Atopic dermatitis is a common allergic disorder. A multifactorial background for atopic dermatitis has been suggested, with genetic as well as environmental factors influencing disease development. Our aim was to estimate the prevalence rate and associated factors for atopic dermatitis in northern Croatia using the methods of the internationally standardised ISAAC protocol.
MethodsThe study was undertaken among 12–14-year-old schoolchildren. Data were collected using standardised ISAAC written questionnaire Phase One and some selected questions from the ISAAC supplementary questionnaire completed by parents.
ResultsA total of 2887 children participated in the study. Estimated lifetime (ever) prevalence rate of atopic dermatitis symptoms was 7.55% and estimated 12-month prevalence rate was 5.75%. The factors found to be associated to the symptoms of atopic dermatitis ever were: positive family atopy, female gender, sleeping on feather pillow and contact with pets after age of seven, and to the symptoms in the past 12 months were: positive family atopy, female gender, sleeping on feather pillow, parasite infestation, and contact with pets in the first year of life.
ConclusionsThe results of our study show that northern Croatia is a region with moderate prevalence rates of atopic dermatitis. Following risk factors were family atopy, female gender and sleeping on feather pillow. Because of controversial results of previous studies conducted on the same topic further investigations should be made.
Atopic dermatitis (AD) is a common and chronic inflammatory skin disease that is characterised by relapsing itch and eczema, beginning mostly in infants.1 AD belongs to the group of allergic disorders that includes food allergy, allergic rhinitis, and asthma.2 A multifactorial background for AD has been suggested, with genetic as well as environmental factors influencing disease development.3 Natural history of the clinical manifestations of AD varies with age; three stages can often be identified. In infancy (first phase), the eczematous lesions usually emerge on the cheeks and the scalp with scratching, which frequently starts a few weeks later, causing crusted erosions. During childhood (second phase), lesions involve flexures, the nape, and the dorsal aspects of the limbs, and in the third phase (in adolescence and adulthood) lichenified plaques affect the flexures, head, and neck.4
The prevalence rates and risk factors for AD have been the source of many studies including The International Study of Asthma and Allergies in Childhood (ISAAC). ISAAC was developed to ascertain the prevalence rate and risk factors of allergy diseases (asthma, allergic rhinitis and atopic dermatitis) with a standardised tool and methodology in different regions. A full description of the ISAAC study protocol was published previously.5
In the present study we evaluated the prevalence rate and associated factors for AD in northern Croatia using the methods of the internationally standardised ISAAC protocol.
Materials and methodsThe study was undertaken during the year 2005 among elementary school children in the Međimurje region in northwest Croatia. This region is located between the eastern Alps and the Panonic plain and is characterised by a rural environment. The climate is humid continental, with warm summers and cold winters. The target population was children aged 12 years 0 months to 14 years 11 months (6th–8th grades of school). Data were collected using standardised ISAAC written questionnaire Phase One and some selected questions from the ISAAC supplementary questionnaire, completed by parents. All standardised modules were translated from English to Croatian by physicians specialising in allergy,6 according to translation guidelines.7 The correctness of the questionnaire was tested by back-translation by an independent professional translator. Ethical approval was obtained from the local ethics committee before the start of the study. Any inconsistencies found were eliminated in a phone conversation with the parents. Data were then entered into a computer and analysed. Statistical analyses were performed using IBM SPSS Statistics version 19.0.0.1. Basic descriptive summaries of the data were obtained and differences between investigated groups were calculated with cross-tabulation and the chi-square test. Univariate and multivariate logistic regression analyses were used to depict risk factors for atopic dermatitis symptoms ever or in the past 12 months. Variables that could produce the multiple co-linearity problems were excluded from multivariate models (breastfeeding and pet ownership ever). A P<0.05 indicated a statistically significant difference.
ResultsParticipantsOf the 3298 children invited, completed standardised Phase One and supplementary ISAAC questionnaires were received from 2887 children (participation rate: 87.54%). Children participating in the study were from 27 randomly selected elementary schools (1497 [51.9%] girls; 12-year-olds: n=862, 13-year-olds: n=1017, 14-year-olds: n=1008).
