Excess body mass increases the risk of development of asthmatic symptoms and their severity and decreases the treatment effectiveness. One of the hypotheses explaining the link between the two diseases concerns the adipokines, hormones produced by adipose tissue with a proinflammatory character. The aim of this study was to compare the levels of the adipokines (leptin and resistin) between overweight asthmatic patients, asthmatic patients with normal weight and overweight patients without asthma.
Methods80 peripheral blood samples were collected from patients and blood serum extracted. Three groups were selected: overweight asthmatic patients (BMI≥25), overweight patients without asthma and asthmatic patients with normal weight (BMI<25). Waist circumference of the patients was measured (cut-off points were 80cm for women and over 94cm for men) and a skin prick test performed. Comparison of adipokine concentration between the 3 groups was made and association between these concentrations and the measurements was performed.
ResultsAlthough the concentrations of both adipokines were slightly higher for overweight asthmatic patients compared to overweight healthy patients, these differences were not significant. A significant association was found between leptin concentration and both BMI (p<0.01) and waist circumference (p<0.01). A difference for this cytokine was also found between asthmatic and non-asthmatic female patients (p<0.05).
ConclusionsAs expected overweight patients with BMI≥25 and patients with increased waist circumference showed higher leptin levels. We suggest that the studied cytokines, with a stronger indication for leptin, can elicit asthmatic inflammation in obese phenotype of asthma that affects more frequently women.
As defined by the World Health Organization (WHO) asthma is a chronic inflammatory airways disease characterized by recurrent attacks of wheezing and breathlessness.1 Asthma inflammation involves the recruitment of various cells and cellular elements such as immunoglobulins and cytokines that will result in airways mechanical and physiological changes. Asthmatic patients have narrowed airways due to the bronchi edema and thickening achieved by the hypertrophy and hyperplasia of the smooth muscle cells (result of the VEGF – vascular endothelial growth factor secretion) and their contraction. Additional airflow problems are caused by the increased secretion of mucus.2
Obesity and overweight is “abnormal or excessive fat accumulation that may impair health”.3 In the last decades the prevalence of asthma and obesity increased significantly in industrialized countries becoming a burden not only for affected patients but also public health systems.4,5 This convergence captured the interest of researchers and resulted in various studies examining the link between the two conditions. It soon became clear that obesity is a strong risk factor for asthma development, affecting prevalence, severity and treatment effectiveness in obese patients.6
Body mass index (BMI) measured in kg per square meter is the most commonly parameter used to assess the excess of weight and obesity. Numerous epidemiological studies found a significant association between BMI and asthma symptoms both in adults7,8 and children.9 However, contrary results can also be found.10,11 BMI, despite being the most frequent, is not the most precise measure of the fat excess. This index describes only the relation of the total body mass to height, not taking into consideration the actual proportion of the fat versus lean mass or the fat distribution.
Another commonly used indicator for obesity, examining the fat distribution, is the waist circumference. Central obesity (fat concentration around the waist area) is a strong risk factor for cardiovascular diseases and type 2 diabetes.12 A study run in the Hunter Medical Research Institute, New Castle, Australia, considered in obesity-related asthma studies not only BMI but also body composition and waist circumference. A significant association was encountered indicating a detrimental impact of increased fat mass and both thoracic and android fat tissue on respiratory health (expiratory reserve volume – ERV) in women. In men the association was found with thoracic and android lean issue and ERV. However, leptin concentration, also included in this analysis, was positively associated with thoracic and android fat tissue in men.13
Several studies indicate that obesity-related asthma phenotype is observed more commonly in women. Von Behren et al. used not only BMI but also waist size in the cohort study of 88,304 women and found a positive association between these measurements and current asthma, with waist circumference being independently associated with asthma symptoms, even in the group of women with normal BMI status.14
