There are many educational events for physicians in different countries covering one or some of the allergic diseases. Most of these educational events have been reported to improve care by the physicians. The aim of this study was to determine the baseline knowledge of general practitioners (GP) regarding the systemic nature of childhood allergy and atopic march, and to assess the influence of an educational event on this baseline knowledge.
MethodsTwo hundred and two GPs from five different cities in Turkey who attended education seminars were enrolled. All GPs were received the questionnaire both before and after the seminar. The questionnaire had statements about the systemic nature of childhood allergies and the atopic march, and GPs were asked to mark their degree of agreement as (completely true, partially true, wrong).
ResultsMean age of GPs was 38.6±6.0 years. Mean duration after graduation from medical faculty was 13.9±6.5 years. There was significant improvement in answers after education. The statement “Frequency of allergic rhinitis and asthma is not as high as expected in children with atopic dermatitis” was regarded “wrong” by 60.9% but increased to 94.3% after the education (p<0.001). Systemic nature of allergy was approved by 72.8%, which increased to 99% after the education (p<0.001). Adrenalin as first line treatment in anaphylaxis treatment was appreciated by a higher number of GPs with the education (p<0.001).
ConclusionMany GPs lack updated information about the systemic nature of paediatric allergic diseases and a single educational event may improve their knowledge significantly.
Allergic diseases including asthma, atopic dermatitis, and urticaria are the most common diseases of childhood. In a study from Turkey, the prevalence of having at least one allergic disease has been reported as 27% and in another study which included many regions of Turkey, prevalence has been reported to range between 4-21% for individual allergic disease.1,2 Therefore, children with allergic diseases compromise a major group among children with chronic diseases who present to physicians.
Primary care physicians provide two thirds of all ambulatory asthma care in the United States.3 This is similar to Turkey where general practitioners (GPs) are the first centres which children see most of the time, thus it is vital to assess knowledge of the GPs about the systemic nature of allergic diseases in children and to provide them with continuing postgraduate education about risk factors, diagnosis, and management of these disease. Most of the physicians from different countries report having heard of guidelines, especially about asthma diagnosis and management yet fall short of practising these.4,5
There are many educational events in different countries covering one or some of the allergic diseases, such as the “Asthma Training Centre” in the United Kingdom which includes both nurses and physicians.6 Most of these educational events about asthma have been reported to improve care by the physicians.6 There are seminars about different fields of allergy, mostly asthma and allergic rhinitis (AR) in Turkey, too. However, these meetings are locally organised, do not include information about children and the systemic nature of allergy in children, and they involve specialists. Therefore, the aim of this study was to determine the baseline knowledge of general practitioners about the systemic nature of childhood allergy and the atopic march and to assess the influence of an educational event on this baseline knowledge.
Materials and methodsStudy populationTwo hundred and two GPs aged between 24 and 57 who attended one of the five education seminars that were held in five different cities of Turkey during a two-year period were enrolled in the study. These cities were chosen to represent different regions of Turkey.
Study designAll the GPs who attended the seminars were given a questionnaire about the systemic nature of childhood allergies and the atopic march before the seminar started. They were instructed not to write down their names on the questionnaire forms and were explained that the aim was not to do individual assessment but to obtain information for planning of future educational events. The same questionnaire was administered right after the education seminar finished.
Education eventsEach educational event lasted half a day and consisted of five main topics including the definition and pathogenesis of paediatric allergic diseases; clinical findings of paediatric allergic diseases; follow-up of paediatric allergic diseases; prognosis of paediatric allergic diseases; and co-morbidities of paediatric allergic diseases. Each topic was presented by one of the researchers. General aspects of treatment were mentioned in the clinical findings section. The main diseases discussed under the common name paediatric allergic diseases included asthma, AR, urticaria, atopic dermatitis (AD), food allergy, and anaphylaxis. All the slides used in the seminars were the same and were prepared and approved by all the researchers.
QuestionnaireA self-administered questionnaire was developed by the researchers, addressing knowledge about pathogenesis; clinical findings; prognosis; follow up; and co-morbidities of paediatric allergic diseases, including asthma; AR; AD; food allergies; urticaria; and anaphylaxis. The questionnaire consisted of 28 items. Statements were given in each item and GPs were asked to mark their extent of agreement (completely true, partially true, wrong) and a last choice of “I don’t know” was added. All the statements were in agreement with the content of the education slides.
