Psychological problems are more commonly observed in mothers of children with asthma when compared to the general population. Smoking in the house and parental cooperation are the other factors which influence psychological status in mothers of children with asthma. In our study, we aimed to investigate family functioning and frequency of psychological symptoms in mothers of children with asthma.
MethodsThe study group consisted of 160 mothers of 4–15 year old children with asthma and the control group consisted of 90 mothers of healthy children. Beck's inventory, continuous anxiety inventory and family assessment device were administered to each group of mothers.
ResultsResults indicated that levels of depression and anxiety symptoms were higher and perception of family functioning was less healthy in mothers of children with asthma compared to those in the control group (p<0.0001). Smoking status at home and level of communication with the father were found to have a significant impact on the evaluation scale in mothers in the case group.
DiscussionPsychiatric symptoms observed in mothers of asthmatic children might be associated to influencing the functioning of the entire family rather that of the mother alone. Therefore, evaluation of family functioning in mothers of children with asthma might be beneficial in terms of follow-up and control of disease.
Childhood asthma is a common chronic disease with potential to cause severe complications. The prevalence and morbidity of the disease has been increasing in the recent years.1,2 Psychiatric disorders which develop in the mother sometimes increase the morbidity and frequency of complications in the follow-up of children with asthma.3,4 Being a chronic disease, childhood asthma has the potential of causing various kinds of psychiatric disorders particularly in the mother as well as in the entire family of the asthmatic child.5,6 Moreover, having an asthmatic child and one that requires greater attention and special care may favour the development and/or maintenance of psychiatric symptoms and poorer levels of mothers’ mental health.5 Studies indicate a worsening family environment for asthmatic children as compared to the non-asthmatic population, and both the asthmatic child and his/her mother form part of the context of stressor, and this in turn may influence both the mothers’ mental health and that of other family members.5,7 Furthermore, some studies have shown the potential influence of prenatal stress and some psychosocial factors on the immunological and foetal neuro-endocrinal systems and their possible influence on the development of atopic diseases, such as asthma.8,9 We encountered few studies investigating the factors affecting the emergence of psychiatric complaints in mothers of asthmatic children in the literature on asthma,10,11 although there were numerous studies on psychiatric disorders observed in these mothers.6,12 In our study, we aimed to demonstrate perception of family life by mothers of children with asthma—the influence of Family Functioning on the emergence of psychiatric symptoms using the Family Assessment Device (FAD). In addition, we aimed to show the influence of smoking status at home and paternal cooperation in care of the child on symptoms observed in the mother.
Material and methodsSubjectsThis study has been performed on mothers of asthmatic children with mild to moderate asthma followed at the Paediatric Allergy Out-Patients Clinic of Vakif Gureba Hospital, Istanbul for at least one year between September 2007 and June 2008. Diagnosis and severity of asthma were defined retrospectively according to the Global Initiative for asthma guidelines.13 The control group consisted of mothers without any chronic diseases who applied to the out-patients clinic of the same hospital for simple diseases. Mothers with chronic diseases in other family members, history of use of psychotropic medications and history of any disease negatively affecting the mental state of the mother in the last 1 year were excluded from the study. However, presence of acute emergency visits was not taken into consideration in mothers of asthmatic children.
MeasuresA personal evaluation form designed to assess the socio-demographic features of the child and mother was filled out through interviews with the mother, relating to family interaction and maternal health.14,15 This interview also included the administration of Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI) and McMaster Family Assessment Device (FAD). STAI scale was filled by participants themselves in this interview.
Evaluation of anxiety and depression in mothersBDI was developed in 196116 and validated in Turkey in 1989 by Hisli.17 This is an evaluation scale consisting of 21 items on physical, mental, cognitional and motivational symptoms. The highest score is 63, and the cut-off point for validity-safety in Turkey has been determined as 17. Points equal to or above 17 indicate significant depressive disorder.
STAI was developed in 1970 by Spielberg et al.18 and adapted to Turkish by Oner and LE Compte.19 This scale is the one that is self-determined by the individual. It consists of 2 sub-scales each consisting of 20 items. Subgroup 1: State-trait anxiety inventory; defines how an individual feels at a certain moment and in certain conditions. Subgroup 2: Continuous anxiety inventory; defines how an individual feels generally regardless of the state and conditions of the moment. Scores from both scales range from 20-80. Higher scores indicate higher levels of anxiety. The cut-off point for validity-safety in Turkey has been determined as 36.19 Points equal to or above 60 indicate a high level of anxiety.
