As triggers have a potential to induce asthma exacerbations, awareness of the patients to individual triggers as well as protective measures might be helpful to prevent asthma attacks. Though allergens and allergen avoidance have been studied extensively, there are only few studies on non-allergic triggers and their avoidance for adult patients with asthma. In this study, we wanted to investigate asthma triggers and compliance to the preventive measures in an adult population.
MethodsOne hundred and thirty one adult asthma patients were enrolled into the study. A face to face interview was done by using a questionnaire including individual asthma triggers, prevention measures against major modifiable triggers and knowledge sources of the cases.
ResultsRegardless of asthma severity, 59.5 % of the subjects reported to be triggered by more than 10 factors. The most common triggers were air pollutants (89.3 %) and weather changes (81.7 %). Severe group was more frequently affected by medications, emotional stress, weather changes and indoor pollutants than other severity groups (p=0.017, 0.014, 0.049 and 0.018, respectively) whereas stress was reported more frequently by females than males. Prevention measures were insufficient regarding some major triggers.
ConclusionAdult patients are vulnerable to several triggers regardless from underlying severity of the illness. Insufficient compliance to the major preventive measures indicates that new strategies are needed to prevent asthma attacks caused by modifiable triggers.
Asthma is a chronic inflammatory disease of the airways which affects millions of people throughout the word. Asthma exacerbations may be caused by a variety of factors defined as “triggers” which include both allergens, and non-allergic factors such as viral infections, pollutants, drugs and others.1–5 Therefore, awareness of the patients about individual triggers as well as measures against these triggers might be helpful to prevent some asthma attacks. However, creating a low-allergen environment in patients' homes and reduced exposure to indoor allergens has been shown to be ineffective at reducing asthma symptoms.1,2,6 Therefore, other non-allergic triggers and actions taken against these factors, as well as assessing the outcomes in asthma control could be of interest.
The main non-allergic asthma triggers are indoor air pollutants, including passive and active smoking, harmful fumes and gases from heating devices, outdoor air pollutants including exhaust gases, certain weather and atmospheric conditions, influenza infections, psychological factors, physical activities and certain medications such as aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs), and beta blockers.1,2 Actually, all of these factors are a part of routine daily life of patients with asthma, and therefore have potential to induce asthma episodes in vulnerable cases. Although the studies which investigate the effect of tertiary prevention actions taken against indoor allergens on asthma outcomes are from some time ago, there is evidence that preventive measures for non-allergic asthma triggers might provide a beneficial outcome on asthma symptoms and, therefore, on asthma control. However, the number of studies on asthma triggers and preventive measures is limited and mostly analysed children based on the reports of parents or caregivers.7–10 There are only a few studies which investigate asthma triggers in adult asthma.3,11,12 These studies indicated that non-allergic triggering factors were important predictors of patients' general well-being; asthma control; and management of asthma, compared to allergic triggers.
In this study, our principal objective was to document the profile of asthma triggers of our adult patient group and their ability to cope with these triggers in their daily life. In detail, our aims were: 1) to quantity asthma triggers; 2) to determine what behaviours these adults have used to reduce their exposure to major triggers; and which factors affect these behaviours; and 3) to assess asthma information sources in an adult clinical population in Turkey.
Material and methodsPatient selection and the study designThe study was conducted in the outpatient allergy clinic of our tertiary university hospital. A total of 131 adult patients with asthma were consecutively enrolled into this cross-sectional study. Asthma diagnosis was based on a history of recurrent symptoms of wheezing, shortness of breath, cough and demonstration of objective signs of reversible airway obstruction by means of at least > 12 % increase in FEV, after 15 minutes with an inhalation of 200 μg salbutamol.1,2
Demographics (age, gender, education, occupation, smoking status) and disease characteristics (duration and severity of asthma, presence of atopy, family history of allergy) were recorded. Asthma severity was determined by the frequency of asthma symptoms, pulmonary function tests, and medication requirements according to international asthma guidelines. Disease was classified as mild intermittent, mild persistent, moderate persistent and severe persistent asthma.1
Atopy was defined by positive skin prick tests (SPT), which were performed using a standardised panel including Dermatophagoides pteronyssinus, Dermatophagoides farinae, grass, tree, weed pollens; cat, dog, cockroach, Alternaría and Cladosporium antigens (Allergo Pharma/Germany). A wheal diameter of 3 mm greater than negative control was considered positive.
