (0.22–0.79) | 0.007 |
| Mother's age <26 years at time of birth No | 15 | 698 | 1.00 | |
| Yes | 17 | 279 | 2.84 (1.41–5.68) | 0.003 |
| Mother's age at time of birth ≥35 years | 13 | 387 | 1.00 | |
| 30–34 years | 4 | 269 | 0.44 (0.14–1.36) | 0.154 |
| 25–29 years | 13 | 428 | 0.90(0.42–1.95) | 0.797 |
| ≤24 years | 14 | 196 | 2.13 (1.00–4.52) | 0.050 |
| Exclusive breastfeeding No | 14 | 404 | 1.00 | |
| Yes | 18 | 557 | 0.93 (0.46–1.87) | 0.845 |
| Day care No | 12 | 349 | 1.00 | |
| Yes | 20 | 638 | 0.91 (0.45–1.88) | 0.800 |
| Social class High/Middle I–II | 5 | 249 | 1.00 | |
| Low III–VI | 37 | 973 | 1.89 (0.74–4.82) | 0.180 |
| Truck traffic Rare | 21 | 677 | 1.00 | |
| Frequent | 10 | 252 | 1.28 (0.60–2.72) | 0.521 |
| Constant | 1 | 54 | 0.60 (0.08–4.44) | 0.614 |
| Residence >50,000 inhabitants No | 7 | 282 | 1.00 | |
| Yes | 37 | 992 | 1.50 (0.67–3.37) | 0.323 |
| Industrial zone No | 27 | 789 | 1.00 | |
| Yes | 15 | 456 | 0.96(0.51–1.81) | 0.902 |
| Seaside zone No | 40 | 1170 | 1.00 | |
| Yes | 4 | 101 | 1.15 (0.41–3.27) | 0.779 |
RR: relative risk; CI: confidence interval; some items had incomplete information.
Sociastabl class: I, professional; II, managerial and technical; III, skilled non-manual; IV, skilled manual; V–VI, partially skilled and unskilled.
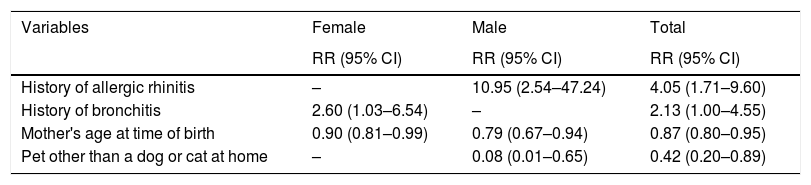
In the Poisson regression model (Table 4), four factors were associated with the incidence of asthma, history of allergic rhinitis (RR=4.05; 95% CI 1.71–9.60), history of bronchitis (RR=2.13; 95% CI 1.0–4.55), mother's age at time of birth (RR=0.87; 95% CI 0.80–0.95) and pet other than a dog or cat at home (RR=0.42; 95% CI 0.2–0.9). For males, the risk factor was personal history of allergic rhinitis (RR=10.95; 95% CI 2.54–47.24), and protective factors were mother's age at time of birth (RR=0.79; 95% CI 0.67–0.94) and pet other than a dog or cat at home (RR=0.08; 95% CI 0.01–0.65). For females, the risk factor was history of bronchitis (RR=2.60; 95% CI 1.03–6.54) and a protective factor was mother's age at time of birth (RR=0.90; 95% CI 0.81–0.99). Mean of mother's age at time of birth was 25.1±4.7 years for cases and 28.2±4.8 years for non-cases (p=0.0006). In the multivariate Poisson regression model, for mother's age less than 26 years the RR of asthma was 2.54 (95% CI 1.2–5.34).
Risk and protective factors of asthma incidence in the Castellon cohort: Poisson regression analysis.
| Variables | Female | Male | Total |
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| History of allergic rhinitis | – | 10.95 (2.54–47.24) | 4.05 (1.71–9.60) |
| History of bronchitis | 2.60 (1.03–6.54) | – | 2.13 (1.00–4.55) |
| Mother's age at time of birth | 0.90 (0.81–0.99) | 0.79 (0.67–0.94) | 0.87 (0.80–0.95) |
| Pet other than a dog or cat at home | – | 0.08 (0.01–0.65) | 0.42 (0.20–0.89) |
We estimated the PAR% and PPF% after the Poisson regression analysis. The PAR% were 20.5% for history of allergic rhinitis and 22.0% for history of bronchitis, both higher than those obtained in the previous period, 4.4% and 18%, respectively. Considering the mother's age at time of birth less than 26 years in the same Poisson regression model, the PAR% was 32.3% and the PPF% of pet other than a dog or cat at home was 30.6%.