Various hypotheses were presented trying to explain the mechanism causing the association. One explanation focuses on the common environmental factors for both diseases, namely sedentary lifestyle and changes in diet. Other hypotheses implicate the reduced lung capacity caused by the mechanical impact of body mass on the chest, gastroesophageal reflux and sleep-disordered breathing.15 Recent studies have shown that adipose tissue has not only a passive energy storage role but is also physiologically active having endocrine functions. Hormones secreted by this tissue are called adipokines and their main role is to regulate hunger and satiety, although they are also involved in inflammation processes. The most indicated adipokines suggested to have an impact on asthma development are leptin and resistin.16 Leptin is a 16kDa protein of 167 amino acids is a product of ob gene (gene of obesity) in humans. Food intake results in the increased expression of this gene and as a consequence, of leptin serum concentration. The leptin receptor gene (db) is expressed in the lung tissue. The presence of the receptors itself indicates the lungs as the target organ for this hormone.17 Resistin is a recently discovered 12.5kDa adipokine belonging to a cysteine-rich secretory protein family. Resistin is expressed in human macrophages, bone marrow, spleen, mononuclear leucocytes and at low levels in adipose tissue. This hormone concentrates around the inflamed tissue, up-grading its own expression and promoting the NF-κB activation and cytokine production ipso facto triggering the inflammation. Similarly to leptin, resistin levels increase with increased adipose mass.18 Both hormones described above are important mediators of the metabolic processes with pro-inflammatory character. Higher serum concentrations of both adipokines were observed in asthmatic patients with an even stronger association for women.19
MethodsQuestionnaire data collectionThe database and sample used in this work is a part of a larger project making part of the Global Allergy and Asthma European Network (GA2LEN).20 Data collection was carried out in 2010 and centered on the population-based sample of 2200 individuals aged between 18 and 74 years old. As recommended by the GAL2EN protocol, the sample was selected randomly. A short questionnaire including questions about birth date, gender and asthma symptoms was handed to the participants to be filled in and returned by mail. Three attempts were undertaken in order to obtain the best response rate. A skin prick test was conducted on the randomly selected sub-sample of asthmatics. The presence of asthma symptoms was determined using the GINA classification.21
Anthropometric measurementsAll the individuals participating in the study were measured and weighed (with light clothing and barefoot). BMI was calculated with the formula
Using the cut-off points recommended by the WHO we considered individuals with a BMI value equal to or greater than 25 as overweight and equal to or greater than 30 as obese, but due to the small sample of obese patients, we included the obese individuals in overweight group and used it as one for all the analyses.
Waist circumference was measured using the measuring tape, and, as recommended by the WHO, cut-off points of 80cm and 94cm were used for women and men, respectively.
Final sample selectionIndividuals born before 1945 were excluded from the study, as they are already classified as elderly and could express hormonal changes related to the aging process rather than fat tissue excess or asthmatic inflammation. Three groups were selected in order to perform the adipokine concentration comparison. Overweight (including obese) patients with asthma (28 individuals) and overweight without asthma (26 individuals) were selected in order to measure the impact of asthma on adipokines serum concentrations. The third, the control group, consisted of asthmatic patients with BMI values within normal range (26 individuals).
Adipokine concentration measurementsThe blood serum of the 80 selected individuals was analyzed to measure the leptin and resistin serum concentration using ELISA kits. As the dilution proportions were suggested in the protocol, after a bibliographic research and optimization protocol for several dilutions we chose to use 1:20 dilution for leptin and left the resistin undiluted. The minimum detectable concentration was 0.016ng/ml for resistin and 0.313ng/ml for leptin.
Statistical analysesThe Software PASW Statistics v18 and Numbers ‘09 was used for the data processing and statistical analysis. Values of p<0.05 were considered as statistically significant. To compare the concentrations between selected groups, Kruskal–Wallis and Mann–Whitney U test were used as the data did not have a normal distribution (KS<0.05). Values for women were calculated separately due to the hypotheses of phenotype of obesity-related asthma having a stronger association with the female gender.
ResultsFor the purposes of the investigation three groups were selected:
Group 1: 28 asthmatic individuals with BMI≥25kg/m2 (mean BMI=30.4±4.3); assigned as overweight with asthma (including 14 obese patients with BMI>30).
Group 2: 26 non-asthmatic individuals with BMI≥25kg/m2 (mean BMI=28.9±4.2); assigned as overweight without asthma (including 9 obese patients with BMI>30).
Group 3: 26 asthmatic individuals with BMI<25kg/m2 (mean BMI=21.6±1.9); assigned as normal weight with asthma.
