In adult asthmatics the incidence of gastro-oesophageal reflux disease (GERD) reportedly ranges from 34% to 89%. Oesophageal pH monitoring and endoscopy are not required in the patient with typical GERD symptoms before the initiation of a therapeutic trial. Diagnosis of GERD on the basis of history is the simplest and quickest method, placing no demand on patients. Recently, a new questionnaire (FSSG; Frequency Scale for the Symptoms of GERD) was produced to evaluate the severity and the therapeutic response of GERD. The FSSG (F-scale) was used to assess the GERD in subjects with persistent moderate to severe asthma treated with anti-inflammatory asthma medication. In the present study, 27.4% of the patients with asthma had symptoms suggestive of GERD. There is significant correlation between GERD symptom (F-scale score) and severity of cough and sputum. The observations suggested that reflux symptoms, not gastric dysmotility symptoms, significantly associated with severity of cough, not of sputum. It is the first such study to use a FSSG as incidence of GERD symptoms in asthmatics and examine the relationship between F-scale score and asthmatic symptoms.
Acid in the oesophagus may cause cough or bronchial asthma (BA) symptoms by reducing the cough sensitivity threshold.1 The prevalence of gastro-oesophageal reflux disease (GERD) among asthmatics is high, ranging from 34% to 89% in different studies.2–6 Most of the papers published in English have come from Western countries where GERD is highly prevalent. In East Asia, the prevalence of GERD is less common than in Western countries, but obviously has been increasing,7 and has recently become a common disease in Japan. However, severe oesophagitis is not common.8 A multitude of tests have been used to diagnose GERD in asthmatics including barium studies, upper endoscopy, pH monitoring and the acid perfusion test. Ambulatory 24-h pH testing is the gold standard for diagnosing GERD.9 These methods, however, place pressure on patients. Oesophageal pH monitoring and endoscopy are not required in the patient with typical GERD symptoms.10 An empiric trial of acid suppression using a PPI (PPI test) is a simple and potentially definitive method for diagnosing and assessing GERD.11 In addition, diagnosis by obtaining a history is the quickest and simplest method and it does not put stress on patients, making it the favoured method for general practitioners. A Questionnaire for the diagnosis of reflex disease (QUEST) was recently introduced and its usefulness for GERD diagnosis has been evaluated in Western countries.12 As a result, several problems with QUEST have been detected. It was not easy to complete the questionnaire and evaluate therapeutic response of GERD.13 The new questionnaire (FSSG; Frequency Scale for the Symptoms of GERD) was developed to evaluate the severity and the therapeutic response of GERD.14 The aim of this study was to determine the incidence of GERD symptoms, and revealed its association with respiratory symptoms in asthmatic patients by using the FSSG.
MethodsThe present study was performed between July and October 2005. We used an asthma questionnaire and the FSSG to obtain information on the impact of both asthma and GERD on everyday symptoms. The FSSG consisted of 12 questions, which were scored to indicate the frequency of symptoms as follows: never=0; occasionally=1; sometimes=2; often=3; and always=4 (Table 1). Patients with FSSG scores of more than 8 were considered as positive. The asthma questionnaire consisted of 4 questions (frequency of cough, sputum, attacks and short-acting β2-agonist use), which were scored to indicate the frequency of symptoms as follows: never=0; occasionally=1; sometimes=2; often=3; and always=4.
PPI therapy (PPI test) significantly decreased the FSSG score one month later
| 1. Do you get heartburn? |
| 2. Does your stomach get bloated? |
| 3. Does your stomach ever feel heavy after meals? |
| 4. Do you sometimes subconsciously rub your chest with your hand? |
| 5. Do you ever feel sick after meals? |
| 6. Do you get heartburn after meals? |
| 7. Do you have an unusual (e.g. burning) sensation in your throat? |
| 8. Do you feel full while eating meals? |
| 9. Do some things get stuck when you swallow? |
| 10. Do you get bitter liquid (acid) coming up into your throat? |
| 11. Do you burp a lot ? |
| 12. Do you get heartburn if you bend over? |
Each questionnaire was scored to indicate the frequency of symptoms, as follows: never=0; Occasionally=1; sometimes=2; often=3; and always=4.
Outpatients (n=113; male 45, female 68, with average age [age (yr)±SEM] of 55.89±2.89 and 56.53±1.94, respectively) with mild to severe asthma at the Oita University Hospital and associated hospitals, were surveyed. Patients with gastrointestinal disease other than GERD were excluded from this study. The characteristics of patients with asthma are summarised in Table 2. Of all the patients who regularly attended our hospital, 113 asthmatics answered the questionnaire and were interviewed at the site. As shown in Table 3, the questionnaire consisted of questions assessing asthma symptoms during the previous week and FSSG score at consultation.