DiscussionIn the area of Castellon, the incidence of asthma between 13–15 years old and 23–25 years old was 3.44%. A significant decrease of asthma from the 1994 to 2002 cohort study was observed4 with an incidence rate of asthma of 8.2 per 1000 persons/year, and 3.5 per 1000 person – years in the present study, although the follow-up of the two studies were 8 and 10 years, respectively. By gender, the biggest fall was among males.
Few studies have been published to date on the incidence of asthma in young adults. Moreover, comparisons are not easy to make due to differences in case definition, periods of study, and asthma diagnosis. In an international adult population study,3 age 20–44 the cumulative incidence of asthma was 3.9%, like our study. Incidence of asthma in a Spanish adult cohort (age 20–44) based on the European Community Respiratory Health Survey was 5.53 cases per 1000 person – years,6 and in a Huelva cohort7 with the same age as the Spanish cohort it was 4.76 cases per 1000 person – years, both higher than our study.
The risk factors for asthma in the 1994–2002 cohort study4 were history of allergic rhinitis, history of bronchitis, high social class (groups I–II versus III–VI) and family history of asthma. In our study the risk factors were history of allergic rhinitis and history of bronchitis, and two protective factors were mother's age at time of birth and pet other than a dog or cat. If we compare the results to the study published in 20074 on the same cohort but 10 years earlier, factors associated with asthma have changed. History of allergic rhinitis and bronchitis remain risk factors, but both with relative risks greater than those detected in 2002. In addition, asthma was a risk factor of allergic rhinitis incidence in this young adults cohort.8 This suggests that risk factors may change following the development from adolescence to adulthood. Modifying factors may have influenced asthma and be part of the cause of the decrease in the incidence and the prevalence of stabilisation.
Some of these factors are found in other cohort studies, including history of allergic rhinitis,3,9 history of bronchitis,3,10 and other risk factors have been identified, such as parental asthma and allergic rhinitis, poor parents, mother who smoked during pregnancy, early or late day-care attendance or respiratory infections.11,12 In 2009, the study of prevalence of this cohort detected a protective association with a pet other than a dog or cat and mother's age at time of birth and asthma.13 The relationship between the mother's age to asthma observed in some studies could be associated with prenatal and maturity level.14,15 On the other hand, owning rodents or birds has not been associated with asthma incidence in eleven European birth cohorts.16 However, in the United Kingdom one birth cohort study found that pet ownership was associated with reduced atopic asthma and increased non-atopic asthma.17
Females have up to two times more risk of developing asthma. Cumulative incidence was also higher among women than men (4.53% versus 2.27%) as well as an increased risk of asthma attacks, night-time awakenings, need for medication and wheezing in the last year. Other cohort studies also detected this difference between sexes.3,18 In childhood, asthma is more common in males,19,20 reaching a plateau in adolescence between the two sexes in adulthood to reverse the trend, when it becomes more frequent in women. We believe the effect of female sex hormones could be playing an important role as a modulator of the inflammatory response and the occurrence of cyclical changes in airflow and lung diffusion capacity.21–23
The risk and protective factors found in our study indicate the evidence of the multi-factorial aetiology of asthma and these factors change with the age. In addition, genome-wide association studies have discovered genetic loci of asthma risk.24–26 Per the latest theories on the aetiology and the appearance of new asthma phenotypes-endotypes,27,28 we believe that this disparity regarding risk factors is due to limited knowledge about the origin of the disease.
Few national studies based on the young adult population have examined the incidence of asthma. In Spain, there are no studies assessing the evolution of the incidence of asthma and associated factors from adolescence to adulthood, perhaps because of the complexity of tracking a cohort of individuals at great risk of dispersion. For this reason, our study makes a unique contribution to date.
The study has some strengths, including the prospective design, a sufficiently large sample to detect potential risk factors, acceptable follow-up, and the use of the same core questionnaire.29 However, the following limitations should be noted: the follow-up losses were associated with gender, some items were not completed by the participants, some risk factors for asthma such as diet and home characteristics, ambient air pollution, and vitamin D status were not included in the study,30–32 no objective measures were used in this study such as lung function or allergy skin prick test33 and the case definition of asthma was based on self-reported asthma34 and under-diagnoses of asthma could have occurred.35,36
ConclusionA significant decrease in the incidence asthma was observed when the age increased. History of rhinitis, history of bronchitis, mother's age at time of birth and a pet other than a dog or cat were the factors associated with asthma.
Conflict of interestThe authors have no conflict of interest to declare.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
We thank the participants and their families for their cooperation in making the study possible.