Allergic disorders are the chronic diseases of greatest pediatric morbidity, affecting over 25% of the pediatric population. Indeed, this situation has been referred to as an “allergic epidemic”. In comparison with asthma, atopic dermatitis and allergic rhinitis have been less extensively investigated, although this does not mean that they should be regarded as minor disorders but rather as alterations that affect the quality of life of the patients and their families, which generate considerable direct and indirect costs.
Despite an important research effort, the reason for this allergic epidemic is not well known. These are multifactor disorders without a single causal agent, in which the most important component is the genetic predisposition of the patient (atopy), modulated by environmental factors, exposure to allergens, infections and irritants, among others. A confounding element is the fact that the concept of allergic diseases encompasses phenotypes of rhinitis, atopic dermatitis or asthma in which no IgE-mediated atopic mechanism is demonstrated, and which can manifest in a way similar to true allergic phenotypes. Differentiation between the two is difficult to establish on the basis of self-administered questionnaires alone, in the absence of a precise etiological diagnosis.
The present article reviews the numerous factors suggested to be responsible for the increase in allergic diseases recorded in the last few decades, and for the differences in prevalence observed among centres. For most of these factors the results published in the literature are contradictory, in some cases due to a lack of control of the associated interacting or confounding factors. Consensus exists for only some of these causal factors, such as the established parallelism between the increase in allergic diseases and the reduction in infectious processes on one hand, and the increase in particles generated by diesel fuel combustion on the other.
In addition, the implicated factors could act differently (and in some cases even antagonically) upon atopy and on the different disease phenotypes, thereby complicating the study of these interactions even further.
The prevalence of allergic diseases has increased considerably in the last 30–40years, and in the industrialized world it is estimated that over 25 % of all children have some form of allergic problem. Specifically, atopic dermatitis and allergic rhinitis are diseases that typically develop in childhood and should not be regarded as minor disorders but rather as chronic diseases that cause very unpleasant symptoms and affect the quality of life of the patients and their families. In addition, these illnesses generate important costs both directly (consumption of health care resources and drugs) and indirectly (reduction in parent work yield).
Epidemiological studies have revealed important differences in the prevalence of allergic disorders among different countries, and even within single countries, as well as contradictory results in relation to the possible associated risk or protective factors. However, variability in the methodology used may influence the observed differences, thereby complicating comparisons among studies and the drawing of conclusions.
The ISAAC (International Study of Asthma and Allergies in Childhood) was created in 1991 with the aim of establishing and comparing the prevalence of allergic disorders in childhood and adolescence in different countries, and to explore their trend over time, thanks to the adoption of standardized methodology. For this purpose, the study used a questionnaire comprising simple questions in an attempt to homogenize the diagnostic criteria in the different parts of the world, thereby preventing the reported differences in prevalence from being attributable to methodological differences. Up until that time there were few multinational epidemiological studies on pediatric allergic diseases, and most were referred to asthma. The studies focusing on atopic dermatitis and rhinitis were practically anecdotal, though the idea that asthma and rhinitis are closely related is now gaining strength.
PREVALENCE OF ALLERGIC DISEASESAlthough the prevalence of allergic diseases is growing throughout the world, there are marked inter-regional differences, thus pointing to the influence of environmental factors upon the development of allergic disease. Phase 1 of the ISAAC study1 reported worldwide rates of rhinoconjunctivitis in the range of 1.4-39.7 % in adolescents of 13-14years or age, and between 0.8-14.9 % in children aged 6-7years. With regard to atopic dermatitis, these figures range from 2-16% in children between 6-7years of age, and from 1-17 % in those between 13-14years of age. In Spain, the prevalence of allergic rhinitis and atopic dermatitis in schoolchildren aged 13-14years in Cartagena was found to be 17.5 % and 6.3 %, respectively.2
INCREASE IN PREVALENCE OF ALLERGIC DISEASESIn the last few decades the increase in such diseases, particularly in the developed parts of the world, has been so notorious that the phenomenon has been referred to as an “allergic epidemic”. Studies have shown this increase to be genuine, and not attributable to the fact of diagnosing a larger number of cases as a result of improved knowledge of allergic disorders among both physicians and the general population.3,4 The high prevalence of reported allergic diseases in children of parents without a family history of atopy suggests that much of the prevalence increase in allergic disorders is occurring in children without a significant genetic predisposition.
