We interestedly read the manuscript ‘Is abnormal liver function correlated with food sensitisation in adults?’ by Shiue et al.1 The dietary protein antigen induced proctocolitis, is characterised by the presence of mucoid and bloody stools, and regression of symptoms under an elimination diet, in otherwise healthy infants. Cell-mediated cow's milk hypersensitivity associated liver injury was reported in infancy.2,3 We here described transient transaminase elevation in five infants with non-IgE mediated cow's milk protein antigen induced proctocolitis.
We retrospectively analysed medical records of 70 patients diagnosed cow's milk antigen induced proctocolitis for hypertransaminasemia from April 2010 to December 2013 in our gastroenterology outpatient clinic. Patients’ age, duration and characterisation of symptoms, feeding pattern, total eosinophil counts, alanine aminotransferase (ALT), aspartate aminotranferase (AST), gamma-glutamyl transpeptidase (GGT), alkaline phosphatase (AP), bilirubin, total immunoglobulin (Ig) E, milk-specific IgE levels were noted at presentation. In the presence of hypertransaminasemia, alpha-1 antithyripsine levels, serology for hepatitis B and C, Human Immunodeficiency Virus, Cytomegalovirus, Epstein Barr Virus, liver ultrasonography, ALT and AST levels during follow-up were noted. Patients who had bloody mucoid stools, 1.5 fold of upper normal limit of ALT and/or AST levels, normal total IgE levels and negative for cow's milk specific IgE were included in the study. Patients who had inadequate weight gain, hyperbilirubinemia, positive viral serology, alpha-1 antithyripsine deficiency were excluded from the study. Normal ranges of ALT and AST were 0–33IU/l, and 0–38IU/l respectively. Normal levels of serum total IgE was 0–100IU/l and cow's milk specific IgE was negative if <0.35kUa/L.
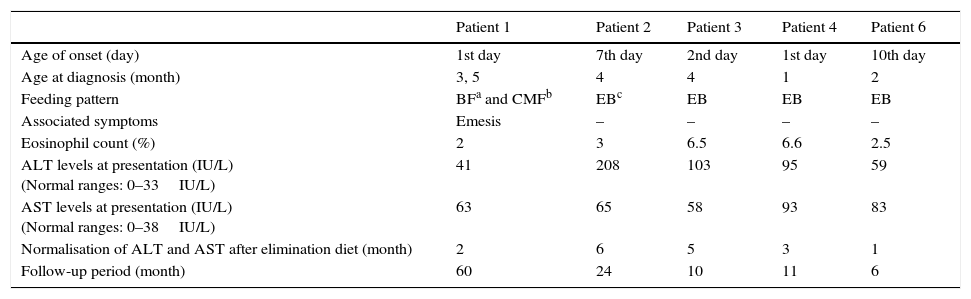
Out of 70 patients, only five (three girls, 60%) infants had transaminase elevation. The median symptom onset age was two days of life (1–10 day). Patients’ mean presentation age was 2.9±1.3 (1–4) months. All patients had normal physical examination findings and there was no skin involvement. Two patients had slight eosinophilia (Table 1). Serum total bilirubin, GGT, ALP and levels were normal in all patients. At presentation mean ALT levels were 101.2±65IU/l (41–208IU/l), mean AST levels were 72.4±14.8IU/l (58–93IU/l). All patients had normal hepatobiliary ultrasonography. All patients underwent a cow's milk elimination diet at presentation. The symptoms of all patients were improved or significantly reduced in the first month of elimination diet. The normalisation of both ALT and AST were determined mean 3.4±2 months (1–6 months) after initiation of elimination diet. No increment in transaminases was determined for a median of 11 months (6–60 months) of follow-up period.
Characteristics of patients with non IgE-mediated cow's milk allergy.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 6 | |
|---|---|---|---|---|---|
| Age of onset (day) | 1st day | 7th day | 2nd day | 1st day | 10th day |
| Age at diagnosis (month) | 3, 5 | 4 | 4 | 1 | 2 |
| Feeding pattern | BFa and CMFb | EBc | EB | EB | EB |
| Associated symptoms | Emesis | – | – | – | – |
| Eosinophil count (%) | 2 | 3 | 6.5 | 6.6 | 2.5 |
| ALT levels at presentation (IU/L) (Normal ranges: 0–33IU/L) | 41 | 208 | 103 | 95 | 59 |
| AST levels at presentation (IU/L) (Normal ranges: 0–38IU/L) | 63 | 65 | 58 | 93 | 83 |
| Normalisation of ALT and AST after elimination diet (month) | 2 | 6 | 5 | 3 | 1 |
| Follow-up period (month) | 60 | 24 | 10 | 11 | 6 |
We here described transient transaminase elevation in five infants with non-IgE mediated cow's milk protein antigen induced proctocolitis, which normalised with dietary cow's milk elimination. Saito et al.,2 showed isolated hypertransaminasemia that improved after elimination of cow's milk based formulas. They demonstrated cow's milk protein specific lymphocyte proliferation was increased and hepatic dysfunction might be related to delayed type hypersensitivity against cow's milk.2 Macromolecules may be taken up by the intestinal mucosa and can be detected in peripheral blood at limited rates, but increased uptake of macromolecules occurs due to immaturity of gut barrier, the presence of structural or functional abnormalities of the gastrointestinal tract, and secondary inflammatory events. Intestinal mucosa is not fully matured in infants or with an impaired barrier, increased uptake of macromolecules may occur. Moreover, food allergens may mediate local intestinal inflammation through release of pro-inflammatory cytokines, causing increased intestinal permeability and fluid shifts. Increased intestinal permeability may contribute to the influx of antigens into the submucosa and enter to the portal circulation. Food derived antigens flow from the intestines, interact with the T cells in liver and may initiate liver damage.4 In liver Kupffer cells, sinusoidal endothelial cells and hepatocytes themselves present antigenic peptides and could be targets for the cytotoxic CD8 (+) cells.5 These interactions may explain the mechanism of hepatic dysfunction, but much remains elucidated.
As a conclusion, transient elevation of transaminase levels in non IgE-mediated cow's milk allergy should be kept in mind and needs to be investigated in further studies.