Asthma triggers, actions taken against these triggers, and information sources of the patients were assessed by a questionnaire which was developed by the authors to serve the requirements of the topic of “prevention of asthma symptoms and exacerbation” in the international asthma guidelines.1 A face-to-face interview between patients and a chest physician/allergy specialist was conducted to fill out the questionnaire. After a pilot trial in a small group of patients, the study, has then been set for the target study group.
The questionnaire consisted of three main topics with either yes/no or multiple choice questions. In part one, non-allergic triggering factors reported as the most common triggers in the asthma textbooks and the international guidelines were listed in random order (see Appendix 1). The study subjects were asked to highlight the name(s) of the triggers which worsen their asthma symptoms. In part two; tertiary prevention measures related to preventing some major asthma triggers and the attitude changes that had been made by patients in their routine life following asthma diagnosis were investigated. Finally in the last part of the questionnaire, the information sources of the patients were evaluated. All patients gave verbal informed consent to be included in the study.
Asthma Triggers Questionnaire
| Please indicate that; which one of these triggering factors below causes worsening in your asthma? You can signal more than one triggering factor. | |
| 1. | Outdoor air pollution (exhaust fumes, other harmful gases in the atmosphere etc) |
| 2. | Indoor air pollution (heating devices such as: gas-stoves, fire places, wood-stoves, etc) |
| 3. | Cigarette smoke |
| 4. | Active cigarette smoking by yourself |
| 5. | Weather changes (hot air, cold air, severe humidity in the air etc) |
| 6. | Strong scents (cooking smells, room sprays, smell of detergents, perfumes etc) |
| 7. | Emotional stimulation (feeling sadness, stress/anxiety) |
| 8. | Upper airway infections (having a cold, flu etc) |
| 9. | Exercise (walking, swimming, running, bicycles etc) |
| 10. | Medications (aspirin, other NSAID, ACE inhibitors, Beta blockers etc) |
The statistical analyses were performed by computer software (SPSS version 11.0, Chicago, Illinois). Descriptive statistics were expressed as mean ± SEM and n (%). Categorical data were tested by Chi-square test. One way ANOVA was used for the comparison of continuous variables in different asthma severities. As there were only a few number of subjects with mild intermittent asthma, data on these subjects were combined with those with mild persistent asthma in statistical analysis. A p value less than 0.05 was considered as statistically significant.
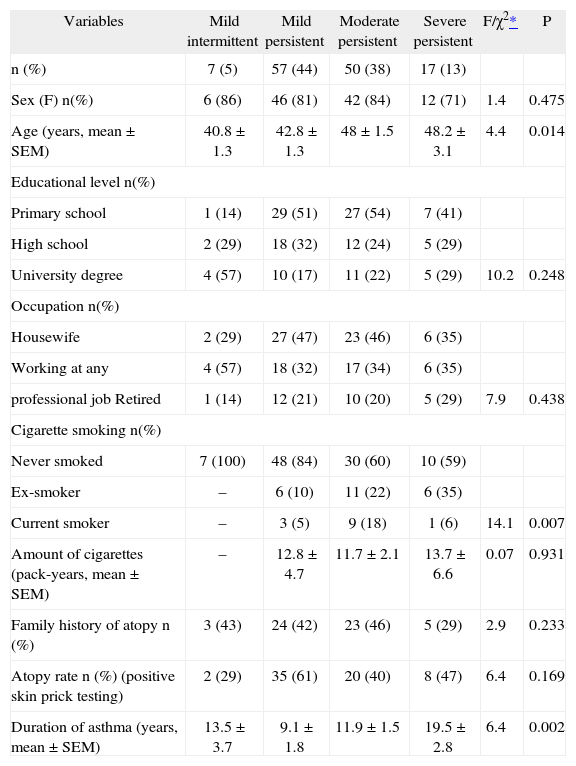
ResultsDemographics and disease characteristicsA total of 131 adult patients with asthma [F/M: 106/25 (80.9/19.1 %) and mean age 45.4 ± 0.9] were included in the study. The mean duration of asthma was 11.7 ± 0.9 years. Sixty five patients (49.6 %) had positive SPT. Most of the patients had mild persistent asthma (n = 57; 43.5 %) (Table I).