Statistical analysisChi square test was used to compare frequencies of the answers given to each question. Comparisons were made for answers before and after the educational event and answers given by GPs who had graduated from medical faculty in the previous 10 years or earlier. Moreover, answers of GPs who had attended an educational seminar about paediatric allergies were compared with the ones who had not.
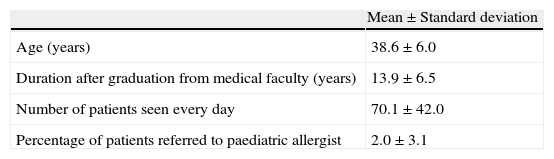
ResultsSociodemographic characteristics of the general practitionersMean age of the GPs enrolled in the study was 38.6±6.0 years. Mean duration after graduation from medical faculty was found to be 13.9±6.5 years (Table 1). One hundred and fifty four GPs gave information about the date of graduation and 57 of these had graduated within the previous 10 years. Most of the GPs were working at a primary care centre of the Ministry of Health (76.7%). Other areas of work included State hospitals, private offices and clinics of special institutions. Among the GPs, 3.5% did not answer this question.
The average number of patients seen was reported to be 70.1±42.0 and the mean percentage of referral to a paediatric allergist was 2.0±3.0 (Table 1).
Among the GPs, 20.3% had attended an education event about allergy before, while 76.2% had not attended any postgraduate educational event about allergy and 3.5% did not answer this question (Table 1).
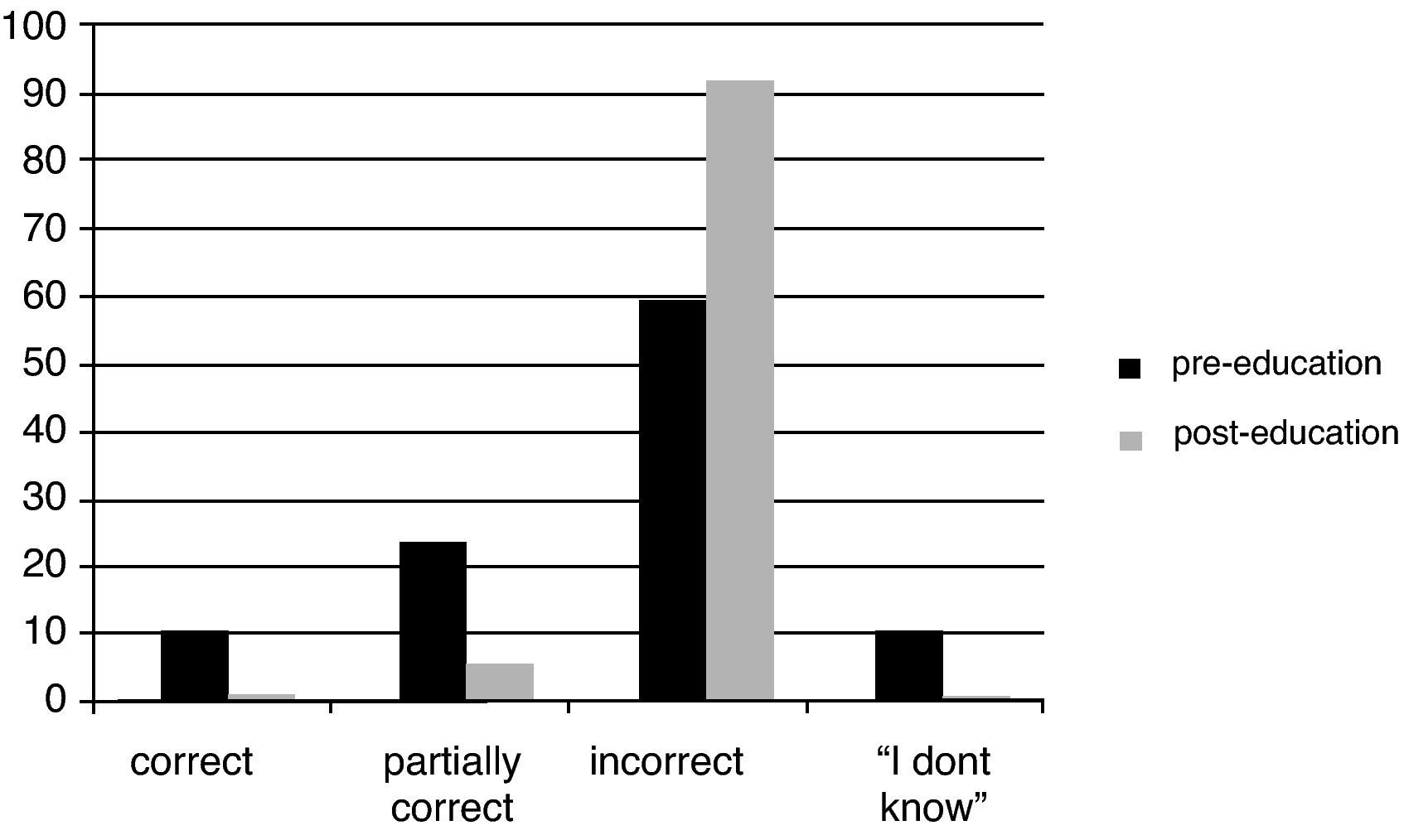
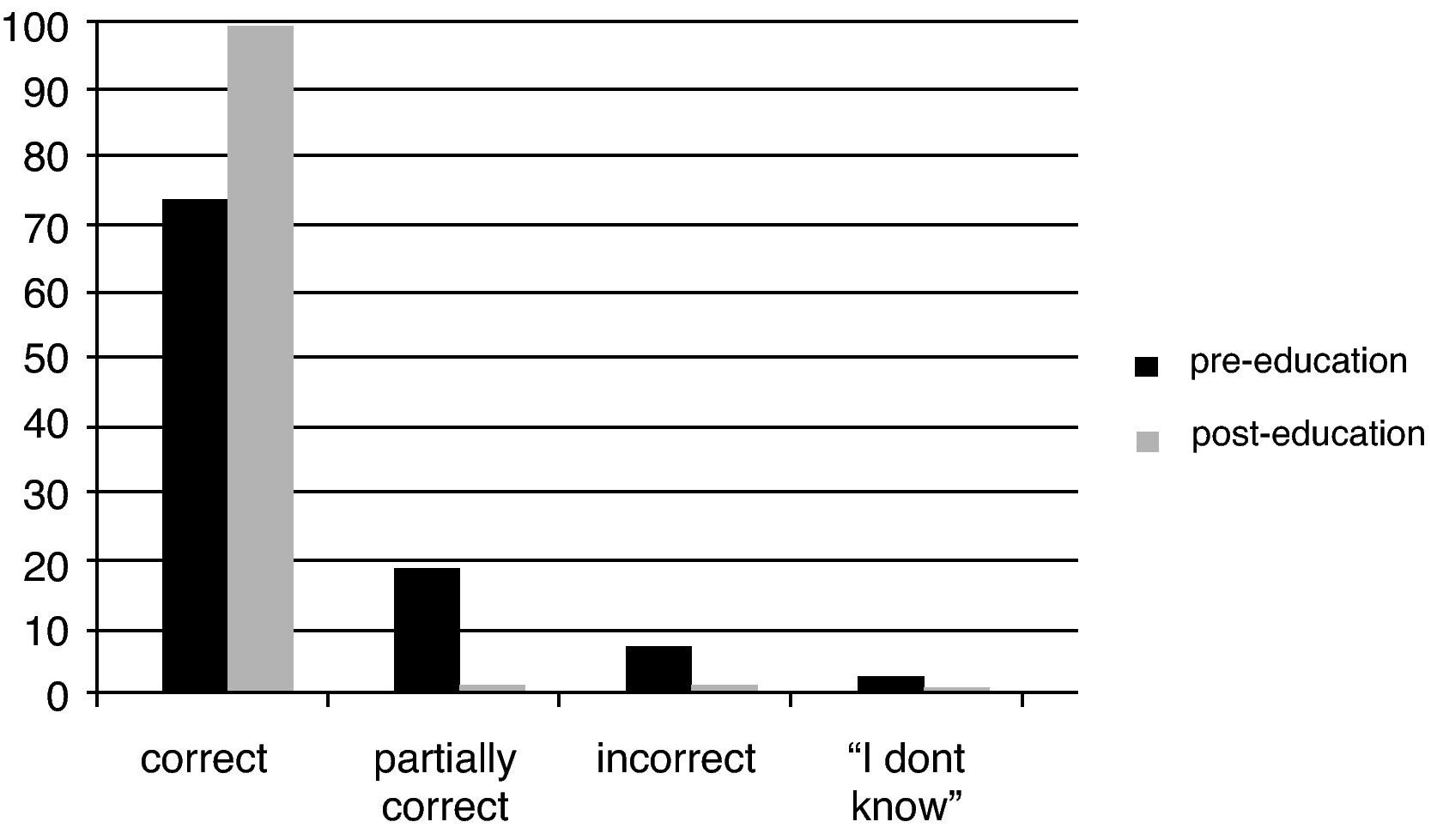
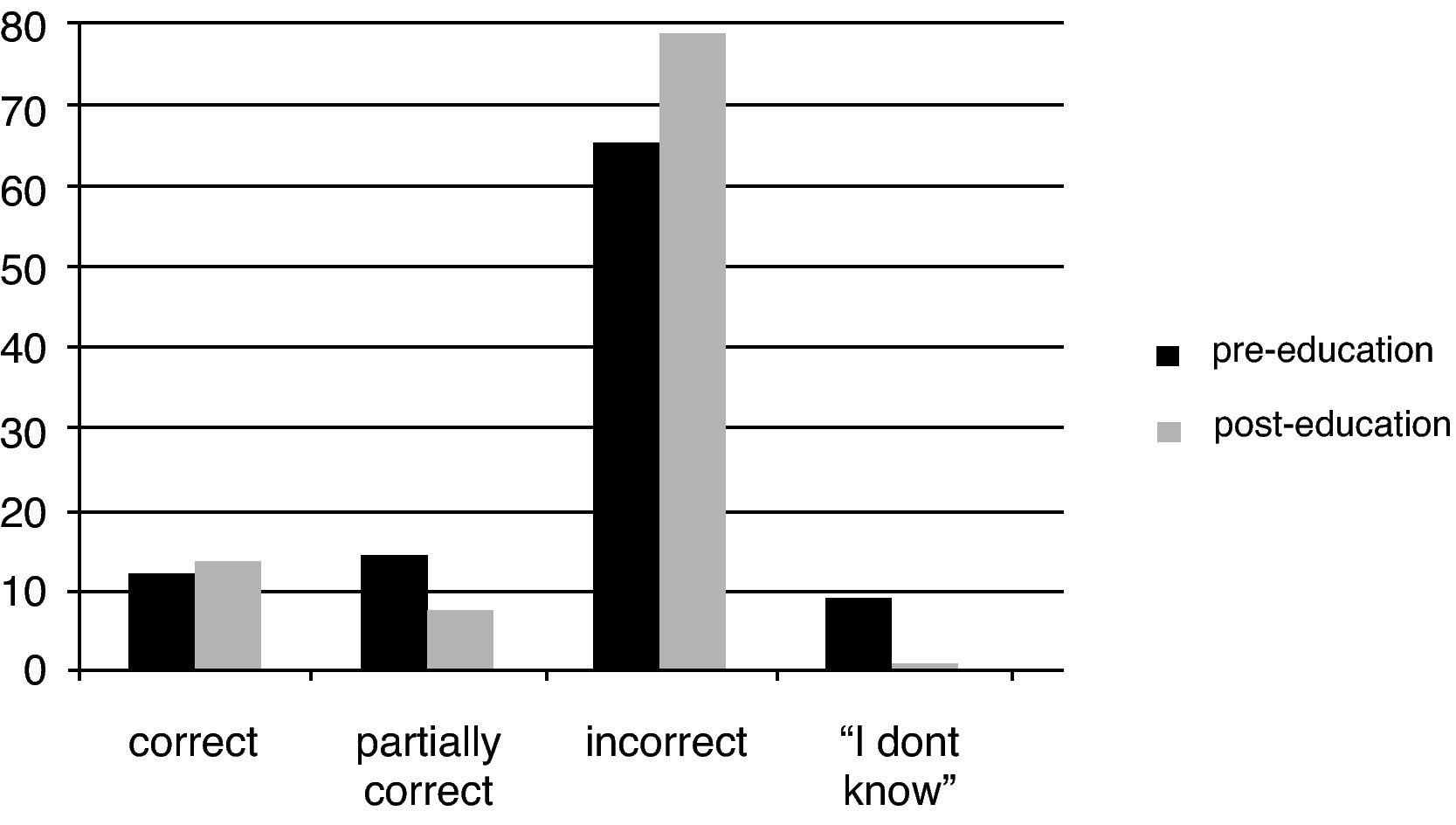
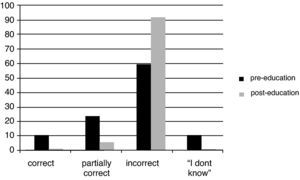
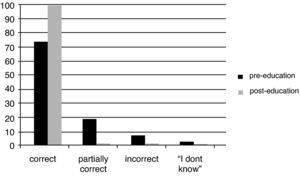
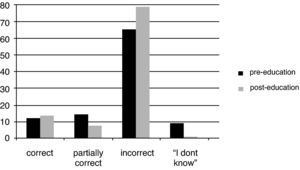
Responses to questions about the pathogenesis of childhood allergic diseasesThe definition of atopy as a tendency for an IgE-mediated immune reaction was recognised as true by 76.2% of the GPs before the seminar and this increased to 95.9% after the education (p<0.001). The statement “Frequency of AR and asthma is not as high as expected in children with AD” was regarded as “wrong” by 60.9% of the GPs initially and this increased to 94.3% after the educational event (p<0.001) (Fig. 1). The systemic nature of allergy that is expressed in different organs was approved by 72.8% of the GPs initially and this increased to 99% after the educational event (p<0.001) (Fig. 2). Coexistence of genetic and environmental risk