Prevalence of atopic dermatitis symptomsEstimated lifetime (ever) prevalence rate of atopic dermatitis symptoms was 7.55% with a significantly higher rate in girls (9.01% vs. 5.97% in boys; OR: 1.561, 95%CI: 1.175–2.073, P=0.002). Estimated 12-month prevalence rate of atopic dermatitis symptoms was 5.75% with the same gender difference (girls: 7.08%, boys: 4.32%; OR: 1.689, 95%CI: 1.219–2.339, P=0.0016).
Results are shown in Table 1.
Prevalence of symptoms of atopic dermatitis calculated from the written questionnaire according to gender. Values P, OR, 95%CI according to female gender.
| Total N=2887 | Male N=1390 | Female N=1497 | P | OR | 95%CI | ||||
| N | % | N | % | N | % | ||||
| Itchy rash ever | 218 | 7.55 | 83 | 5.97 | 135 | 9.01 | 0.002 | 1.561 | 1.175–2.073 |
| Itchy rash in the past year | 166 | 5.75 | 60 | 4.32 | 106 | 7.08 | 0.0016 | 1.689 | 1.219–2.339 |
| Involvement of the predilection areas | 124 | 4.29 | 46 | 3.31 | 78 | 5.21 | 0.012 | 1.606 | 1.107–2.329 |
| Itchy rash cleared in the past year | 132 | 4.57 | 49 | 3.53 | 83 | 5.54 | 0.010 | 1.606 | 1.119–2.305 |
| Waking due to itchy rash | 57 | 1.97 | 22 | 1.58 | 35 | 2.34 | 0.148 | 1.489 | 0.869–2.550 |
| Confirmed atopic eczema ever | 335 | 11.60 | 140 | 10.07 | 195 | 13.03 | 0.014 | 1.337 | 1.062–1.684 |
Confirmed lifetime eczema was reported in 11.60% of the children, with the same gender difference (girls: 13.03%, boys: 10.07%; OR: 1.337, 95%CI: 1.062–1.684, P=0.014).
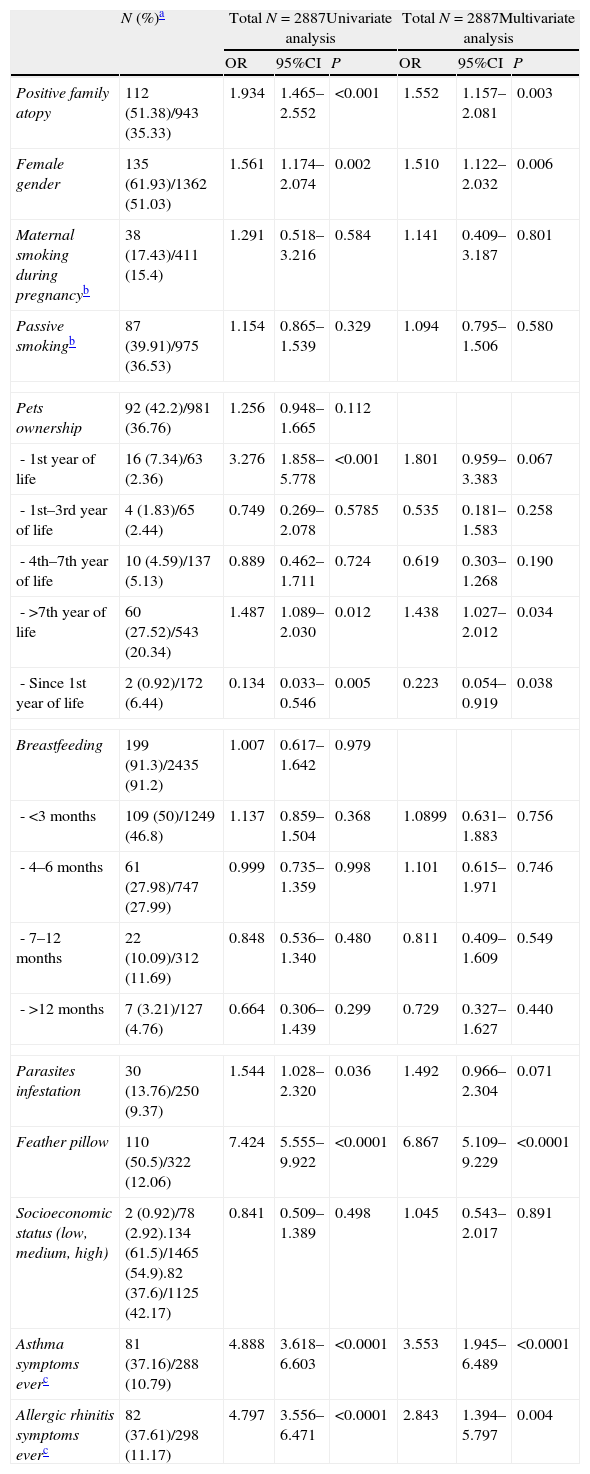
The main factors significantly associated to atopic dermatitis symptoms ever found in the univariate analysis, using the chi-squared test, were the following: positive family atopy (OR 1.934, 95%CI: 1.465–2.552, P<0.001), female gender (OR: 1.561, 95%CI: 1.174–2.074, P=0.002), sleeping