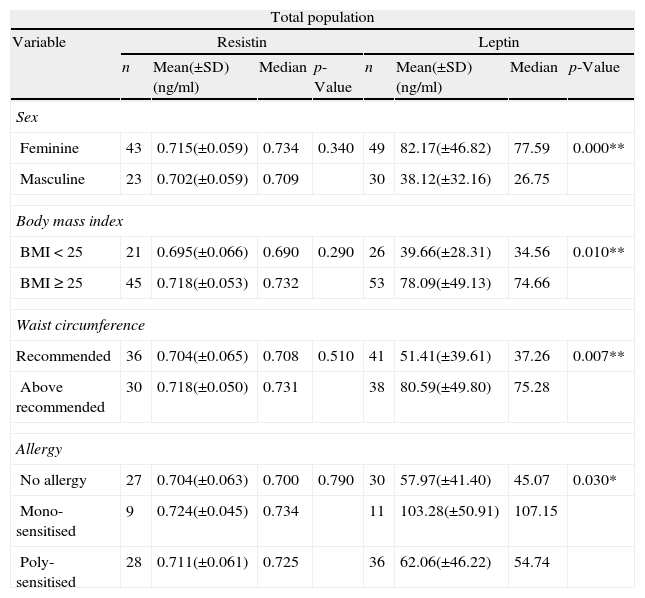
Women had significantly higher serum levels of leptin compared to men. Serum concentrations of resistin in women also occurred higher but the difference was not significant (Table 1).
Comparison of leptin and resistin serum concentrations within selected variables for total studied population. Non-parametric tests, Kruskal–Wallis and Mann–Whitney, were used to compare the concentrations between groups and the p≤0.05 was considered significant (*) and p≤0.01 strongly significant (**).
| Total population | ||||||||
| Variable | Resistin | Leptin | ||||||
| n | Mean(±SD)(ng/ml) | Median | p-Value | n | Mean(±SD)(ng/ml) | Median | p-Value | |
| Sex | ||||||||
| Feminine | 43 | 0.715(±0.059) | 0.734 | 0.340 | 49 | 82.17(±46.82) | 77.59 | 0.000** |
| Masculine | 23 | 0.702(±0.059) | 0.709 | 30 | 38.12(±32.16) | 26.75 | ||
| Body mass index | ||||||||
| BMI<25 | 21 | 0.695(±0.066) | 0.690 | 0.290 | 26 | 39.66(±28.31) | 34.56 | 0.010** |
| BMI≥25 | 45 | 0.718(±0.053) | 0.732 | 53 | 78.09(±49.13) | 74.66 | ||
| Waist circumference | ||||||||
| Recommended | 36 | 0.704(±0.065) | 0.708 | 0.510 | 41 | 51.41(±39.61) | 37.26 | 0.007** |
| Above recommended | 30 | 0.718(±0.050) | 0.731 | 38 | 80.59(±49.80) | 75.28 | ||
| Allergy | ||||||||
| No allergy | 27 | 0.704(±0.063) | 0.700 | 0.790 | 30 | 57.97(±41.40) | 45.07 | 0.030* |
| Mono-sensitised | 9 | 0.724(±0.045) | 0.734 | 11 | 103.28(±50.91) | 107.15 | ||
| Poly-sensitised | 28 | 0.711(±0.061) | 0.725 | 36 | 62.06(±46.22) | 54.74 | ||
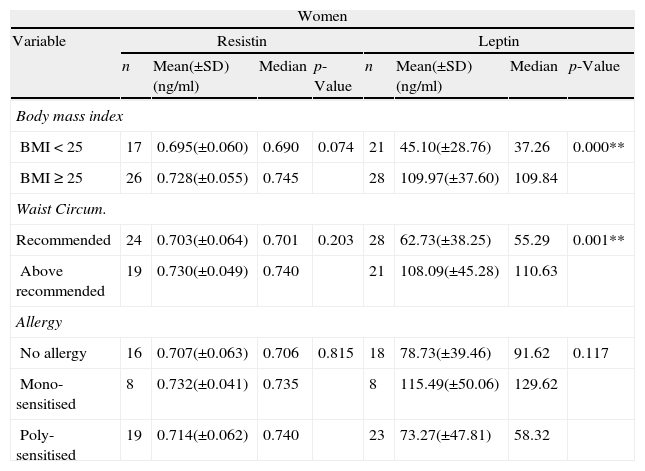
When we analyzed all population considering only BMI or waist circumference, as expected, the group of people with BMI≥25kg/m2 and the group with waist circumference values above recommended (over 80cm for women and over 94cm for men), had significantly higher levels of serum leptin (Table 1) and these differences were even stronger for women population (Table 2).