Family functioningFamily adjustment was assessed using the Family Assessment Device (FAD). FAD is based on the McMaster Model of Family Functioning and consists of a 60—item questionnaire designed for completion by parents,20 and adapted to Turkish people by Bulut.21 It consists of 7 subscales consisting of 60 items. These include 6 items on “Problem solving”; 9 items on “Communication”; 11 items on “Roles”; 6 items on reacting emotionally; 7 items “Affective Responsiveness”; 9 items on “Behaviour Control”; and 12 items on “General Functioning”. Each item is assessed with a score from 1 to 4. A score of 1 indicates a healthy answer whereas a score of 4 indicates a pathological finding. There is no global cut-off point for the FAD. The average of the scores is taken into consideration in each subscale according to the adapted Turkish version of FAD. Scores above 2 indicate impairment in family functioning and theoretically the cut-off point is 2 in each subscale.21
Statistical analysisThe statistical analysis of the study data was performed using SPSS for Windows 11.5 software package. Chi-square test was used to evaluate the categorical variables. For statistical significance, Fisher exact chi-square test was used when at least one of the expected values was below 5 and Yates continuity adjustment was used for the rest of the variables. Continuous variables of the case-control group were compared using the t-test. Comparison of BDI, STAI and FAD scores of the mothers was performed using the Mann-Whitney U test. The relationship of the scores with certain risk factors was analysed with Pearson correlation analysis. p Values less than 0.05 were considered statistically significant.
Ethical approvalThis study was approved by the Ethics Committee of the Vakif Gureba Hospital. Written informed consent was obtained from mothers of children.
ResultsThe study group included 160 mothers of children with mild to moderate asthma (87 males and 73 females) aged between 4–15 years (mean=7.4±2.9). Thirty children (19%) had moderate asthma and 130 children had mild asthma. More children were identified with mild asthma during the study period. Asthma diagnosis and disease severity was similar on the time of evaluation of mothers’ scales. In 94% of cases the mother was the main caregiver, in 6% the father was the main caregiver. Ninety-four percent of children lived in two-parent families and the remainder lived in single-parent families. The control group consisted of mothers of 90 children without any chronic diseases. Children in the control group were 5–16 years (mean=8.2±3.9) and consisted of 42 males and 48 females. Ninety-six percent of children lived in two-parent families in the control group and in 97% of cases the mother was the main caregiver.
Table 1 shows the socio-demographic data of the mothers in the study and control groups. The presence of no significant differences between the socio-demographic data of the two groups except one-parameter (economic level) allowed us to obtain clearer results in the comparison of the two groups.
Socio-demographic features of mothers in the case and control groups
| Case group (N=160) | Control group (N=90) | p | |
| Age (mean) ±SD (years) | 34±7.3 | 30±4.7 | 0.52 |
| Number of siblings (n) | |||
| 1(%) | 55(34) | 28(31) | 0.41 |
| 2(%) | 85(53.5) | 53(59) | |
| >2(%) | 20(12.5) | 9(10) | |
| Occupation | |||
| Housewife n (%) | 130 (81) | 75(83) | 0.75 |
| Worker n (%) | 30 (19) | 15(17) | |
| Monthly income (€) (±SD) | 500±60 | 650±40 | 0.02 |
| Mothers Education Level | |||
| ≤8 years n (%) | 95(59) | 58(64) | 0.33 |
| High school n (%) | 58 (37) | 29(33) | |
| University | 7(4) | 3(3) | |
| Age of marriage, median (range-in years) | 23(18–25) | 24(19–26) | 0.90 |
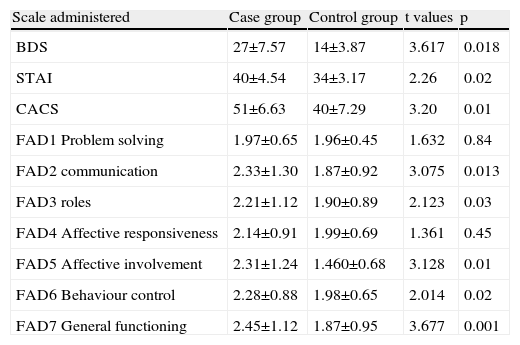
Mean scale scores of the groups are presented in Table 2. According to these data BDI, STAI and FAD2, FAD3, FAD5, FAD6, and FAD7 scores were found statistically significantly higher in the case group compared to the control group.