on feather pillow (OR 7.424, 95%CI: 5.555–9.922, P<0.001), parasite infestation (OR 1.544, 95%CI: 1.028–2.320, P=0.036), contact with pets in the first year of life (OR 3.276, 95%CI: 1.858–5.778, P<0.0001), and after the age of seven (OR 1.487, 95%CI: 1.089–2.030, P=0.012). Children in contact with pets since the first year of life had fewer symptoms of atopic dermatitis ever (OR 0.134, 95%CI: 0.033–0.546, P=0.005).
We did not observe any statistically significant relationship between atopic dermatitis and maternal smoking during pregnancy, passive smoking, breastfeeding, and socioeconomic status.
Following univariate analysis, multiple logistic regression analysis was made with all the variables. The factors found to be associated to the symptoms of atopic dermatitis ever in children were: positive family atopy (OR 1.552, 95%CI: 1.157–2.081, P=0.003), female gender (OR: 1.510, 95%CI: 1.122–2.032, P=0.006), sleeping on feather pillow (OR 6.867, 95%CI: 5.109–9.229, P<0.0001), and contact with pets after the age of seven (OR 1.438, 95%CI: 1.027–2.012, P=0.034). Children in contact with pets since the first year of life had fewer symptoms of atopic dermatitis ever (OR 0.223, 95%CI: 0.054–0.919, P=0.038).
We found that children with symptoms of atopic dermatitis ever are at increased risk for developing other atopic disorders: asthma (OR 3.553, 95%CI: 1.945–6.489, P<0.0001) and allergic rhinitis ever (OR 2.843, 95%CI: 1.394–5.797, P=0.004).
We did not observe any statistically significant relationship between atopic dermatitis and parasite infestation, maternal smoking during pregnancy, passive smoking, breastfeeding, and socioeconomic status. Results are shown in Table 2.
Risk factors for symptoms of atopic dermatitis ever calculated from the written questionnaire.