Comparison of leptin and resistin serum concentrations within selected variables considering only women. Non-parametric tests, Kruskal–Wallis and Mann–Whitney, were used to compare the concentrations between groups and the p≤0.05 was considered significant (*) and p≤0.01 strongly significant (**).
| Women | ||||||||
| Variable | Resistin | Leptin | ||||||
| n | Mean(±SD)(ng/ml) | Median | p-Value | n | Mean(±SD)(ng/ml) | Median | p-Value | |
| Body mass index | ||||||||
| BMI<25 | 17 | 0.695(±0.060) | 0.690 | 0.074 | 21 | 45.10(±28.76) | 37.26 | 0.000** |
| BMI≥25 | 26 | 0.728(±0.055) | 0.745 | 28 | 109.97(±37.60) | 109.84 | ||
| Waist Circum. | ||||||||
| Recommended | 24 | 0.703(±0.064) | 0.701 | 0.203 | 28 | 62.73(±38.25) | 55.29 | 0.001** |
| Above recommended | 19 | 0.730(±0.049) | 0.740 | 21 | 108.09(±45.28) | 110.63 | ||
| Allergy | ||||||||
| No allergy | 16 | 0.707(±0.063) | 0.706 | 0.815 | 18 | 78.73(±39.46) | 91.62 | 0.117 |
| Mono-sensitised | 8 | 0.732(±0.041) | 0.735 | 8 | 115.49(±50.06) | 129.62 | ||
| Poly-sensitised | 19 | 0.714(±0.062) | 0.740 | 23 | 73.27(±47.81) | 58.32 | ||
No association was found between hormone levels and allergy presence, but on dividing allergic patients into sub-groups of mono- and poly-sensitised, a significant difference was observed between the mono-sensitised and the other two groups (no allergy, poly-sensitised) in leptin concentration (Table 1).
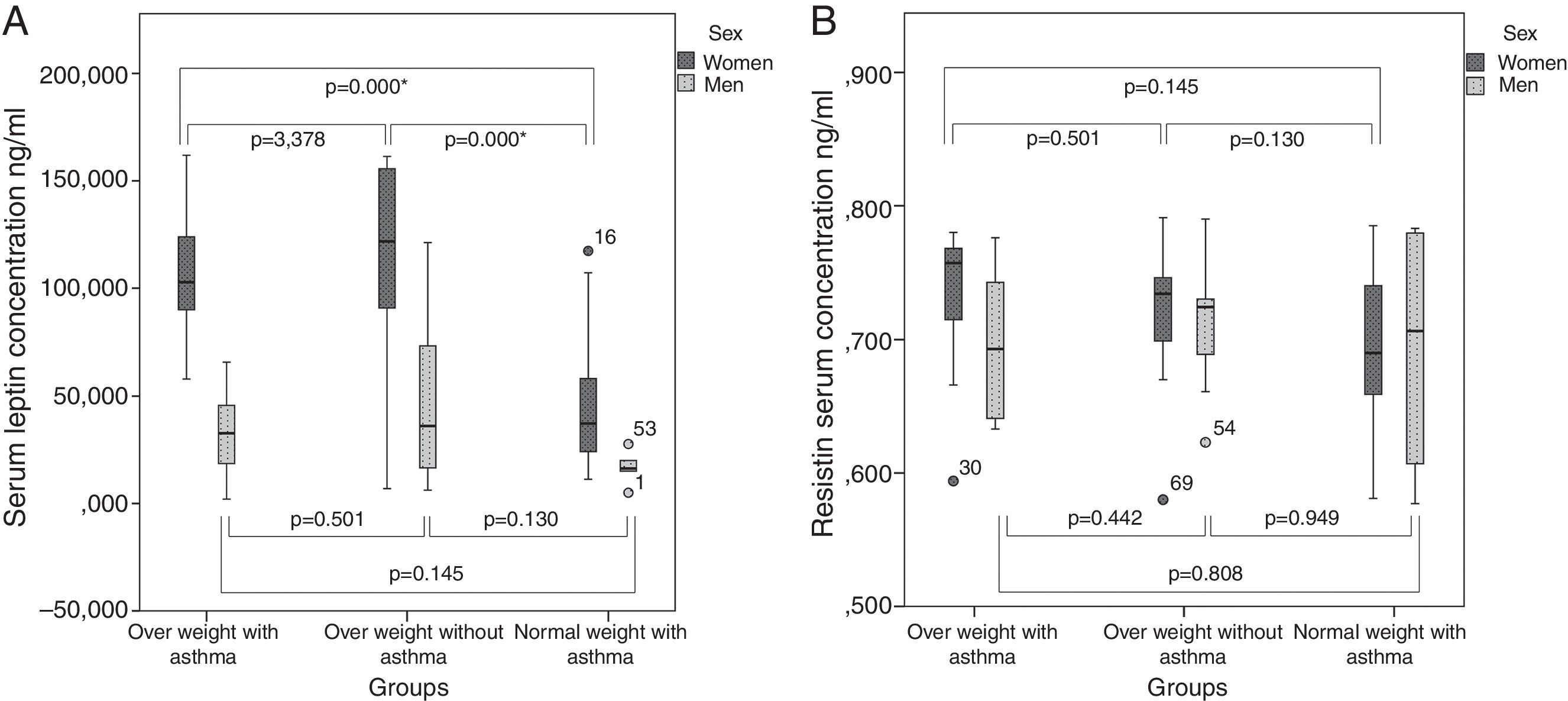
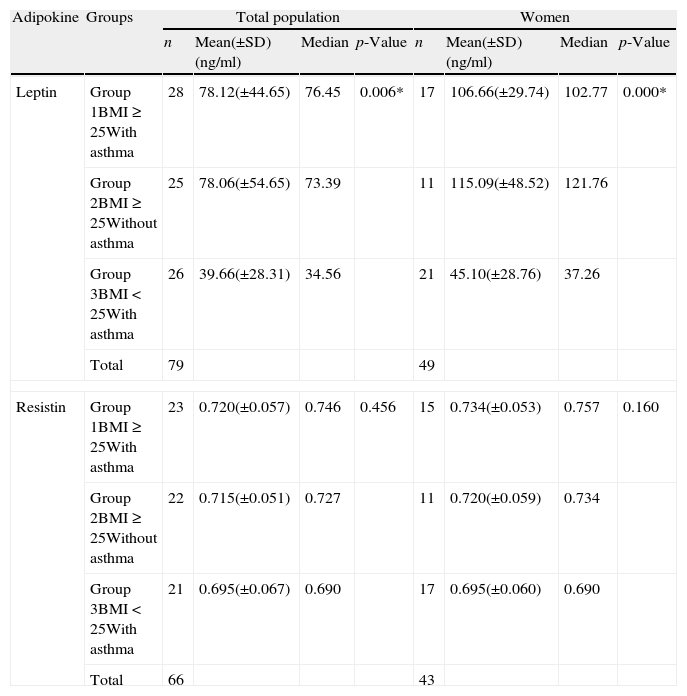
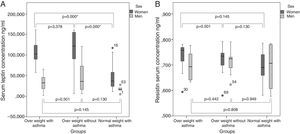