Distribution of mean scores (±SD) on BDS, STAI, CACS and FAD in the study and control groups
| Scale administered | Case group | Control group | t values | p |
| BDS | 27±7.57 | 14±3.87 | 3.617 | 0.018 |
| STAI | 40±4.54 | 34±3.17 | 2.26 | 0.02 |
| CACS | 51±6.63 | 40±7.29 | 3.20 | 0.01 |
| FAD1 Problem solving | 1.97±0.65 | 1.96±0.45 | 1.632 | 0.84 |
| FAD2 communication | 2.33±1.30 | 1.87±0.92 | 3.075 | 0.013 |
| FAD3 roles | 2.21±1.12 | 1.90±0.89 | 2.123 | 0.03 |
| FAD4 Affective responsiveness | 2.14±0.91 | 1.99±0.69 | 1.361 | 0.45 |
| FAD5 Affective involvement | 2.31±1.24 | 1.460±0.68 | 3.128 | 0.01 |
| FAD6 Behaviour control | 2.28±0.88 | 1.98±0.65 | 2.014 | 0.02 |
| FAD7 General functioning | 2.45±1.12 | 1.87±0.95 | 3.677 | 0.001 |
BDS, Beck Depression Scale; STAI, State-trait anxiety scale; CACS, Continuous Anxiety Concern Scale; FAD, Family Assessment Device Scale.
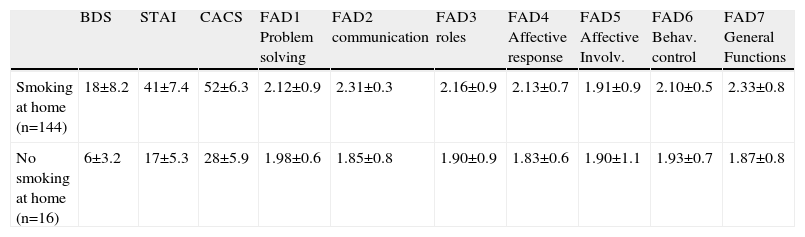
The frequency of persistent smoking inside the house despite warnings revealed that the frequency of smoking was 90%. Hundred percent of the mothers in the study group expressed anger against smoking at home, while 87% of the mothers in the control group had a smoker at home and 100% were negatively affected from this condition. Scale scores of mothers living in positive and negative smoking-status homes are shown in Table 3. Data in this table shows significantly higher mean scores for mothers in the study group who have at least one smoker at home.
Distribution of mean scores (±SD) according to the smoking status at home in the case group
| BDS | STAI | CACS | FAD1 Problem solving | FAD2 communication | FAD3 roles | FAD4 Affective response | FAD5 Affective Involv. | FAD6 Behav. control | FAD7 General Functions | |
| Smoking at home (n=144) | 18±8.2 | 41±7.4 | 52±6.3 | 2.12±0.9 | 2.31±0.3 | 2.16±0.9 | 2.13±0.7 | 1.91±0.9 | 2.10±0.5 | 2.33±0.8 |
| No smoking at home (n=16) | 6±3.2 | 17±5.3 | 28±5.9 | 1.98±0.6 | 1.85±0.8 | 1.90±0.9 | 1.83±0.6 | 1.90±1.1 | 1.93±0.7 | 1.87±0.8 |
BDS, Beck Depression Scale; STAI, State-trait anxiety scale; CACS, Continuous Anxiety Concern Scale; FAD, Family Evaluation Device.
The results of Table 3 showed that smoking at home increases the stress load of mothers since it directly affects the health of the asthmatic child. The presence of only 16 families with negative smoking status at home out of a case group of 160 individuals did not allow for evaluation in terms of statistical workout. Another factor that was found to influence maternal psychiatric status was her opinion about the paternal cooperation in child care. The father was not fulfilling his responsibilities regarding the child's disease according to 64% of mothers in the study group. In addition, adequate cooperation was found to have a positive impact on the mean scores although the rate of smoking was 80% in these families.