| N (%)a | Total N=2887Univariate analysis | Total N=2887Multivariate analysis | |||||
| OR | 95%CI | P | OR | 95%CI | P | ||
| Positive family atopy | 112 (51.38)/943 (35.33) | 1.934 | 1.465–2.552 | <0.001 | 1.552 | 1.157–2.081 | 0.003 |
| Female gender | 135 (61.93)/1362 (51.03) | 1.561 | 1.174–2.074 | 0.002 | 1.510 | 1.122–2.032 | 0.006 |
| Maternal smoking during pregnancyb | 38 (17.43)/411 (15.4) | 1.291 | 0.518–3.216 | 0.584 | 1.141 | 0.409–3.187 | 0.801 |
| Passive smokingb | 87 (39.91)/975 (36.53) | 1.154 | 0.865–1.539 | 0.329 | 1.094 | 0.795–1.506 | 0.580 |
| Pets ownership | 92 (42.2)/981 (36.76) | 1.256 | 0.948–1.665 | 0.112 | |||
| - 1st year of life | 16 (7.34)/63 (2.36) | 3.276 | 1.858–5.778 | <0.001 | 1.801 | 0.959–3.383 | 0.067 |
| - 1st–3rd year of life | 4 (1.83)/65 (2.44) | 0.749 | 0.269–2.078 | 0.5785 | 0.535 | 0.181–1.583 | 0.258 |
| - 4th–7th year of life | 10 (4.59)/137 (5.13) | 0.889 | 0.462–1.711 | 0.724 | 0.619 | 0.303–1.268 | 0.190 |
| - >7th year of life | 60 (27.52)/543 (20.34) | 1.487 | 1.089–2.030 | 0.012 | 1.438 | 1.027–2.012 | 0.034 |
| - Since 1st year of life | 2 (0.92)/172 (6.44) | 0.134 | 0.033–0.546 | 0.005 | 0.223 | 0.054–0.919 | 0.038 |
| Breastfeeding | 199 (91.3)/2435 (91.2) | 1.007 | 0.617–1.642 | 0.979 | |||
| - <3 months | 109 (50)/1249 (46.8) | 1.137 | 0.859–1.504 | 0.368 | 1.0899 | 0.631–1.883 | 0.756 |
| - 4–6 months | 61 (27.98)/747 (27.99) | 0.999 | 0.735–1.359 | 0.998 | 1.101 | 0.615–1.971 | 0.746 |
| - 7–12 months | 22 (10.09)/312 (11.69) | 0.848 | 0.536–1.340 | 0.480 | 0.811 | 0.409–1.609 | 0.549 |
| - >12 months | 7 (3.21)/127 (4.76) | 0.664 | 0.306–1.439 | 0.299 | 0.729 | 0.327–1.627 | 0.440 |
| Parasites infestation | 30 (13.76)/250 (9.37) | 1.544 | 1.028–2.320 | 0.036 | 1.492 | 0.966–2.304 | 0.071 |
| Feather pillow | 110 (50.5)/322 (12.06) | 7.424 | 5.555–9.922 | <0.0001 | 6.867 | 5.109–9.229 | <0.0001 |
| Socioeconomic status (low, medium, high) | 2 (0.92)/78 (2.92).134 (61.5)/1465 (54.9).82 (37.6)/1125 (42.17) | 0.841 | 0.509–1.389 | 0.498 | 1.045 | 0.543–2.017 | 0.891 |