As we can see in Table 3 and Fig 1, when comparing the three groups of overweight patients with asthma (group 1), overweight patients without asthma (group 2) and individuals with normal weight and asthma (group 3), without division between sexes, a significant difference in serum leptin levels was found. However, as shown in Fig. 1, the results turned non-significant when comparing only the two groups of overweight patients with and without asthma. After the division between sexes, significant differences could be found also only between the groups 1 and 2, and groups 2 and 3. No significant difference between asthmatic and healthy overweight patients was observed.
Comparison of the leptin and resistin serum concentrations between the three studied groups. Non-parametric test, Kruskal–Wallis, was used to compare the concentrations between the groups. The p≤0.05 was considered significant (*) and p≤0.01 strongly significant (**).
| Adipokine | Groups | Total population | Women | ||||||
| n | Mean(±SD)(ng/ml) | Median | p-Value | n | Mean(±SD)(ng/ml) | Median | p-Value | ||
| Leptin | Group 1BMI≥25With asthma | 28 | 78.12(±44.65) | 76.45 | 0.006* | 17 | 106.66(±29.74) | 102.77 | 0.000* |
| Group 2BMI≥25Without asthma | 25 | 78.06(±54.65) | 73.39 | 11 | 115.09(±48.52) | 121.76 | |||
| Group 3BMI<25With asthma | 26 | 39.66(±28.31) | 34.56 | 21 | 45.10(±28.76) | 37.26 | |||
| Total | 79 | 49 | |||||||
| Resistin | Group 1BMI≥25With asthma | 23 | 0.720(±0.057) | 0.746 | 0.456 | 15 | 0.734(±0.053) | 0.757 | 0.160 |
| Group 2BMI≥25Without asthma | 22 | 0.715(±0.051) | 0.727 | 11 | 0.720(±0.059) | 0.734 | |||
| Group 3BMI<25With asthma | 21 | 0.695(±0.067) | 0.690 | 17 | 0.695(±0.060) | 0.690 | |||
| Total | 66 | 43 | |||||||
In case of resistin, for all the variables included, no significant associations were found neither in the total population nor within genders.