The starting point and causes of this increase are not fully clear, and different hypotheses have been proposed to explain the situation. Most of these hypotheses are related to changes in lifestyle and to environmental and domestic factors that interact with the immune system in the early stages of life. The increase in the cases diagnosed in industrialized countries appears to occur at the expense of allergic phenotypes, since a parallel increase has been recorded in positive skin tests.5 This is not extrapolatable to the developing world, where a high prevalence of respiratory symptoms is observed, although these situations correspond to non-allergic phenotypes characterized by earlier and more severe alterations, associated with crowded living conditions and early exposure to environmental pollutants.6
In the last few years a number of studies have reported a certain slowing in the increase in prevalence of allergic diseases.7,8 However, rather than a case of true deceleration, this situation may reflect a lesser reporting of symptoms due to the availability of more effective treatments.9
THE HYGIENE THEORYIn 1989, Strachan10 observed that atopy predominates among first offspring and single children, and for the first time suggested that this may be due to a lack of immune system maturation stimulus on the part of certain infections.
Physiologically, intrauterine life is characterized by important Th2 cell polarization, with intense expression of cytokines (IL-4, IL-10, leukaemia inhibiting factor), the function of which is to counter Th1 responses that are toxic for the placenta.11 It has been seen that atopic mothers suffer fewer miscarriages and have a larger number of pregnancies,12 with a greater frequency of deliveries to term, and without complications. In contrast, the placentas of women who suffer spontaneous miscarriages show lesser Th2 cytokine expression.14 After birth, and as a result of microbial stimulation (pathogenic or saprophytic), a shift occurs from Th2 responses towards Th1 responses, which in turn consolidate through successive exposures to the microbial antigens – thereby protecting the host against the germs and avoiding the Th2 reactivity that leads to allergic processes.
The hygiene theory postulates that the increase in the prevalence of allergic diseases is linked to a decrease in exposure to germs. In this sense, a more adequate term could be “microbial reduction hypothesis”. Allergy thus would be the price to pay for reducing morbidity-mortality, particularly in children, by curbing or eliminating infections such as measles, hepatitis A or tuberculosis, which have dropped in both industrialized15 and developing countries.16 In this sense, the hygiene theory appears to be related to the increase in atopy (understood as sensitization) and allergic phenotypes in the developed world, but would not explain the increase in the prevalence of respiratory diseases in developing countries –where certain purported protective factors in the industrialized world (e.g., respiratory or gastrointestinal infections in early life) are not applicable.
THE GENETICS OF ALLERGIC DISEASESDespite important research efforts, the etiology of allergic diseases is not well known. These are multifactorial disorders without a single causal agent, in which the most important component is the genetic predisposition of the patient (atopy), modulated by environmental factors, exposure to allergens, infections and irritants, among others.
Atopy is the most important risk factor for the development of allergic disorders. In effect, the risk of allergy in atopic individuals is between 10 and 20 times greater than in non-atopic subjects. It is moreover estimated that the risk of developing allergy is 25–35 % in the presence of an atopic sibling, between 30–50 % if one or both parents are atopic, and 70 % if both parents have the same allergic disease.17 The difficulty posed by genetic studies is represented by the numerous atopy markers involved, and the fact that atopy and allergic diseases are not always jointly inherited. Some genetic markers have been shown to be linked to bronchial hyperreactivity (chromosome 4), total IgE and eosinophilia (chromosome 6), and bronchial hyperreactivity, total IgE and eosinophilia (chromosome 7), among other phenotypes. In a recent review, Cookson describes the genes and genetic loci that are associated with increased susceptibility to asthma and atopic dermatitis.18 It is of great interest that genetic loci linked to eczema and asthma are not shared, suggesting that the risk of suffering these two diseases is mediated by different genes, rather than related through a common atopic susceptibility.