factors for the development of allergic diseases was regarded as correct by 94.6% and 100% of the GPs before and after education, respectively (p=0.01). Similarly there was a significant increase in the number of GPs who marked the statement “Absence of clinical findings in allergic diseases indicates that the inflammatory process has ended” as wrong (65.3% vs. 78.9%, p<0.001) (Fig. 3).
There was no significant increase in the number of GPs who regarded viral agents as triggering factors for asthma exacerbations before and after education (96.0% vs. 99.5%, p=0.07). On the other hand, the number of GPs stating that “Avoidance of allergens is the most important treatment in allergic diseases” was true increased significantly from 73.8% to 93.8% after the educational event (p<0.001). In addition, education increased the number of GPs who were aware of the fact that children with asthma may be completely normal between exacerbations (51.05 vs. 73.2%, p<0.001).
Similarly, recognition of xerosis and itching as clinical findings of AD increased significantly after the educational event (71.3% vs. 98.5%, p<0.001). Localisation of AD lesions to cheeks as well as neck was appreciated by an increased number of GPs with the education (p<0.001 for both). Another statement regarding AD, “It is possible to eliminate symptoms of AD to a great extent and to decrease social problems associated with it” was marked as “completely correct” by 57.4% of the GPs before the education vs. 97.9% after the educational event (p<0.001).
Recognition of cow's milk allergy as the most common food allergy and as a transient allergic sensitisation was increased among the GPs (p<0.001 for both). Moreover, use of soya-based formula for children with cows’ milk allergy was approved by an increased number of GPs after the education (36.6% vs. 90.2%, p<0.001).
There was an increase in the number of GPs who stated that “AR was the most common co-morbidity encountered in children with asthma” was correct after the educational event (53% vs. 80.9%, p<0.001). Additionally, recognition of AR as a proven risk factor for the development of asthma increased significantly with education (p<0.001). Moreover, the role of antihistamines and corticosteroids as the most effective treatment of AR was appreciated by an increased percentage of the GPs with education (78.7% vs. 93.2%, p<0.001).