Demographics and clinical features of the study subjects (n = 131)
| Variables | Mild intermittent | Mild persistent | Moderate persistent | Severe persistent | F/χ2* | P |
| n (%) | 7 (5) | 57 (44) | 50 (38) | 17 (13) | ||
| Sex (F) n(%) | 6 (86) | 46 (81) | 42 (84) | 12 (71) | 1.4 | 0.475 |
| Age (years, mean ± SEM) | 40.8 ± 1.3 | 42.8 ± 1.3 | 48 ± 1.5 | 48.2 ± 3.1 | 4.4 | 0.014 |
| Educational level n(%) | ||||||
| Primary school | 1 (14) | 29 (51) | 27 (54) | 7 (41) | ||
| High school | 2 (29) | 18 (32) | 12 (24) | 5 (29) | ||
| University degree | 4 (57) | 10 (17) | 11 (22) | 5 (29) | 10.2 | 0.248 |
| Occupation n(%) | ||||||
| Housewife | 2 (29) | 27 (47) | 23 (46) | 6 (35) | ||
| Working at any | 4 (57) | 18 (32) | 17 (34) | 6 (35) | ||
| professional job Retired | 1 (14) | 12 (21) | 10 (20) | 5 (29) | 7.9 | 0.438 |
| Cigarette smoking n(%) | ||||||
| Never smoked | 7 (100) | 48 (84) | 30 (60) | 10 (59) | ||
| Ex-smoker | – | 6 (10) | 11 (22) | 6 (35) | ||
| Current smoker | – | 3 (5) | 9 (18) | 1 (6) | 14.1 | 0.007 |
| Amount of cigarettes (pack-years, mean ± SEM) | – | 12.8 ± 4.7 | 11.7 ± 2.1 | 13.7 ± 6.6 | 0.07 | 0.931 |
| Family history of atopy n (%) | 3 (43) | 24 (42) | 23 (46) | 5 (29) | 2.9 | 0.233 |
| Atopy rate n (%) (positive skin prick testing) | 2 (29) | 35 (61) | 20 (40) | 8 (47) | 6.4 | 0.169 |
| Duration of asthma (years, mean ± SEM) | 13.5 ± 3.7 | 9.1 ± 1.8 | 11.9 ± 1.5 | 19.5 ± 2.8 | 6.4 | 0.002 |
Regarding the severity of asthma; there were no differences between gender, education level, occupation, family history of allergy and individual atopy rate. The patients with moderate to severe asthma were older and smoked more than mild asthma patients (p < 0.05). Severe asthma patients had longer asthma durations.
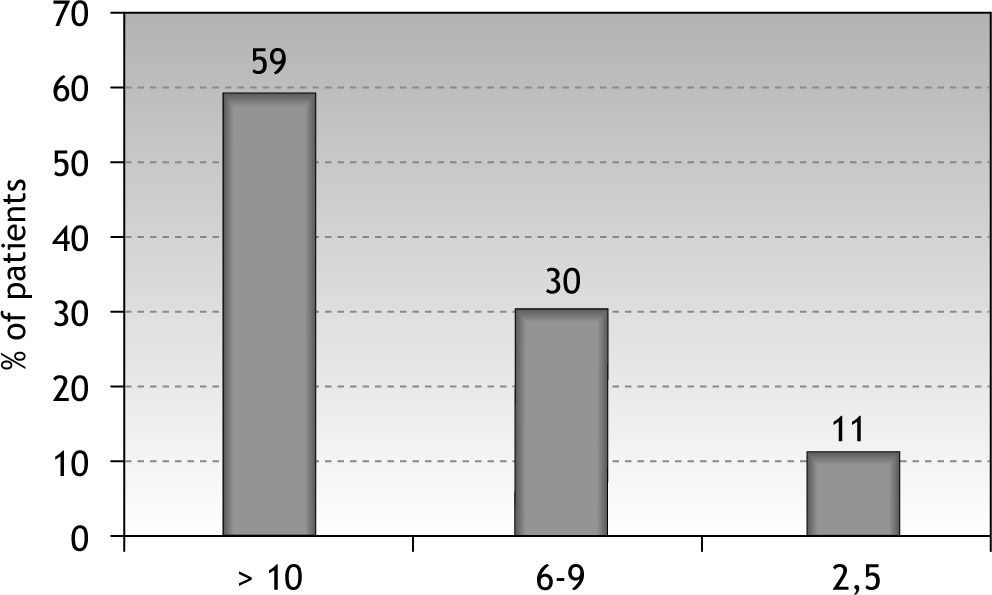
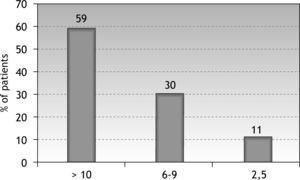
Part I: Quantification and classification of triggersNumber of triggering factorsThe mean number of triggering factors in the study group was 11.8 ± 0.4. The majority of the subjects (n = 78; 59.5 %) reported more than 10 factors as triggering their asthma, whereas 30.5 % (n = 40) and 9.9 % (n = 13) of the subjects reported to be triggered by 6–10 triggers and 2–5 triggers, respectively (Fig. 1). All patients reported at least two triggers and each of the triggers in the list was reported by at least one patient.