The characteristics of patients with asthma
| Asthma patients (n=113: male 45, female 68) | |
| Atopy | |
| Atopic | 66.70% |
| Non-atopic | 27.20% |
| Unclassified | 6.10% |
| Age | Male 55.89±2.89 |
| Female 56.53±1.94 | |
| Stage | |
| I | 8.80% |
| II | 21.90% |
| III | 46.50% |
| IV | 12.30% |
| Unclassified | 10.50% |
| Complication | |
| Allergic rhinitis | 62.68% |
| Sinusitis | 11.50% |
| FSSG | |
| Positive | 27.40% |
| Positive+history of GERD | 31% |
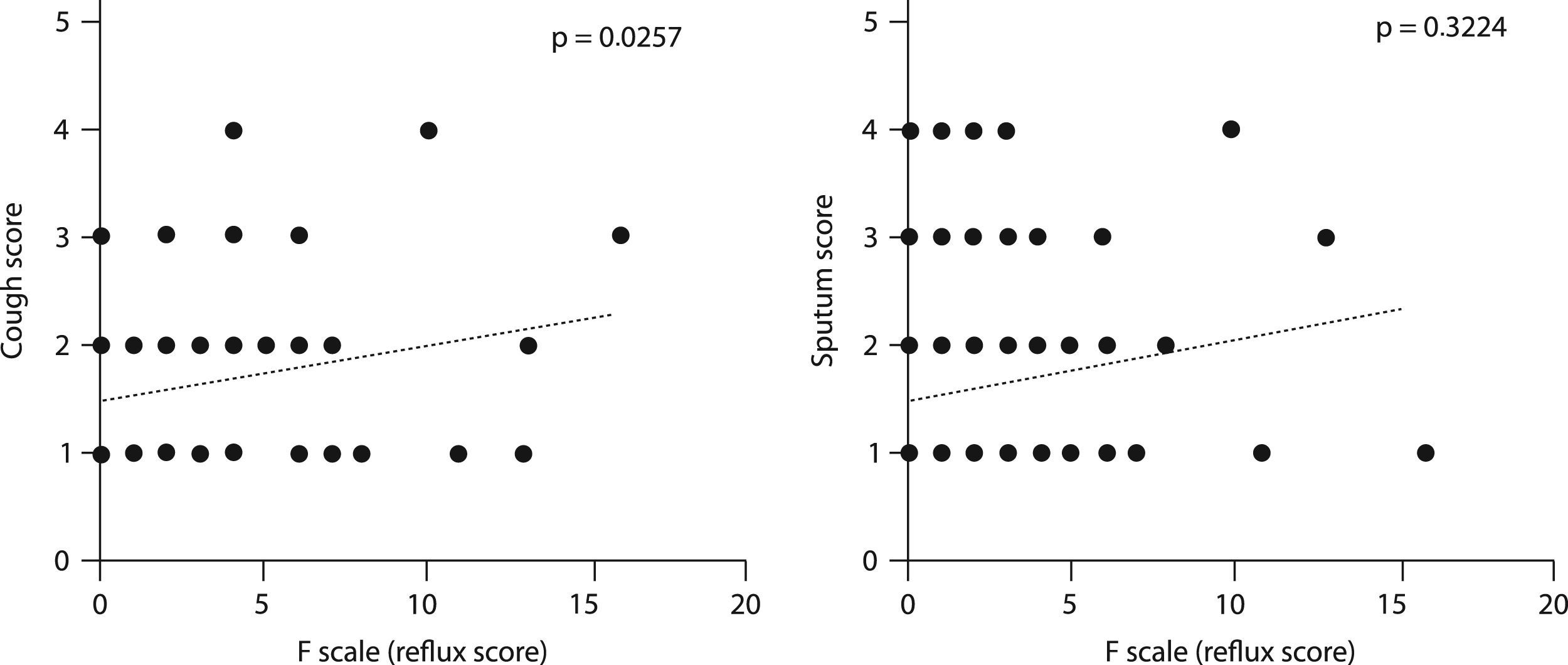
The reflux symptoms significantly correlated with cough score, not with sputum score
| 1. In the past 7 days, did you have any respiratory symptoms (cough, sputum)? |
| 2. In the past 7 days, did you have an attack of wheezing or use short-acting β-stimulant treatment for asthma? |
Each questionnaire was scored to indicate the frequency of symptoms, as follows: never=0; occasionally=1; sometimes=2; often=3; and always=4.
Histories of BA were ascertained in the following ways: (a) personal contact with patients to complete an initial questionnaire of their personal history of allergy, and (b) additional history obtained by personal interview of patients at the time of the consultation.
The following criteria were used to classify the specific allergy diagnosis: BA—a history of recurrent, reversible episodes of wheezing and dyspnoea not caused by any known organic condition. The diagnosis and severity of BA were classified according to the criteria of the Asthma Prevention and Management Guidelines (Japan Guidelines; JGL). Among the 113 subjects, 8.8% were stage I; 21.9% were stage II; 46.5% were stage III; 12.3% were stage IV; and 10.5% were unclassified (Table 2).