FRACTION ATTRIBUTABLE TO ATOPYIn the same way that some subjects suffer asthma, rhinitis or atopic dermatitis in the absence of atopy (i.e., without allergic sensitization), other individuals present sensitization (positive testing for allergens) but suffer no disease as such. These situations correspond to subclinical or asymptomatic sensitization.
In order to calculate the degree to which allergic disease is attributable to atopy, Pearce et al.19 conducted a meta-analysis of articles describing the relationship between asthma and atopy. The authors concluded that the percentage of asthma cases (children and adults) attributable to atopy is between 30-40 %. Posteriorly, Arshad et al.20 confirmed these results not only for asthma, but also for rhinitis and eczema –proposing a model of allergic diseases for children at the age of four in which 30-40 % of all cases are attributable to atopy and the remaining 60-70 % to other factors. In this model, atopic dermatitis could be regarded as the least atopic of the allergic diseases (with intervention of a dual type I and type IV hypersensitivity mechanism), while asthma and rhinitis disorders – that are intimately related –would have a greater atopic component.
The fraction of allergic diseases attributable to atopy is calculated by means of the formula P(R-1)/R, where R is the relative risk of suffering a given allergic disease in sensitized individuals, and P is the proportion of atopy in the patients with such allergic disease. However, it must be pointed out that this fraction depends on percentage sensitization among patients with a given allergic disease, and this in turn depends on factors such as the number and quality of allergenic extracts used, and the age of the patient when establishing the allergic diagnosis. Another point to be taken into consideration is that other pathogenic elements derived from the Th2/Th1 imbalance (distinct from IgE) cannot be measured by prick tests or the determination of specific IgE, and are therefore not represented in this formula.
ATOPY AS AN EVOLUTIVE BENEFITThe immune system of the atopic individual shows an exaggerated response, producing IgE against substances that are harmless for the rest of the population, and causing deleterious consequences. For this reason, in theory there are no biological or evolutive reasons for the existence of allergic diseases, since the latter afford no advantage for those who suffer them. However, some authors have suggested that such disorders could constitute an evolutive advantage by favouring survival among those who suffer them,21 and protecting them against most types of cancer,22 although another recent study has reported no association between allergy and cancer.23
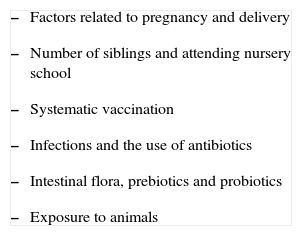
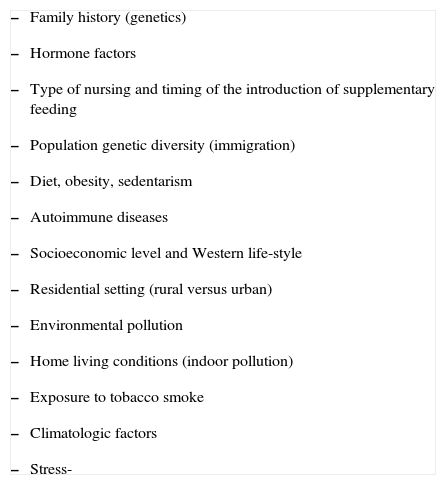
FACTORS ASSOCIATED TO RHINITIS AND ATOPIC DERMATITISMany investigations, mostly referred to asthma, have attempted to associate the increase in allergic processes to environmental pollution and to changes in population habits of hygiene, diet and life-style (sedentarism, the generalization of antibiotic use, poorly ventilated living spaces), among other factors, which in practical terms could be summarized in the form of two large groups: 1) factors related to the decrease in microbial burden; and 2) other factors unrelated to the latter (Tables I and II).