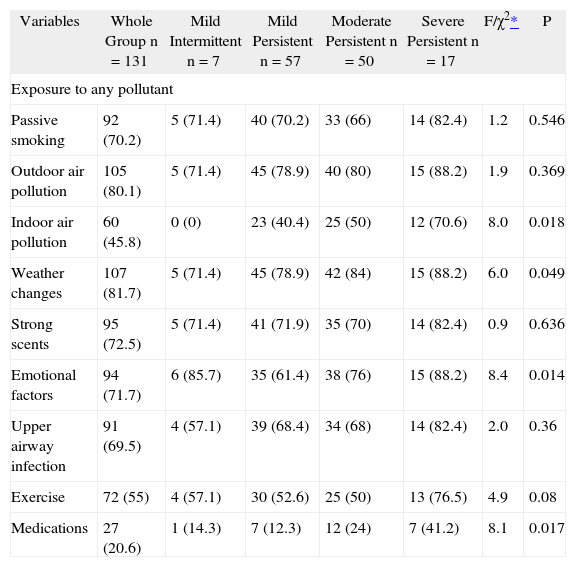
TriggersExposure to any pollutants such as cigarette smoking, outdoor and indoor pollution were the most common triggering factors (n = 117; 89.3 %); followed by exposure to dust (n = 99; 75.5 %); strong odours (n = 95; 72.5); emotional distress (n = 94; 71.7 %) and upper airway infections (n = 91; 69.4 %) (Table II).
Type of triggering factors according to severity of asthma. Values are expressed as n(%)
| Variables | Whole Group n = 131 | Mild Intermittent n = 7 | Mild Persistent n = 57 | Moderate Persistent n = 50 | Severe Persistent n = 17 | F/χ2* | P |
| Exposure to any pollutant | |||||||
| Passive smoking | 92 (70.2) | 5 (71.4) | 40 (70.2) | 33 (66) | 14 (82.4) | 1.2 | 0.546 |
| Outdoor air pollution | 105 (80.1) | 5 (71.4) | 45 (78.9) | 40 (80) | 15 (88.2) | 1.9 | 0.369 |
| Indoor air pollution | 60 (45.8) | 0 (0) | 23 (40.4) | 25 (50) | 12 (70.6) | 8.0 | 0.018 |
| Weather changes | 107 (81.7) | 5 (71.4) | 45 (78.9) | 42 (84) | 15 (88.2) | 6.0 | 0.049 |
| Strong scents | 95 (72.5) | 5 (71.4) | 41 (71.9) | 35 (70) | 14 (82.4) | 0.9 | 0.636 |
| Emotional factors | 94 (71.7) | 6 (85.7) | 35 (61.4) | 38 (76) | 15 (88.2) | 8.4 | 0.014 |
| Upper airway infection | 91 (69.5) | 4 (57.1) | 39 (68.4) | 34 (68) | 14 (82.4) | 2.0 | 0.36 |
| Exercise | 72 (55) | 4 (57.1) | 30 (52.6) | 25 (50) | 13 (76.5) | 4.9 | 0.08 |
| Medications | 27 (20.6) | 1 (14.3) | 7 (12.3) | 12 (24) | 7 (41.2) | 8.1 | 0.017 |
Regarding the mean number of triggers; there was no difference among groups with various severity degrees, age, gender and individual atopy.
The patients with severe persistent asthma reported weather changes, medications, emotional factors and indoor pollutants as triggers more than mild and moderate severity groups did (p = 0.049, 0.017, 0.014, and 0.018, respectively). Female subjects and the subjects with higher education reported emotional stress as triggers more frequently (p = 0.025 and 0.016, respectively). There was no relationship between the type of triggers and individual atopy, age or asthma duration.