DiscussionIn this study, most of the FAD scores (FAD2, FAD3, FAD5, FAD6 and FAD7) were found to be significantly higher in the case group compared to the control group. This study is the first study to our knowledge that shows the FAD results in mothers of children with asthma. Extensive prevalence of psychiatric symptoms in mothers of children with asthma has been demonstrated in several studies.4,12,22,23 However, none of these studies have used family assessment measurement scores; instead, psychiatric symptoms were assessed according to DSM-IV diagnostic criteria.
Significantly high FAD scores in our study may suggest the presence of communication problems in families having an asthmatic child. Inadequate communication might lead to incomplete perception of the demands and needs of mother by the rest of the family members. This, in turn, has various effects on the mother's mental health.24
The relationship between having an asthmatic child and the development of psychological impairments in the mother is a complex one including daily stress, relationship between the mother and the rest of the family members and being able to obtain proper help when needed. In our study, we evaluated only the familywise communication part of this complex relationship. We did not study the ability to obtain proper help regarding the disease and possible effects of daily stress. In addition, the need for emergency room visits was also not investigated within the scope of this study since the objective was not to determine the relationship between the severity of disease and functional impairments of the mother and family. Barlet et al.3 reported that there is a relationship between the psychiatric symptoms of the mother and use of emergency room. They also showed that demographic features did not have a significant impact on this relationship. We also did not determine any significant relationships between some demographic findings that including number of children, age at marriage, and level of education in terms of case and control groups. However, we showed a statistically significant low economic level in the case group in our study.
Smoking status inside the house was one of the factors that were evaluated for its influence on the FAD scores.25 Any object that harms the child will lead to distress in the mother and thus increase the mother's stress load.26 Failure of the mother in trying to prevent harmful behaviours including smoking at home might lead to feelings of guilt. This, in turn, creates feelings of anger and hatred against the other member (father) of the family who smokes. This psychological opinion is also observable in our study results. Although we could not obtain a statistical measurement between the case subgroups because of insufficient case numbers, we can say that smoking does affect family functioning negatively, since the mean scores of family functioning of mothers with no smoking at home were lower than those of smoking at home in the case subgroup.
High rates of smoking at home despite the presence of an asthmatic child and despite the mother's objection should certainly be found strange. Negative and even fatal effects of smoking on the respiratory system have been proven in several studies.27,28 We could not find any reasonable explanations for this condition except for the low socio-economic level of the families in the case group.
Smoking at home has been found to be one of the major factors affecting the psychological condition of the mother. Non-cooperating father was found to be a more determining parameter than smoking at home, since the rate of smoking at home was 81% in families with a cooperating father.
Mental indicators of mothers with cooperating husbands are also influenced positively from this cooperation. The congruity and strong communication resulting from fulfilment of responsibilities mutually should also affect the mental status of the child positively.29 We may conclude that our results of FAD regarding family functioning supported our study.
These results highlight the importance of obtaining information directly from asthmatic children's mothers when assessing the impact of asthma on family quality of life when the focus is on mothers’ subjective experience of their children's illness. In the past, family-based interventions have focused on trying to improve children's compliance with medication or improving their psychological adjustment. Less attention has been given to the impact of family functioning on mothers’ perceptions of their quality of life.30
Our data on family functioning indicate that the presence of a chronic disease such as childhood asthma may increase the underlying family conflicts. This finding also underlines the importance of evaluating family functioning as well as the child and mother. Given the continuous nature of asthma, undervaluing the assessment of family functioning should lead to some deficiency in the control of the child's disease. Increasing the cooperation between related professionals (psychiatrist, allergy physician, family physician, paediatrician) and the level of psychiatric support provided to mothers of children with asthma and assessment of their family functioning may help to increase maternal psychiatric status, and this in turn will affect the management of the asthmatic child.
Key-points: Childhood asthma affects the family functioning negatively. Low socio-economic status is associated with smoking at the home. Smoking in the home is strictly associated with failed family function measures in the mother of asthmatic children.