"Non-microbial" factors associated to atopy and allergy
|
It has been reported that sex hormone levels during pregnancy can influence maturation of the foetal immune system, favouring the development of allergic diseases. The maternal estrogens produce increases in Th2 cytokine production,24 and an increased prevalence of allergic disorders has been reported in the offspring of women who have taken oral contraceptives prior to pregnancy.25,26 However, Maitra et al.27 in 2005, published a study in 5765 mother-offspring couples in which no association was found between the earliness of maternal menarche (associated with increased oestrogen levels) and the presence of asthma, eczema, pollinosis or atopy in the offspring at 7years of age.
The role of prenatal exposure to allergens and drugs in the development of atopic diseases has been studied. The evidence points to production in the newborn infant of a prenatal T-cell response against environmental antigens before actual exposure to them has taken place.28,29 In this sense, a reduction in the exposure to dust mites during pregnancy and early infancy has been associated with lesser rates of sensitization to acarids.30 Likewise, a dose-dependent association has been found between the use of paracetamol at the end of pregnancy and the presence of asthma, sensitization and high IgE titers in the preschool period of life.31,32 Likewise, an increased risk of asthma and eczema has been reported in the children of mothers who used antibiotics during pregnancy,33 though a review of 5 studies on this subject failed to confirm the latter observation.34
In addition, it has been suggested that the influx of immigrants in industrialized countries could contribute to the increase in the prevalence of allergic diseases in such countries, since the greater genetic heterogeneity of mixed-race couples causes women to over-express Th2 cytokines (IL-4, leukaemia inhibiting factor) during pregnancy, in order to avoid rejection of the foetal haplotype.35
On the other hand, attempts have been made to relate caesarean section to an increased predisposition towards sensitization to pneumoallergens and foods, due to the lack of colonization of the newborn infant with the birth canal flora,36,37 although this hypothesis is also controversial, and has not been supported by the findings of other studies.38,39
GenderIt has been described that in the pre-puberal stage, males show a greater prevalence of allergic sensitization,40,41 rhinitis, and asthma.40 This situation inverts in adolescence, with a greater frequency of these diseases in females42–44 (with the exception of atopic dermatitis, which is more common in females than in males at all ages). This observation can be explained in endocrine terms. In effect, estrogens are proinflammatory hormones, while the male steroids are immune suppressors.45 This hormonal and immunological dimorphism also appears to influence the greater prevalence of autoimmune diseases in women of child-bearing age46 who have been treated with tamoxifen (an anti-estrogen drug)47 and dehydroepiandrosterone.48 In the specific case of asthma, further consideration is required of functional and structural differences in the airways between sexes. In effect, boys are characterized by disynaptic lung growth (lung volume grows relatively more than the airways), while girls show a proportional growth up until adolescence, after which the caliber of the airways and lung function increases in males.49
BreastfeedingThe relationship between breastfeeding and its possible protective effect against the future development of allergic diseases is very controversial. Some publications report a preventive effect, while others document a partial effect (protection only in the first years of life, or only of certain subgroups), or even unfavourable effects. Ethical considerations make it very difficult to conduct randomized, double-blind placebo-controlled trials capable of clarifying this important point.
A meta-analysis of prospective studies showed that exclusive breastfeeding during at least the first four months of life is associated with a lesser rate of atopic dermatitis, and that the effect is more pronounced in children with a family history of atopy.50 Other studies suggest that breastfeeding prevents the appearance of allergic disorders in children without parental antecedents of allergy, although not in the subgroup with family atopy.51,52 However, this could be explained as a consequence rather than as a cause, i.e., these are children with family history of atopy whose allergic disease tends to develop earlier and is more severe and/or persistent, thus causing the mothers to prolong breastfeeding. This in turn is erroneously interpreted as representing an association between breastfeeding and allergic risk.
Systematic vaccinationThere is considerable controversy regarding the possible influence of vaccination in infancy upon allergic disease. Some studies have related systematic vaccination, particularly against whooping cough and measles, to the development of allergic diseases,53,54 as a result of the decrease in protective native infections and the development of IgE responses mediated by the vaccine itself. Bremner et al.55 found no association between DTP and MMR vaccination and an increased risk of allergic rhinitis, and conducted an analysis of possible confounding factors such as the fact that allergic children visit the physician more often and are more likely to receive their vaccines on time, while children with many siblings and recurrent viral infections (protective factors) can suffer delays in vaccination.