Part II: Behaviours and attitude changes by patients following asthma diagnosisCigarette smoking habitsWhen the general smoking habits were asked, of all the respondents 72.5 % (n = 95) declared that they had never smoked. The rest of the patients (n = 23, 17.6 %) had quitted smoking, whereas 9.9 % (n = 13) still continued smoking. When asked specifically “Did you quit cigarette smoking because of your asthma diagnosis?” among 24 cases who were smokers at the time of asthma diagnosis, 45.8 % (n = 11) reported quitting cigarette smoking because of asthma diagnosis.
Influenza vaccination and strategies for prevention from influenzaWhen asked “What kind of behaviour changes have you done against flu infections after your asthma diagnosis?” 31 % of the patients (n = 46) reported beign vaccinated regularly against influenza. Regarding the general recommended procedures for prevention of influenza (i.e.: vaccination; wearing mask; keeping away from infected people); 45 % (n = 59) and 41.9 % (n = 55) of the subjects had performed one or two of these actions, respectively, whereas only seven subjects (5.3 %) had performed all three.
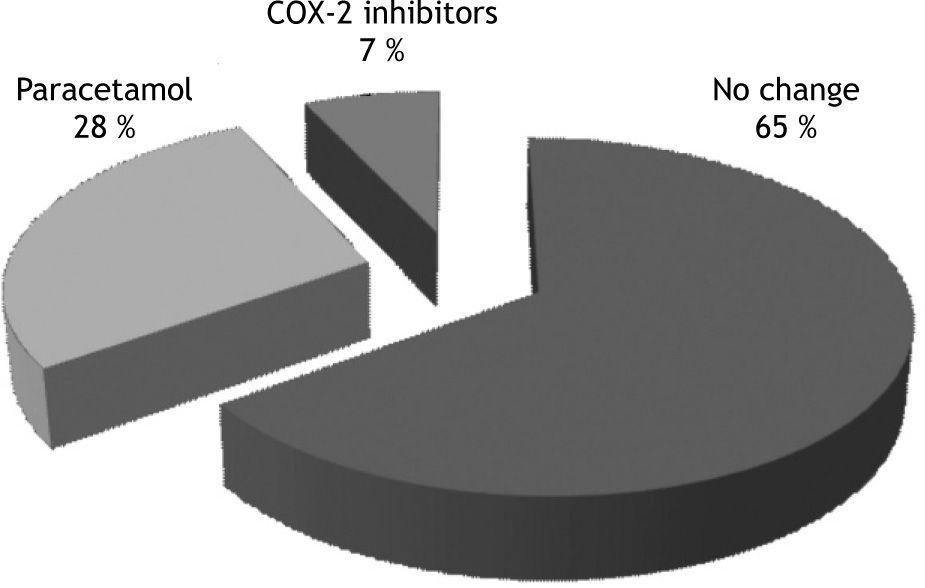
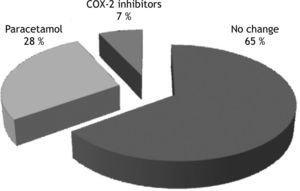
Analgesic useWhen patients were asked “Did you do any changes about your analgesic preference after your asthma diagnosis?” 85 patients (64.9 %) reported not to have any analgesic preference, whereas the remaining 46 cases (35 %) restricted their analgesic preference to certain analgesics (Fig. 2). Among those, 37 patients (80 %) reported that they preferred paracetamol following asthma diagnosis, while 9 (20 %) used COX-2 inhibitors. Among 37 patients who prefer paracetamol, 27 patients (73 %) had analgesic intolerance (AI); the remaining 10 patients (27 %) had no history of aspirin and/or NSAID related adverse effect. Eight of nine patients who used COX-2 inhibitors (meloxicam/nimesulide) had AI and used these drugs as their doctors advised after negative oral provocation tests with these drugs.
Factors effecting behaviour and attitude changesRegarding the factors affecting the compliance of the patients to the prevention measures; only higher education level was found to be related with better compliance with vaccinating against influenza (p = 0.017). Age, asthma duration and severity, higher education or having information about asthma were not related with compliance to other prevention measures.
