Oral mite anaphylaxis (OMA), also known as the pancake syndrome, is characterised by severe acute allergic symptoms triggered by the ingestion of mite-contaminated foods. More frequently, clinical manifestations include breathlessness, angio-oedema, wheezing, rhinorrhoea, cough, stridor, and dysphagia.1 In this paper we report the case of a patient with OMA who was admitted to the hospital with an initial diagnosis of acute asthma.
A 10-year-old boy was brought to the ER presenting dyspnoea, intense cough, and wheezing which began approximately two hours after eating a homemade sponge cake. Physical examination disclosed acute respiratory distress with nasal flaring, intercostal retractions, generalised pallor, cyanosis, expiratory wheezing rales, and hyaline rhinorrhoea with postnasal drip. Respiratory rate was 32 per minute, pulse 112bpm, blood pressure 70/50mm Hg and oxygen saturation 81%. The diagnosis of an asthma exacerbation was made. Although the patient had a history of rhinitis, he had no previous history of past nocturnal wheezing, cough with exercise or laughter, asthma, wheezing or dyspnoea. Parents referred that the patient had experienced two episodes of facial (eyelid) angio-oedema after taking diclofenac or dipyrone.
Since treatment with nebulised fenoterol/ipratropium bromide given four times at 10-min intervals did not result in significant clinical improvement, the patient was transferred to the ICU where oxygen, inhaled salbutamol and budesonide, iv methylprednisolone and ranitidine administration induced a remission of the symptoms after 24h.
Due to the absence of previous asthma, and the initiation of the symptoms after ingesting a cake made with wheat flour, the possibility of OMA was entertained. Microscopic examination of the flour used to prepare the food revealed the presence of mites in a quantity of 2500 mites per gram of flour, of the species Aleuroglyphus ovatus (Fig. 1). Levels of Der p1, Der f1 and group 2 allergens in the flour were 0.059, 0.014 and 0.046 micrograms per gram of flour, respectively. These low Group 1 and Group 2 allergen levels are likely due to the absence of Dermatophagoides spp. mites in the incriminated flour.
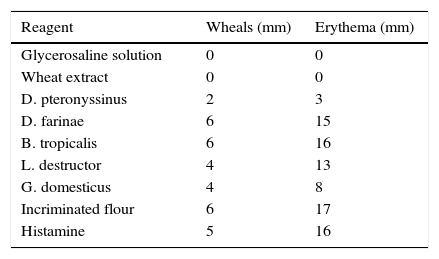
Skin prick tests were conducted one week later, after discontinuation of antihistamines, with wheat and mite extracts (Inmunotek, Madrid, Spain) and a 1:20 w/v extract of the patient's flour. Results of the skin prick tests are shown in Table 1.
OMA is being increasingly reported from various areas of the world, especially in tropical countries.1–3 It may be observed at any age, including childhood.4 The patient described in this report was diagnosed at the time of hospitalisation as having acute asthma. However, since no previous record of asthma was present, other diagnostic possibilities were considered. The diagnosis of OMA was based on the following findings: (1) Acute respiratory symptoms temporarily associated with the ingestion of food prepared with flour. (2) Mite sensitisation demonstrated by positive prick tests to mite extracts. (3) Negative skin test with commercial wheat extract. (4) Positive prick test to the incriminated flour. (5) Microscopic identification of mites in the flour.
Interestingly, the clinical manifestations present in this patient were exclusively respiratory, and no angio-oedema, laryngeal oedema, urticaria, or gastrointestinal symptoms were observed. For this reason, a diagnosis of asthmatic crisis was initially proposed. In previous OMA studies dyspnoea (generally related to upper respiratory tract angio-oedema) was present in approximately 90% of the cases and wheezing in about 40%. Additionally, this patient had a previous history of angio-oedema episodes triggered by at least two NSAIDs. NSAID hypersensitivity has been frequently observed in patients who develop OMA (the New ASA Triad).5
In conclusion, we present the case of a young patient without a previous clinical history of asthma who developed OMA, showing a clinical picture resembling acute asthma. The clinical implications of this report are: (1) OMA could be included in the differential diagnosis of acute asthma in patients with, or without a previous history of asthma. (2) Oral allergy syndrome has been previously reported from oral exposure to pollens or fruits in sensitised patients.6 However, the triggering of asthma-like symptoms by oral exposure to aeroallergens is rarely described in the medical literature. Therefore, we propose that the ingestion of mite allergens can induce acute bronchial obstruction simulating asthma.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human and animal subjectsThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.