Antibiotic hypersensitivity states present an often frustrating challenge for most physicians.
The knowledge of the natural history, course and pathogenesis of the reactions of these antibiotic intolerant patients remains superficial. Because of limited number of immunodiagnostic tests for these patients, many practitioners have concluded total avoidance of offending drugs and replacing with their safe alternatives 1 .
Quinolones have been the centre of considerable scientific and clinical interest since their discovery in the early 1960s. This is because they potentially offer many of the attributes of an ideal antibiotic, combining high potency, a broad spectrum of activity, good bioavailability, oral and intravenous formulations, high serum levels, a large volume of distribution indicating concentration in tissues and a potentially low incidence of side-effects. Much research has attempted to make these potential attributes real 2 . Moxifloxacin (Avelox ® ), the latest fluoroquinolone, might be among safe alternative antibiotics with only few reported anaphylactoid reactions 3,4 .
The purpose of this survey was to investigate whether moxifloxacin can be among the safe alternative antibiotics determined by OPT for antibiotic intolerant patients.
MATERIAL AND METHODSTo investigate the tolerability of moxifloxacin in antibiotic allergic/intolerant patients, 20 patients who were referred to our clinic between 1 January 2003 and 31 December 2003 and diagnosed antibiotic hypersensitivity were enrolled in this survey. The diagnosis was made by the positive history of at least one reaction with the liable antibiotic.
A standard questionnaire, including the questions about age, gender, accompanying allergic and systemic diseases, liable antibiotic, the type, the time of onset and the duration of reaction was completed by a physician for each patient.
We performed OPTs with moxifloxacin to antibiotic intolerant patients. An inform consent was obtained from each patient. Tests were performed by an allergist in the out-patient clinic where all emergency tools were available as required.
The OPT protocol was single-blind and placebo controlled. The placebo and moxifloxacin with a total dose of 1000 mg were given at thirty minutes intervals in divided dosages. During the procedure blood pressures, peak expiratory flow (PEF) values and possible allergic reactions were monitored every 15 minutes up to three hours and every one hour afterwards.
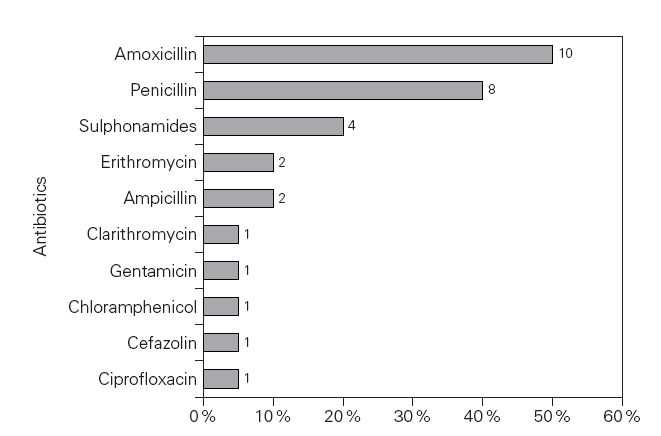
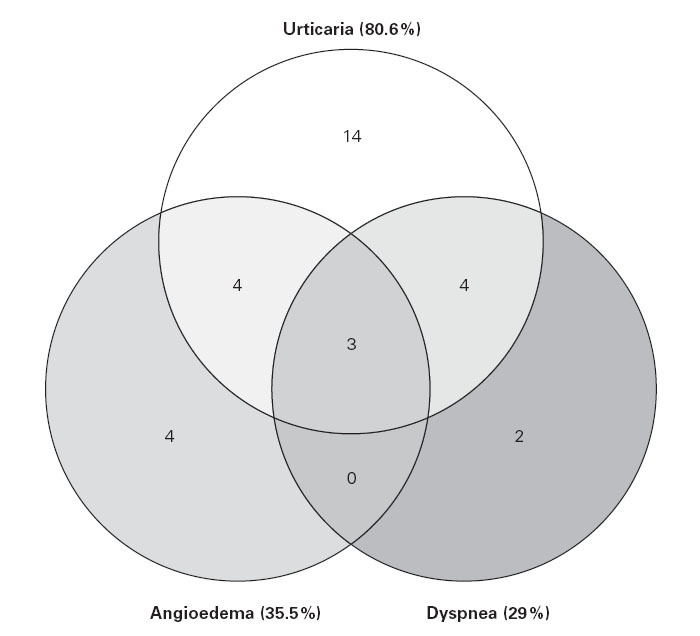
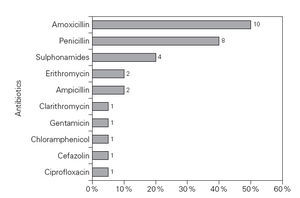
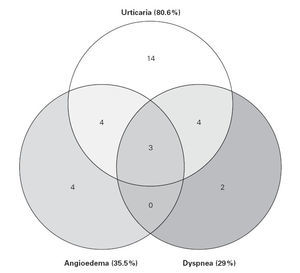
RESULTSThe mean age of the patients was 38.05 ± 14.1 and 17 (85 %) of them were females. There were only two patients with accompanying allergic diseases; one with bronchial asthma and the other with chronic urticaria (table I). The rates of common anamnestic antibiotic hypersensitivities were 50 % with amoxicillin, 40 % with penicillin, 20 % with sulphonamides, respectively (fig. 1). There were 31 reactions in 20 patients.Urticaria (80 %) was the leading reaction appearing after antibiotic ingestion (fig. 2). The mean time interval between the ingestion of the drug and the onset of the reactions was 48.2 ± 120.6 minutes and the mean duration of reactions with antibiotics was 27.6 ± 26,6 hours.