The statement “Urticaria or angio-oedema is classified as chronic if the duration is longer than six months” was regarded as “incorrect” by 8.4% of the GPs before the education vs. 51% after the education (p<0.001). Diagnostic tests were found unnecessary in acute urticaria if history does not indicate a specific aetiological agent by more of the GPs after the education (17.8% vs. 60.8%, p<0.001).
The definition of anaphylaxis as a life-threatening IgE-mediated systemic reaction was recognised by an increased number of GPs after the education (88.1% vs. 97.9%, p<0.001). Moreover, skin and respiratory findings as the most common clinical findings, and adrenalin as the first-line agent in the treatment of anaphylaxis was appreciated by a higher number of GPs with the education (p=0.03 and p<0.001 respectively). The dose of adrenalin as 0.01mg/kg (max 0.3mg) was marked as correct by 77.7% of the GPs before education, and this increased to 99.5% after education (p<0.001).
Responses to questions about follow-up of childhood allergic diseasesThe importance of regular pharmacotherapy including inhaled corticosteroids and bronchodilators was recognised by 87.1% of GPs before vs. 98.5% after the educational event (p<0.001). The statement “Topical steroids are the first-line agents in the treatment of AD” was marked as completely true by 47.0% and 56.2% of the GPs before and after the educational event, respectively (p=0.007). Education increased the number of GPs who were aware of the fact that aetiology cannot be identified in around 80% of chronic urticaria cases (p<0.001). Moreover, there was an increase in the number of GPs who were aware of specific IgE as an alternative diagnostic method of allergen sensitisation for children in whom skin prick testing cannot be performed (p<0.001).
Comparison of the responses to questions before the educational event according to different characteristic of general practitionersWhen GPs who had graduated from Medical Faculty within the previous 10 years and the ones who had graduated earlier were compared before the educational event, a significant difference was not present for most of the questions (p>0.05). However, a higher number of GPs who had graduated earlier than the previous 10 years recognised that the statement “Children with asthma are completely normal between exacerbations” was correct (p=0.048). Moreover, use of soya-based formula for children with cows’ milk allergy was approved by 22.8% of the GPs who had graduated within the previous 10 years versus 41.2% of the GPs who had graduated earlier (p<0.001). The statement “Further diagnostic testing is not required in cases of acute urticaria in which history does not point out a specific aetiological agent” was marked as incorrect by 63.2% of the GPs who had graduated within the previous 10 years versus 37.1% of GPs who had graduated earlier, but the number of answers as “I don’t know” was higher in the latter group (10.5% vs. 21.6) (p=0.004). In addition, the use of adrenalin as the first agent to use in anaphylaxis was regarded as wrong by a higher number of the GPs who had graduated within the previous 10 years (10.5% vs. 1.0%, p=0.005).
Previous attendance to an educational event did not make a significant difference in the responses to the questions (p>0.05 for all). Similarly, there was no significant difference in the responses of the GPs from different regions (p>0.05 for all).
DiscussionIncreasing awareness of the primary care physicians about the systemic nature of allergy and the atopic march is a very important step in improving paediatric patient care. In this study it was detected that 76% of the primary care physicians who participated in the study had not attended an educational event about allergy in childhood before. This was very much lower than the number reported by a study which had been performed in the United States about primary care physicians’ knowledge about NAEPP guidelines, where 79% of all physicians had attended a post-graduate education seminar about asthma.3
In a study performed in five European countries including Germany, Norway, Netherlands, Sweden and Slovak Reunion, it was detected that inhaled corticosteroids were prescribed to nearly half of the patients with asthma.7 This study, which was performed in 2001, demonstrated significantly lower rates of inhaled corticosteroid use than our results.7 Regular long-term treatment with inhaled corticosteroids was regarded as completely correct by 87.1% of the GPs before the education and by 98.5% after the education in our study. However, there are two important differences between these two studies. One is that the previous study was not completely knowledge questionnaire based but relied on patient scenarios. Second, there is a six-year difference between the two studies and during this time awareness of inhaled corticosteroid use has increased and emphasis increased in guidelines.8 Another study carried out on GPs in Australia reported that around 68% of GPs regarded inhaled beclomethasone as a useful drug for children with asthma.9 This percentage is below pre- and post-education percentages of GPs in our study, which regard chronic treatment of asthma with inhaled corticosteroids as important. Again there is a time difference between this study which was published in 1994 and ours. This might have contributed largely to the difference. Thus, in a more recent study from Missouri, use of inhaled corticosteroids in patients with asthma was around 80%, which is much closer to the frequency in our study. In addition, in a recent study from Turkey most of the physicians had indicated that inhaled corticosteroids were drugs of choice for maintenance asthma treatment.10