| Asthma symptoms everc | 81 (37.16)/288 (10.79) | 4.888 | 3.618–6.603 | <0.0001 | 3.553 | 1.945–6.489 | <0.0001 |
| Allergic rhinitis symptoms everc | 82 (37.61)/298 (11.17) | 4.797 | 3.556–6.471 | <0.0001 | 2.843 | 1.394–5.797 | 0.004 |
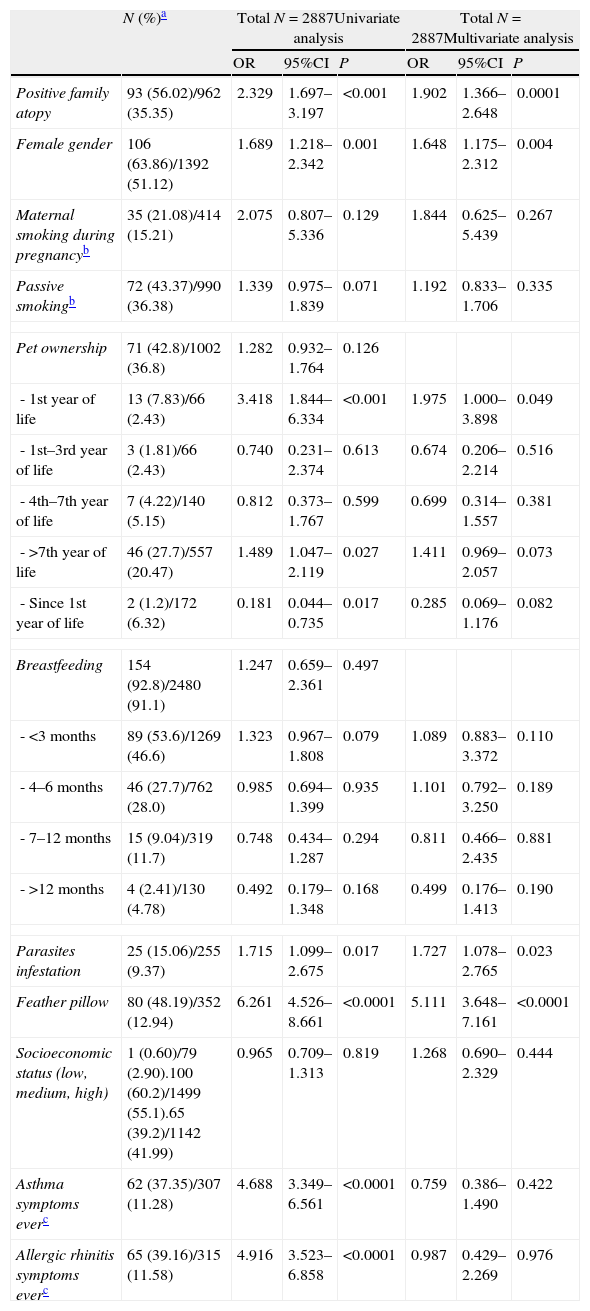
The main factors significantly associated to atopic dermatitis symptoms in the past 12 months found in the univariate analysis, using the chi-squared test, were the following: positive family atopy (OR: 2.329, 95%CI: 1.697–3.197, P<0.001), female gender (OR: 1.689, 95%CI: 1.218–2.342, P=0.001), sleeping on feather pillow (OR: 6.261, 95%CI: 4.526–8.661, P<0.0001), parasite infestation (OR 1.715, 95%CI: 1.099–2.675, P=0.017), contact with pets in the first year of life (OR 3.418, 95%CI: 1.844–6.334, P<0.001) and after the age of seven (OR 1.489, 95%CI: 1.047–2.119, P=0.027). Children who were in contact with pets since the first year of life had fewer symptoms of atopic dermatitis in the past 12 months (OR 0.181, 95%CI: 0.044–0.735, P=0.017).
We did not observe any statistically significant relationship between atopic dermatitis in the past 12 months and maternal smoking during pregnancy, passive smoking, breastfeeding, and socioeconomic status.
In multiple logistic regression analysis the factors found to be associated to the symptoms of atopic dermatitis in the past 12 months in children were: positive family atopy (OR 1.902, 95%CI: 1.366–2.648, P=0.0001), female gender (OR: 1.648, 95%CI: 1.175–2.312, P=0.004), sleeping on feather pillow (OR 5.111, 95%CI: 3.648–7.161, P<0.0001), parasite infestation (OR 1.727, 95%CI: 1.078–2.765, P=0.023) and contact with pets in the first year of life (OR 1.975, 95%CI: 1.000–3.898, P=0.049).
We did not observe any statistically significant relationship between atopic dermatitis symptoms in the past 12 months and maternal smoking during pregnancy, passive smoking, breastfeeding and socioeconomic status. Results are shown in Table 3.