Koppen et al.56 in turn conducted a systematic literature review, selecting epidemiological studies that linked vaccination in infancy (DTP, MMR and BCG) to the development of allergic diseases. Quality and validity varied considerably among the reviewed studies, some of which did not take into account possible confounding variables such as life-style. The studies with the greatest scientific evidence reported that the analysed infant vaccinations did not increase the risk of developing allergic diseases, and that BCG vaccination appears to exert no protective effect upon the development of allergy –in contrast to the reports of other studies.57,58 In two recent studies carried out in The Netherlands, systematic infant vaccination was not associated with an increased risk of atopic disorders.59,60 According to Anderson et al.61, it is unlikely that the international discrepancies in the prevalence of allergic diseases can be ascribed to differences in immunization practices among countries.
Infections and antibiotic useRepeat infections of any location favour the production of cytokines that inhibit Th2 responses, such as IL-12, IL-18 and IFN-γ. Lowered levels of the latter are found in patients with asthma,62 rhinitis,63 and atopic dermatitis;64,65 as a result, it could serve as an in vitro marker of atopic disease.
A study involving 24,341 mother-offspring couples concluded that early infections do not protect against allergic disorders, although other indirect markers of microbial exposure (such as number of siblings, nursery attendance, living on farms or having pets in the home) were indeed found to be protective factors66 –thus suggesting that the concept of “microbial burden” is more important than the existence of specific infections as a protective factor in early childhood.67
In relation to the hygiene theory commented above, if contact with microorganisms protects against allergic diseases, then antibiotic use in infancy would have the opposite effect, i.e., it would constitute a risk factor for such diseases.68–70 This is a tempting interpretation, since the widespread and sometimes abusive use of antibiotics would partially explain the increase in the prevalence of allergic disorders seen in the last 3-4 decades. However, on analysing the studies on this subject, the association between allergic disorders and antibiotic use disappears when children that have received antibiotics for infections involving wheezing are included.34 Therefore, this association can be explained in inverse terms: asthmatic children (which may have associated rhinitis and/or eczema) show a greater risk of infections and these moreover generate more symptoms, as a result of which they are more likely to be treated with antibiotics.
Intestinal flora, probiotics and prebioticsEstablishment of the intestinal microflora is essential for correct modulation of immune system maturation in newborn infants.71 In this context there are differences between the composition of the intestinal microflora in allergic and non-allergic children, with a greater presence of Clostridium difficile,72 coliform species and S. aureus73 in allergic infants, and a predominance of Lactobacillus in non-allergic children.73 Differences have also been observed in the intestinal flora of children with an anthroposophic life-style that avoid the use of antibiotics, vaccines and antithermal drugs, and consume vegetables fermented with Lactobacillus. Such differences could contribute to the lesser rate of allergic diseases found in these children.74
In recent years, a number of groups of investigators have evaluated the benefits of probiotics administered in the last weeks of pregnancy and the first months of life as protection against allergic diseases.75–77 The problem here is posed by the choice of the most adequate probiotic germ, since the exact composition of the intestinal microbiota in healthy children is not known, though it must include properties such as resistance to the digestive enzymes, adhesion to the intestinal epithelium, competition with pathogens and the absence of antibiotic resistance transmission to the saprophytic flora. An alternative is to supplement infant foods with prebiotics (oligosaccharides that favour the development of beneficial saprophytic bacteria present in the intestine). There are promising results with the use of both types of products in atopic dermatitis, though the work carried out to date involves only small samples and with a short duration of follow-up.78,79
Number of siblings and nursery attendanceA lesser prevalence of rhinitis and asthma has been observed in children with many siblings80,81 or who attend the nursery from an early age.80,82,83 Karmaus et al. found that with each pregnancy, maternal tolerance of allergens increases, and the umbilical cord blood levels of IgE decrease, suggesting that this may be due to an in utero effect of the number of siblings.84,85
Exposure to animalsDomestic petsThere is considerable controversy over whether to have furry pets during infancy protects or favours the ulterior development of allergic diseases. It is believed that the effect of the pet depends on the age and degree of allergen exposure, as well as on the type of animal.86 In this context, while some studies have reported a protective effect,87–91 others consider exposure to pets to be a risk factor for sensitization92,93 and allergic diseases.94
These studies must be interpreted, however, with caution, however, since is it possible an inverse causal relation whereby families with a history of allergies would spontaneously apply preventive measures (e.g., avoiding pets or smoking in the home, or the prolongation of breastfeeding) that are not systematically adopted by families without such antecedents. In such situations it would be erroneous to attribute protective properties to the fact of having a pet in the home.