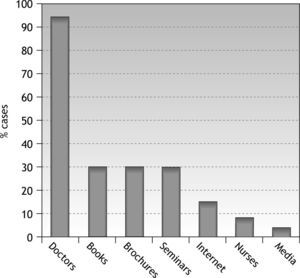
Part IIIInformation sources about asthmaWhen asked, “Where did you obtain specific knowledge and avoidance measures about asthma including asthma triggers?” (Doctors, nurses, special books or brochures for patients with asthma, asthma education seminars web, written and visual media), the majority reported to be informed about asthma primarily by their physicians (n = 119; 90.8 %) (Fig. 3). Only four patients declared that they were not informed by any educational items related to their asthma. Thirty-seven subjects (28.2 %) had participated in asthma education seminars in our department at least once.
DiscussionAlthough the importance of the environmental triggers on asthma management has been well described, this issue for adult patients with asthma seems to be neglected. Emphasizing this data, this study showed that our group of female predominant asthma patients are faced with several triggering factors regardless of the underlying severity of the disease. More importantly, preventive measures against some modifiable triggers were insufficient.
In this study, the degree of asthma severity of the individuals seemed to affect triggering factor pattern. In this sense, patients with severe asthma reported to be affected more frequently by medications such as aspirin and other NSAIDs, emotional stimulations and weather changes than the other severity degrees. Aspirin and other NSAIDs hypersensitivity have been reported to be more frequent in severe persistent asthma patients than in mild to moderate asthma.13,14 Our results also confirmed this data. Emotional stimulation was reported by more than 80 % of the severe asthma patients as asthma trigger in our study. Ritz et al. reported that emotional triggering factors were significantly associated with severity of asthma.11 In their study, Ritz et al. used short form 36 health survey questionnaire (SF 36) and showed that only psychological factors explained unique variance in the SF-36 physical and mental composite scores, and higher trigger scores were associated with lower health status. They also demonstrated that patients with more frequent experience of psychological asthma triggers represented greater airway constriction to emotional film presentations in the laboratory conditions.11 In accordance with this finding, in our study group, presence of emotional factors was significantly higher in severe asthma patients having more limited airway functions. However, we did not analyse the effect of these triggers on daily life of the patients.
On the other hand, emotional factors have significant importance not only in severe cases but also in patients with mild to moderate asthma, being over 60 %, which is higher than previously reported.3 This discrepancy could partly be explained by female predominance of our study population. In our study, female subjects were influenced more frequently by emotional stress than males. Other than emotional factors, exposure to indoor pollutants and weather changes were also other significant triggers in our cases. We may assume that as severe cases spend too much time indoors they are exposed more frequently to indoor pollutants and are more vulnerable to atmospheric changes. Recognition and management of these triggering factors among patients with asthma can be expected to improve symptoms and quality of life.15,16
In general, fewer triggers were reported in patients who were male, married, with cohabitants, and having a higher education. Moreover, higher severity of asthma was found to be associated with higher scores on a number of Asthma Trigger Inventory subscales.12 On the contrary, in our study, we did not observe any difference in varying severity degree of asthma in gender and educational level with regard to the number of triggers. This observation could be a predictor of comparable potential for the development of asthma episodes in all asthma patients with varying severity. Together with the previous findings which showed that the severity of asthma exacerbations was not related to the underlying severity of chronic disease,17 our findings particularly emphasize the vulnerable part of all asthma severities to environmental triggers. However, our data does not provide information about the effect of these triggers on asthma outcomes.
In this study, the secondary aim was to evaluate the preventive measures against major triggers subject to be modified by the patients. As previously stated, tertiary allergen avoidance was not evaluated as it is beyond the scope of this study. Firstly, regarding cigarette smoking habits, the majority of our cases never smoked. However, among the cases who were smoking at the time of asthma diagnosis, only 45 % had quitted smoking after asthma had been diagnosed. Interestingly, half of the current smokers reported environmental tobacco smoke as an asthma trigger for themselves. Actually this data emphasize that even though the smoking rate is below the developed countries' smoking ratios,18 smoking still seems to be an important health problem for patients with asthma in our country. Physicians who are dealing with asthma should ask about active or passive smoking as a part of routine checklist of nonspecific asthma triggers especially, and be supportive to quit smoking for this particular group of patients. However, although such interventions should definitely include individual components, larger policy-level interventions are often necessary as well. We hope that the new regulation in Turkey which bans smoking in all forms of public places (effective after May 19, 2008) will be helpful in this process.19
The other major preventive measure item was influenza vaccination. As patients with asthma are particularly susceptible to serious complications from influenza, we regularly advise our patients with moderate to severe asthma to take an influenza vaccination every year as suggested by international guidelines.1,2,20 But, despite the high ratio of upper airway infections, including common cold, as an asthma trigger in accordance with previous data,21 we showed that only 30 % of the patients were vaccinated against influenza regularly and only patients with higher education level tended to be vaccinated. Fear of allergic side effects of vaccination can partly explain this low rate of vaccination, but economic reasons might also have contributed as reimbursement of the vaccine was not offered by the health insurance system during the study duration. As a good progress in health system policy, the Turkish government now provides free influenza vaccines to risk groups including asthma, will be an aid to control asthma attacks caused by influenza.