Risk factors for symptoms of atopic dermatitis in the past 12 months calculated from the written questionnaire.
| N (%)a | Total N=2887Univariate analysis | Total N=2887Multivariate analysis | |||||
| OR | 95%CI | P | OR | 95%CI | P | ||
| Positive family atopy | 93 (56.02)/962 (35.35) | 2.329 | 1.697–3.197 | <0.001 | 1.902 | 1.366–2.648 | 0.0001 |
| Female gender | 106 (63.86)/1392 (51.12) | 1.689 | 1.218–2.342 | 0.001 | 1.648 | 1.175–2.312 | 0.004 |
| Maternal smoking during pregnancyb | 35 (21.08)/414 (15.21) | 2.075 | 0.807–5.336 | 0.129 | 1.844 | 0.625–5.439 | 0.267 |
| Passive smokingb | 72 (43.37)/990 (36.38) | 1.339 | 0.975–1.839 | 0.071 | 1.192 | 0.833–1.706 | 0.335 |
| Pet ownership | 71 (42.8)/1002 (36.8) | 1.282 | 0.932–1.764 | 0.126 | |||
| - 1st year of life | 13 (7.83)/66 (2.43) | 3.418 | 1.844–6.334 | <0.001 | 1.975 | 1.000–3.898 | 0.049 |
| - 1st–3rd year of life | 3 (1.81)/66 (2.43) | 0.740 | 0.231–2.374 | 0.613 | 0.674 | 0.206–2.214 | 0.516 |
| - 4th–7th year of life | 7 (4.22)/140 (5.15) | 0.812 | 0.373–1.767 | 0.599 | 0.699 | 0.314–1.557 | 0.381 |
| - >7th year of life | 46 (27.7)/557 (20.47) | 1.489 | 1.047–2.119 | 0.027 | 1.411 | 0.969–2.057 | 0.073 |
| - Since 1st year of life | 2 (1.2)/172 (6.32) | 0.181 | 0.044–0.735 | 0.017 | 0.285 | 0.069–1.176 | 0.082 |
| Breastfeeding | 154 (92.8)/2480 (91.1) | 1.247 | 0.659–2.361 | 0.497 | |||
| - <3 months | 89 (53.6)/1269 (46.6) | 1.323 | 0.967–1.808 | 0.079 | 1.089 | 0.883–3.372 | 0.110 |
| - 4–6 months | 46 (27.7)/762 (28.0) | 0.985 | 0.694–1.399 | 0.935 | 1.101 | 0.792–3.250 | 0.189 |
| - 7–12 months | 15 (9.04)/319 (11.7) | 0.748 | 0.434–1.287 | 0.294 | 0.811 | 0.466–2.435 | 0.881 |
| - >12 months | 4 (2.41)/130 (4.78) | 0.492 | 0.179–1.348 | 0.168 | 0.499 | 0.176–1.413 | 0.190 |
| Parasites infestation | 25 (15.06)/255 (9.37) | 1.715 | 1.099–2.675 | 0.017 | 1.727 | 1.078–2.765 | 0.023 |
| Feather pillow | 80 (48.19)/352 (12.94) | 6.261 | 4.526–8.661 | <0.0001 | 5.111 | 3.648–7.161 | <0.0001 |
| Socioeconomic status (low, medium, high) | 1 (0.60)/79 (2.90).100 (60.2)/1499 (55.1).65 (39.2)/1142 (41.99) | 0.965 | 0.709–1.313 | 0.819 | 1.268 | 0.690–2.329 | 0.444 |
| Asthma symptoms everc | 62 (37.35)/307 (11.28) | 4.688 | 3.349–6.561 | <0.0001 | 0.759 | 0.386–1.490 | 0.422 |
| Allergic rhinitis symptoms everc | 65 (39.16)/315 (11.58) | 4.916 | 3.523–6.858 | <0.0001 | 0.987 | 0.429–2.269 | 0.976 |
The present study was carried out using the ISAAC international methodology for the prevalence rates and risk factors for the development of atopic diseases.