Farm animals. The importance of endotoxinsA number of studies have reported that early exposure to bacterial endotoxins from farm animals protects against allergic diseases,95–99 since such endotoxins are potent inducers of type Th1 cytokines. Paradoxically, however, exposure to endotoxins may induce IgE-mediated responses to allergens in subjects that have already developed allergic disease, thus constituting a risk factor for more serious symptoms in these cases.100
Exposure to tobacco smokeAnnesi-Maesano et al.,101 in french adolescents, reported the presence of asthma, rhinoconjunctivitis and eczema to be significantly associated with active smoking. The authors concluded that asthma or allergy status does not constitute a dissuading factor against starting to smoke or continuing to smoke in adolescence. On the other hand, the study of the effects of passive smoking in children is controversial, due to the difficulty of assessing the degree of exposure and of comparing studies with different methodological designs. In Trinidad-Tobago, a country where the benign climate causes children to stay little indoors (and thus with less exposure to tobacco smoke), Monteil et al. found passive exposure to tobacco smoke to be closely correlated to an increased prevalence of asthma and rhinitis in schoolchildren.102 Surprisingly, a Swedish study demonstrates an association between current exposure to tobacco smoke and a lower risk for atopic disorders, in smokers themselves and a similar trend in their children.103
Autoimmune diseasesBoth allergy and autoimmunity are the result of immune system dysregulation, with the predominance of Th2 action in the former and Th1 activity in the latter. A genome search has been made to establish a genetic link between both groups of diseases, with the identification of certain shared regions such as in the case of asthma with respect to ankylosing spondylitis, type 1 diabetes, multiple sclerosis and rheumatoid arthritis.104
A number of investigators have suggested that allergic diseases could protect against type 1 diabetes on the one hand,105,106 and that there are lower rates of atopic diseases among type 1 diabetics on the other.107,108 A meta-analysis published in 2003 confirmed a small but significantly lesser prevalence of asthma in these patients –although the same could not be concluded for the rest of atopic diseases.109
Socioeconomic level. Western life-styleStewart et al.110 found that countries with a gross domestic product in the lower quartile range present a significantly lesser positive response rate in the questionnaires on asthma, rhinitis and eczema in the ISAAC among adolescents in the 13-14years age range. This casts doubts as to the true role of the economic development of countries in relation to the presence of allergic diseases.
Conversely, it has been proposed that socioeconomic progress does not influence the development of allergic diseases, although such progress does improve the diagnosis and treatment of these disorders.111 Therefore, rather than socioeconomic status, associated factors such as smoking, the adoption of preventive measures,112 educational level,113 health care accessibility, language and cultural factors114 would be the true elements influencing the prevalence of these illnesses.
Environmental pollutionPollution is an important cause of respiratory symptoms in both atopic and non-atopic individuals. The degree of pollution, particularly that caused by combustion engines and produced in buildings, has been associated with the greater prevalence of allergic diseases in industrialized countries. The increase in these illnesses in recent decades has paralleled the replacement of coal with diesel fuel as an energy source –resulting in an important decrease in smog, but also in a change in the composition of the polluting particles, which presently originate mainly from the combustion of diesel fuel (70 %). The main mechanisms by which diesel exhaust fumes enhances allergic responses are the adsorption of aeroallergens –which ensures a greater concentration and permanence of such particles in the atmosphere –and a decrease in mucociliary activity with an increase in respiratory epithelial permeability to allergens, which thus gain easier access to the immune system.