Regarding analgesic preference, the majority of our cases (65 %) did not exhibit any analgesic preference because of asthma and they used any analgesics when indicated. The remaining 46 cases (35 %) restricted their analgesic preference to certain analgesics such as paracetamol (80 %) and cyclooxygenase (COX)-II (20 %) inhibitors. Avoidance of the use of aspirin and other NSAIDs is not recommended in patients with asthma without a history of adverse events to aspirin or other NSAIDs.1,2 However, as an interesting piece of data, 27 % of the patients who used paracetamol had no history of aspirin and/or NSAID related adverse effect. This observation shows that there is a tendency by Turkish physicians to prescribe paracetamol to some asthmatics regardless of the history of analgesic intolerance (AI) in our country. On the other hand, in general, for cases with asthma and AI, a structurally different drug from the culprit agent is recommended to be prescribed after its tolerability was assessed with a negative oral provocation tests.22,23 Supporting this approach, COX-2 inhibitors were advised in eight patients who had AI after a negative oral provocation test performed in our clinic.
Regarding the factors effecting behaviour and attitude changes in our particular group of asthma patients, importantly, no factors including higher educational levels or knowledge levels seemed to cause behavioural change. The majority of our group had been educated about asthma either by their physicians or by other sources. However, it is well documented that knowledge alone does not change behaviour.24 According to the theory proposed by Bandura, people can learn through observation via a live or a symbolic model, and; intrinsic reinforcement such as pride, satisfaction, and a sense of accomplishment are important to learning and finally; learning does not necessarily lead to a change in behaviour.24 In this study, we observed that our patients were highly aware about their own triggers, almost all of them had been informed about asthma; almost one third of them had participated in asthma education seminars; however their applications relating to some major triggers were insufficient according to Bandura's theory. This finding indicates the need for a different approach in the management of this issue.
In this sense, an ideal education system has been suggested to be structured, individualized, be supportive for patient's self-efficacy (our belief in our ability to succeed in specific situations), and should be repeated in certain periods.1,2,25–28 Although having knowledge does not always lead to a change in behaviour; it should be kept in mind, knowledge might have an indirect effect on asthma management through patients' ability to adapt to the disease. It has been shown that an appropriate educational programme leads to better awareness of asthma by patients25 and can reduce the number of home triggers for asthma even for low-income communities.29
The current study has a number of limitations. Firstly; regarding its self-reported nature, all definitions of triggers were open to perception of the patients. Secondly; the cross-sectional design cannot imply causality and caused a skewed population in terms of gender in this study. Owing to this, we tried to make our comment in the light of our group characteristics. Our previous trials showed that there was a female predominance in asthma cases not only in our clinic but also in other parts of Turkey14,30–32 and this pattern is also an expected finding for other nationalities.33,34 Thirdly; since the Asthma Control Test suggested by current guidelines in the management of asthma had not been validated in our country when we performed this study, we could not include such an investigation in our study materials. Instead, we used the severity of chronic asthma as a predictor of underlying degree of the disease.
In conclusion; in the present study, we showed that predominantly female adult patients with asthma had several asthma triggers which can cause asthma episodes and this feature is independent from underlying severity of asthma. Patients with severe asthma represented a special triggering pattern; female cases were more vulnerable to emotional triggers than males. Our results also confirmed that compliance to the modifiable major prevention activities was significantly insufficient and needs to be improved. New strategies to improve the awareness of the asthma patients to their own triggers and compliance to preventive measures against modifiable factors, which are also supported by health system policies when necessary, are needed. This approach might prevent asthma attacks caused by modifiable triggers.