Many prospective epidemiological studies show that the incidence of AD is growing and that the increase has been especially dramatic in the past 20–30 years.8 Data on AD symptoms show that this disease is common, with a large range of prevalence from less than 2% in Iran and China to around 20% in Australasia, England, and Scandinavia.9
This is the third study conducted in Croatia,10,11 based on the ISAAC protocol. When comparing our results with the results from other regions in Croatia using the same methodology and in the same age group, we found significantly lower prevalence (OR: 1.393, 95%CI: 1.058–1.833, P=0.018) compared with Zagreb.10 Compared with Primorsko-Goranska county,11 our prevalence was higher, but there were no significant differences found. This could be explained by different environmental factors. Zagreb and the Međimurje region are in the north of the country, with the same humid continental climate. Their difference is that the Međimurje region is a rural environment and Zagreb is an urban area. Primorsko-Goranska county belongs to the northern Adriatic region, which differs in climate, and vegetation. These regional differences should be considered and researched in further studies. Results from our study together with the results of other studies from Croatia show that Croatia is a country with a moderate prevalence of these symptoms.
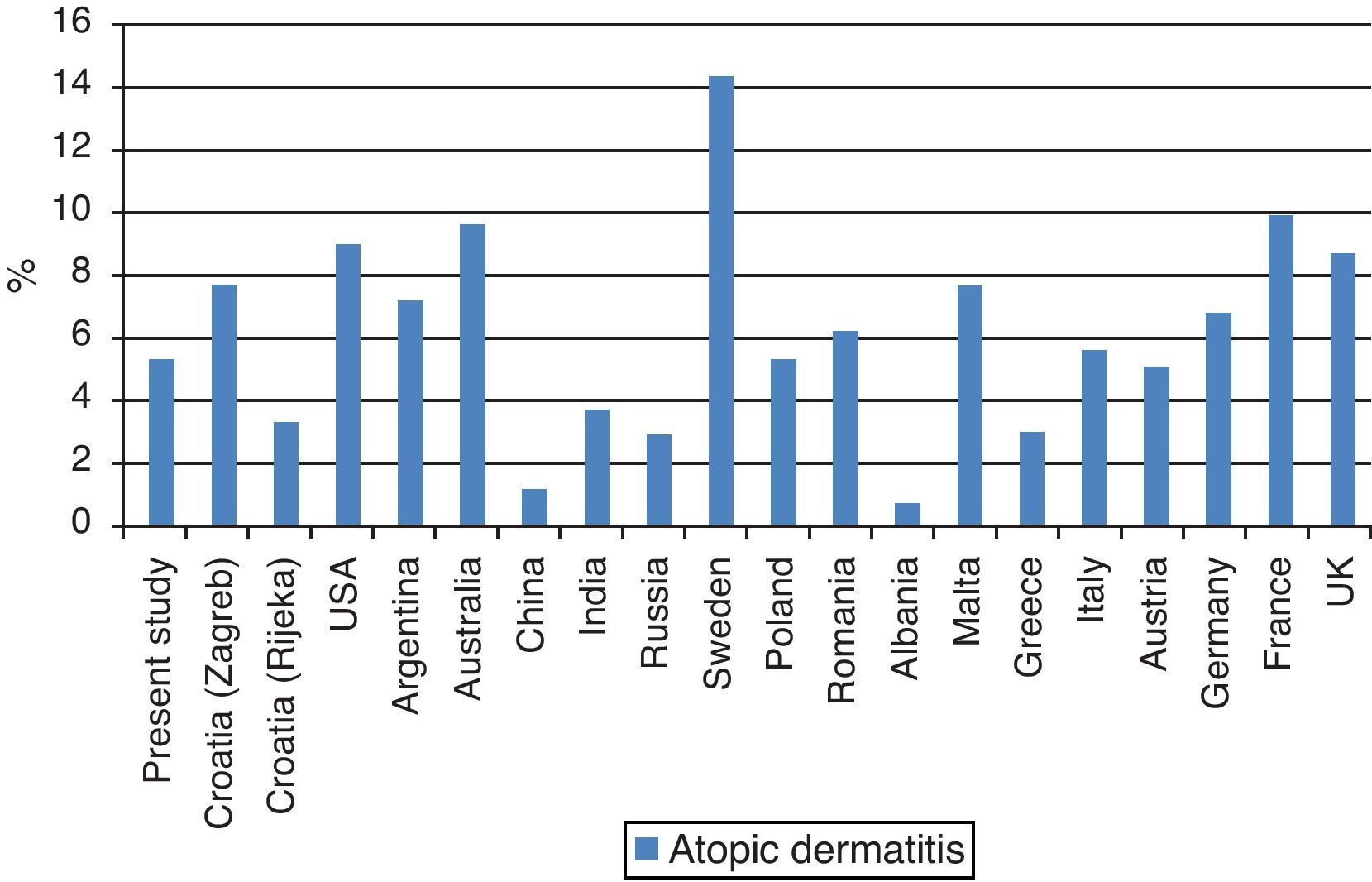
Comparing our results with the results from other European countries we can observe that the prevalence is lower than in Scandinavia, France and UK, and that it is in the same range with most of the nearby European countries (Germany, Italy, Austria). This could be explained by different environmental factors and genetic predisposition in different geographic areas. Comparison of our results with those from other studies is shown in Fig. 1.