A definitive study in this context compared the prevalence of pollinosis in children living in Munich and Leipzig before the reunification of Germany.115 Munich was a “non-polluted” city whose only sources of pollution were motor vehicles and buildings, while Leipzig was an intensely industrialized city with high levels of SO2 from factories that operated mainly with coal. Curiously, it was observed that both the presence of allergic rhinitis and the rate of positive prick tests were greater in Munich (18.2 % and 36.7 %, respectively) than in Leipzig (2.4 % and 8.6 %). Following the reunification of Germany, the obsolete coal burning facilities in Leipzig were eliminated, resulting in an apparently less contaminated city, although from that point onwards the incidence of pollinosis increased spectacularly. It can be concluded that diesel engines, which generates up to 150 times more particles than gasoline, constitute a main cause of the increase in allergic processes associated with the Western life-style.
Ozone is a colourless, scantly soluble and intensely irritating gas produced by photochemical reactions in the upper atmosphere. It is a direct oxidant that leads to the formation of free radicals and macromolecular damage, thus giving rise to nasal symptoms, bronchial hyper-responsiveness and airway inflammation. This in turn has been related to the rates of hospitalization due to respiratory problems in infants under two years of age.116
Rural versus urban settingAlthough pollen exposure is more intense in the rural setting, the prevalence of pollinosis is lower117 than in the urban setting118 –probably because of the lesser traffic pollution on one hand, and contact with farm animal endotoxins on the other.95,96
Differences are also seen in the rural setting. In effect, the prevalence of allergy to cedar tree pollen among Japanese living near highways practically triples the prevalence found in areas near cedar forests.119 Likewise, the prevalence of wheezing and atopic dermatitis is greater in adolescents that live less than 100 metres from main roadways.120
Diet, obesity and sedentarismAlthough the results have been controversial, the ingestion of antioxidants has been related to a lesser prevalence of asthma and other allergic disorders, while diets rich in monounsaturated fats have been associated with an increased risk of such diseases.121 The explanation for this is that these fats undergo peroxidation, with the consequent production of free radicals –as a result of which it is possible that the antioxidant needs are currently greater in industrialized countries than they were in the past. It must also be taken into account that individuals with more healthy eating habits may have other associated protective factors such as a higher socioeconomic level, a longer duration of breastfeeding, or less exposure to tobacco smoke, among other factors.
Some studies showed a consistent pattern of decreased symptoms of asthma, rhinoconjunctivitis and atopic eczema, associated with increased consumption of cereals, nuts, starch, and vegetables,122 and with Mediterranean diet (rich in monounsaturated fats, vegetables and fruits and moderate in milk).123
On the other hand, although a modest association has been found between obesity and asthma,123,124 due fundamentally to the effects of proinflammatory molecules such as leptin,125 no such relationship has been reported between obesity and atopy.124
StressStress is a risk factor for the development of allergy, by inducing alterations in the neuroimmune regulation mechanisms that modulate hypersensitivity response. These alterations occur at a number of levels such as the hypothalamus-hypophysis-adrenal system (with decreases in cortisol and increase in cytokines and inflammatory and immune-stimulating hormones), autonomous airway control (increasing of substance P), corticoid resistance, oxidative stress, and alterations in the intestinal flora, among others.126
In conclusion, it can be stated that there is great diversity in the results of the many studies of the risk factors associated with allergic diseases. After discarding the discrepancies attributable to methodological differences and/or deficiencies, it seems that the factors that exert a more relevant effect upon the atopic genotype causing the manifestation of allergic disease are: 1) the decrease in general microbial burden; and 2) the increase in environmental pollution to which the paediatric population has been exposed in the last few decades in different parts of the world.