DiscussionAdipokines are the proteins secreted by the adipose tissue involved in the regulation of the energy balance with the recently suggested putative role in allergic inflammation increasing the risk of asthma in obese individuals.15 The association between adipokine concentration and asthma has been discovered to be even stronger in women.19 In our studies we analyzed two cytokines: leptin and resistin. As expected, patients with excess weight expressed a significantly increased level of leptin in serum. The difference was significant both for individuals with BMI equal to or over 25 and for those with waist circumference over 80cm for women and 94cm for men. A significantly increased level of adipokines in women as well as a stronger association between their concentrations and obesity resulted in creating a separate phenotype of obesity-related asthma that predominantly affects this sex. The difference in fat distribution between men and women is widely known. In women we can more frequently observe the physiological fat accumulation in the hip area (pear shape/gynoid pattern) while in men the abdominal area is the main storage part (apple shape/android pattern). However, this is not the only difference. Recent studies suggest that the difference is in fact not found in physiological fat, present in the adipose tissue, but in so-called ectopic fat. This fat is present in the viscera or muscles. Although men tend to have more visceral fat, it is more active in women. Muscular fat as well as physiological fat levels are higher for the female sex. In muscles, due to its visual aspect it is often said to create a “marbling” effect on the muscle tissue. The protein involved in the marbling of the muscle is leptin.19 These differences could be the underlying reason for the increased adipokine concentrations in women, that we also establish in our study.
When comparing the mean values of leptin concentrations between the three studied groups (overweight with asthma, overweight without asthma and normal weight with asthma) we can observe a significant difference (even stronger in women) which, however, is not evident when eliminating the normal weight group (Fig. 1). This suggests that the main factor determining the difference in leptin concentration is the excess of fat rather than presence of asthma. Similarly, no difference in leptin concentrations was also reported in a Korean study in children although it did show the negative correlations of this protein with pulmonary functions such as forced respiratory volume in 1 second and flow respiratory volume between 25 and 75%. In the same study significant concentration differences were found for resistin which was not the case in our work.22 As suggested in the article published by Sood et al., leptin levels might not be the link in the association between the obesity and asthma. Although in this work a significant association was found between BMI and leptin levels as well as the leptin levels and asthma in women, the associations turned out to be independent and the research did not confirm that leptin is in fact the link between the two diseases.23 This could also be the reason why in our study, the concentrations of leptin were significantly associated with BMI, but no difference was observed when comparing the asthmatic overweight group with the healthy overweight group. The lack of association could also be due to the fact of the BMI being a very general index for risks related to obesity, as it excludes influence of the fat distribution and type. BMI does not discriminate visceral nor intramuscular fat proportions, which seem to have much stronger association with the elevated risk of morbidities than physiological fat.
Not only asthma, but also an atopy was described to be linked with increased body mass. A positive correlation between levels of IgE and leptin was observed in atopic patients and obesity is considered a risk factor for allergies.24 In our population, allergic individuals had an increased level of both leptin and resistin but the difference was not significant. Interestingly, significantly higher levels were expressed in poly-sensitised patients compared to mono-sensitised and non-allergic patients.
ConclusionsSummarizing, the results of the presented work indicate a modification in the systemic levels of leptin, a protein produced predominantly by adipocytes, in overweight (including obese) patients with the association being stronger for women. No significant difference was found between the group of overweight asthmatics and overweight non-asthmatic patients. Our study suggests that the observed differences in concentrations, especially for leptin, can strengthen the inflammatory response of airways and contribute to the severity of asthma in obese individuals, but in the future research, apart from the physiological fat tissue, role visceral and intramuscular fat should be included in the analysis.
Previous presentation of resultsPart of the results has been previously presented in the form of posters (EAACI Summit on Asthma Severity and Exacerbations, 2nd PF2MUC Symposium – Changing Paradigms of Science Faculty of Medicine of University of Coimbra), and oral presentation with abstract (International Conference “Advances in Pneumology”, in Conference Proceedings http://pneumology.pl/index.php?id=program, Wroclaw).
Ethical disclosuresPatients’ data protectionConfidentiality of Data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
FundingAll serum samples and database information (subject clinical information) originated from the GA2LEN initiative project. The work was developed and financed by the Faculty of Medicine of the University of Coimbra.
Conflict of interestNone declared.
We thank Filipa Ângelo, Leonor Salguinho and Lidia Silvia for the technical help in the research process and all the patients who agreed to participate in the study.