Seven FSSG-positive asthmatics (male 2, female 5) were assessed endoscopically. Endoscopy revealed mucosal injury of the oesophagus in two of them. The grading of GERD was classified according to the criteria of the Los Angeles classification of the endoscopic features of GERD15 which was modified by the addition of grade O (healed mucosal breaks),16 and grade M (minimal change).
The clinical usefulness of the FSSG was evaluated in 12 FSSG-positive asthmatic patients. These subjects were 4 males and 8 females who were treated with PPI (rabeprazole: 10mg/day) therapy (PPI test). During this study, patients maintained their regular pulmonary medications. The study was approved by the institutional review board.
Significant differences were evaluated by the Pearson's linear regression test, and the Wilcoxon signed ranks test. A p-value of less than 0.05 was considered to be statistically significant.
ResultsThe percentage of patients with GERD symptoms among all patients with BA was 27.4%. The percentage of patients with GERD symptoms plus a history of GERD among all patients with BA was 31%. There were no significant differences in the incidence of GERD symptoms according to BA severity and gender (data not shown). The proportions of asthmatics, with or without GERD symptoms, taking short-acting β2-agonists, theophyline, leukotriene antagonist, and inhaled corticosteroids suggested that asthma medication is not an important determinant of GERD symptoms (data not shown).
PPI therapy (PPI test) significantly decreased the FSSG score one month later (Figure 1).
There is a significant correlation between GERD symptom (F-scale score) and cough score and sputum sore (Figure 2). FSSG can divide into two symptoms subtypes: those associated with reflux and those with gastric dysmotility. The reflux symptoms significantly correlated with cough score, not with sputum score (Figure 3). The gastric dysmotility alone did not correlate with cough score or sputum score, although total F-scale score significantly correlated with those scores. There is no significant correlation between GERD symptom (F-scale score) and wheezing score or β2-agonists consumption score
DiscussionBA predisposes patients to GERD, whereas GERD may induce or aggravate BA. The two diseases interact with each other in a cause and effect relationship, which turns out to be a vicious circle. The prevalence of GERD in asthmatics is estimated at 34–89%, which probably reflects the variation in the definition of GERD and the populations studied.2–6 An evidence-based global consensus recently defined GERD as a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications.17 Novel aspects of this new definition include a patient-oriented approach that is independent of endoscopic findings and pH testing in the presence of typical or atypical symptoms or complications. The new definition also recognises that the refluxate causing symptoms may be weakly acidic or gaseous and these patients also meet the case definition of GERD.17
Diagnosis of GERD by obtaining a history is the quickest and simplest method. It does not put stress on patients. A QUEST score, which has been proven to be useful in the assessment of GERD, has been widely used to assess GERD symptoms.12 A higher QUEST score, however, only signifies that an event is more typical of GERD than of other conditions, so changes in the score for this questionnaire cannot be used to assess the severity of GERD or the response to treatment, although QUEST scores have been used for this in some studies.18 Recently, the FSSG has been available to provide an objective evaluation to assess the severity and the response to treatment.14 When the cut-off score was set at 8 points, the FSSG showed a sensitivity of 62%, a specificity of 59% and accuracy of 60%. The percentage of patients with GERD symptoms among all the patients with BA was 27.4%. PPI therapy (PPI test) significantly decreased the FSSG score one month later in our patients. These results indicated that the FSSG is useful to assess GERD in patients with BA.
The percentage of patients with endoscopic mucosal change among all the FSSG-positive patients was 28.6%, although endoscopy was performed in only 7 patients. Endoscopy provides direct visualisation of the oesophageal mucosa. However, the severity of GERD symptoms is not parallel to the damage of the oesophageal mucosa. Endoscopy often reveals no mucosal changes even if typical GERD symptoms existed.19,20
We found that GERD symptoms (F-scale score) significantly correlated with cough score and sputum score. In particularly, the reflux symptoms significantly correlated with cough score, not with sputum score. Littner et al.21 reported that lansprazole reduced asthma exacerbations and improved quality of life without improving asthma symptoms or pulmonary function test results, or reducing β2-agonist use. In contrast to these results, Shimizu et al. reported that PPI (lansoprazole) improves asthma symptoms without any changes in pulmonary function test results.22 In addition, a recent study demonstrated that there is no benefit of treatment with a PPI in patients with poorly controlled asthma who have minimal or no symptoms of gastro-oesophageal reflex. The study suggests that airway inflammation from microaspiration on oesophageal reflexes is not a common contributing mechanism of poor asthma control in patients who have persistent asthma symptoms despite the use of inhaled corticosteroid.23
In conclusion, the FSSG is useful to provide an objective evaluation to assess the severity in asthma patients. We revealed association between symptom subtypes of GERD and asthma related symptoms.