There was significant improvement in the questions about pathogenesis of asthma and allergy including the systemic nature of disease and genetic and environmental contribution to development and in the questions about treatment of asthma such as the need for long-term treatment with inhaled corticosteroids. None of the previous studies have evaluated the influence of education about allergic diseases in children as a systemic disease but there are many which have evaluated the effects on educational programmes about asthma.4,11–14 Similarly, in a previous study that handed out simplified protocols about asthma management to physicians, they have reported that regular asthma education programmes with a specific focus on documentation skills are needed, to improve care.11 Likewise, physicians who participated in another study stated that they had changed their asthma management protocol after consulting guidelines.4 The education seminar that was given to the general practitioners in our study was specifically designed to aid in everyday practice, avoiding too many details. This way of providing practical information might have improved the general concentration of the GPs to listening. Both our results and the results of the previous studies emphasise that an educational event in a simple form which gives out simple messages might improve compliance and results.11 Improvement of patient care assessment was done by evaluating patient outcome in another study that assessed education of physicians, and it was determined that training reduced symptoms of children with asthma up to two years after the programme.12 This study showed that education does not only increase knowledge of physicians but also improves patient outcomes, which is the final aim of all educational events for physicians.12
Anaphylaxis is an emergency and it is vital that all physicians are aware of adrenalin as the first drug of choice.15 When the pre-education answers were reviewed, it was noted that only around 80% of the general physicians marked this statement as completely correct and this increased to 97% after the educational event. A study on paediatricians about the importance of allergy in Missouri reported that 89% were aware of this in 1971, while 100% were aware in 1998.15 The pre-education knowledge of the GPs in Turkey before the education was quite below that in Missouri but with education it increased to comparable levels. When it is considered that only 21% of the general physicians had attended a seminar about allergy before, this emphasises the importance of post-graduate education in attaining a level of patient care that is internationally acceptable. A previous study that evaluated paediatricians’ knowledge about anaphylaxis diagnosis and management using a case-based questionnaire, reported that around 80% of paediatricians who diagnosed a case with anaphylaxis chose to administer adrenalin.16 This was similar to the GPs in our study before the seminar. In the previous study on paediatricians, it was found that paediatricians who had completed residency training more than 10 years ago were more likely to use epinephrine. Similarly, in our study there was a significant difference in the GPs who graduated from medical faculty before or after the previous 10-year period. Although the percentage of complete agreement with the statement that suggested adrenalin as the first line of treatment in anaphylaxis was 84% among the GPs who had graduated from medical faculty within the previous 10 years, around 10% had stated that this was incorrect. Among the GPs who had graduated earlier than the previous 10 years, only 1% had regarded this statement as completely incorrect. This is similar to the report about paediatricians in the above-mentioned study in that more of the GPs who had graduated earlier were aware of the importance of adrenalin treatment in cases of anaphylaxis.16
Mean percentage of patients who were referred to paediatric allergy specialists by the general physicians was around 2% in our study, and about 18% had stated that they do not refer any patients. This value was considerably higher than the paediatricians in Missouri, of whom only 2% had not referred patients to an allergist.15
One of the major limitations of the study was the subject bias. In other words, GPs who had an education about allergic diseases in childhood recently might not have been willing to participate in the seminar. However, as far as we know there have not been similar seminars about the systemic nature of paediatric allergic diseases in Turkey.
In conclusion, general practitioners, who are the first line of medical care that children present to, do not seem to receive adequate postgraduate medical education about the systemic nature of childhood allergies. Therefore, many lack updated information about the systemic nature of childhood allergy. However, a single educational event in the field may improve their knowledge significantly. Therefore, long-term educational planning on childhood allergic diseases needs to be performed on a nationwide basis.
Conflict of interestThe authors report no conflict of interest.
The research project was carried out by the Pediatric section of the Sigma Turkey project which was supported by UCB-Institute of Allergy.