Table I The demographic features of the antibiotic intolerant patients (n = 20)
Figure 1.—The rates of common anamnestic antibiotic hypersensitivities (n = 20).
Seventeen of 20 patients tolerated moxifloxacin at therapeutic doses without any problem. One patient experienced generalized urticaria 4 hours after ingestion of the first dose of the drug, which resolved spontaneously 5 hours after the onset. Another patient experienced tachycardia (heart rate did not exceed beyond 115 per minute) 2.5 hours after ingestion of first dose of the drug, which resolved spontaneously 2 hours after the onset, and a third one developed severe nausea lasting for two hours.
Figure 2.—The distribution of allergic reactions due to antibiotics (n = 31).
DISCUSSION
In this survey, the antibiotics which most commonly caused allergy are amoxicillin, penicillin and sulphonamides, by history. Macrolides, floroquinolones and aminoglycosides are the antibiotics with a low risk of sensitization. The most common anamnestic allergic reaction was urticarial reaction as in a recent study 5 .
The most common drug-related adverse effects (AEs) with fluoroquinolone therapy involve the gastrointestinal tract and central nervous system and are usually transient and mild to moderate in severity 6 . In our study, only one of our patients suffered a mild nausea, and the other one suffered a mild arrhythmia without clinical significance. In the third patient, moxifloxacin induced an immediate reaction (generalized urticaria) in which an immunologic mechanism, probably directed to a specific moxifloxacin metabolite, seems to be involved. This patient had suffered an urticarial reaction with ciprofloxacin This could be explained by the cross-reactivity with other quinolones, as reported before. The cross-reactivity between quinolones seems to be very important, and avoidance of any quinolone should be recommended to any patient who has suffered an allergic reaction to one of these drugs 7 .
In conclusion, given the high incidence of hypersensitivity reactions to beta-lactam antibiotics the use of new fluoroquinolone, moxifloxacin might represent a safe therapeutic alternative.
Antibiotics are among the most commonly used drugs in medicine. Medical progress in understanding and managing antibiotic hypersensitivity states often requires collaborative efforts of multiple disciplines. The high morbidity and cost associated with antibiotic hypersensitivity makes this condition a high priority for future research investments 1 .
Correspondence:
B. BozkurtHacettepe University, School of Medicine Department of Chest Diseases, Adult Allergy Unit 06100 Sıhhiye Ankara/Turkey E-mail: bubozkur@hacettepe.edu.tr