Comparison of prevalence rates of symptoms of atopic dermatitis in the last 12 months reported in the present study and other studies in Croatia together with some ISAAC-participating countries based on the written questionnaire.9–11
In the majority of published epidemiological studies AD was more commonly diagnosed in girls than in boys.12 This tendency has also been confirmed in our study, and female gender increased the risk of AD by about 1.7-fold. Our results are consistent with the hypothesis that positive family atopy increases the risk of atopic dermatitis.13,14
In our study the most important risk factor for development of AD found is sleeping on feather pillow. Feather pillows accumulate a high concentration of dust,15 and children sleeping on them are more likely to be exposed to inhalation allergens like dust mites, which possibly leads to an increased risk for early sensitisation and development of AD.16
Early exposure to second-hand smoking has been shown to be associated with the development of AD.17–19 However, there are also studies showing no association between exposure to second-hand tobacco smoke and allergy diseases.20 In our study, exposure to maternal smoking during pregnancy and exposure to environmental tobacco smoke was not connected to the symptoms of atopic AD ever or in the past 12 months.
There have only been few studies looking directly at the association of AD with intestinal parasites, and most of them do not support a hypothesis of a protective effect of intestinal parasites in AD,21,22 which is contrary to the hypothesis of their protective effect in the development of other allergy diseases.23 Some parasites are associated, at least temporarily as they enter the body, with skin irritation, and this could be misclassified for symptoms of AD. This could be an explanation of the positive association of AD and parasites in our study.
Despite the number of studies, results about exposure to pets and development of AD are controversial.24,25 In our study exposure to pets in the first year of life increased the risk of the development of AD. Exposure to pets after the first year of age is more often in healthy population than in those with allergic symptoms. This could suggest a protective role of long-term animal exposure on development of AD or could be explained by selective avoidance of keeping pets in atopic children.
The protective effect of breastfeeding on the development of AD is also a controversial issue, with some studies showing a benefit and others no effect.26 We did not observe any effect of breastfeeding on development of AD.
Many studies show that socioeconomic status does not influence the development of allergy diseases, therefore associated factors would be the true elements influencing the prevalence of these diseases.27,28 In our study there was no correlation between symptoms of AD and level of socioeconomic status.
ConclusionsThe results of our study show that northern Croatia is a region with moderate prevalence of AD among schoolchildren. Compared with previous studies conducted in Croatia using the ISAAC protocol, results are in the same range. Compared with the results from other European countries we can observe that the prevalence is in the same range with most European countries (Germany, Italy, and Austria) which are placed closely geographically.
The following risk factors were family atopy, female gender and sleeping on feather pillow. Because of controversial results of previous studies conducted on the same topic, further investigations should be made.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflict of interestThe authors have no conflict of interest to declare.
The authors would like to thank all the teachers, parents, and children who participated in this study.