Accidental intraarterial injection is a serious condition which, if unattended, can compromise the viability of a limb within a few hours.
ReportA 97-year-old woman developed acute critical left hand ischemia secondary to iatrogenic intrarterial injection of dexchlorfeniramine and prednisone. The initial angiogram showed the complete occlusion of the ulnar artery and the superficial palmar arch. She underwent successful thrombectomy of the ulnar artery and thrombolysis of the palmar arch, which achieved complete digital reperfusion.
DiscussionMost previously published cases report accidental arterial injections in parenteral drug abusers. There is no consensus about the ideal treatment for these events.
A injecção intra-arterial acidental é uma complicação grave que, se não tratada, pode comprometer a viabilidade de um membro em poucas horas.
Caso clínicoDoente do sexo feminino, de 97 anos de idade que desenvolveu isquémia aguda grave da mão esquerda após injecção intra-arterial iatrogénica de dexclorofeniramina e prednisona. A angiografia inicial mostrou a oclusão da artéria cubital e da arcada palmar superficial. A doente foi submetida a trombectomia da artéria cubital seguida de trombólise da arcada palmar o que permitiu recuperar a perfusão digital.
DiscussãoA maioria destes casos mais frequentemente reportados na literautura referem-se a infecção intra-arterial com contexto de abuso de drogas. Não há consenso sobre o melhor tratamento destes doentes.
Accidental intraarterial injection is a very serious condition which, if unattended, can compromise the viability of a limb within a few hours. Previously reported cases describe mostly accidental injections of different drugs in parenteral drug abusers. There is no consensus about the ideal treatment for this kind of event.
Case reportA hypertensive 97-year-old woman was transferred to our emergency room from another hospital three hours after the acute onset of cold and severe pain in her left hand. The symptoms began following injection of 5mg of dexchlorfeniramine and 60mg of prednisone in her left antecubital fossa, which were meant to treat a possible anaphylactic event secondary to an unknown analgesic.
The physical examination was difficult due to intense pain. The left brachial and radial pulses were present, the ulnar pulse was absent, and there was extreme cyanosis and absence of capillary refill in the hand.
The patient was immediately taken to the operating theatre, where, assisted by a nerve-stimulator, an axilllary block of the left brachial plexus was performed. This seemed to induce partial recovery of the pallor of the hand. A duplex scan, performed in the operating room, revealed brachial and radial artery patency but ulnar artery occlusion.
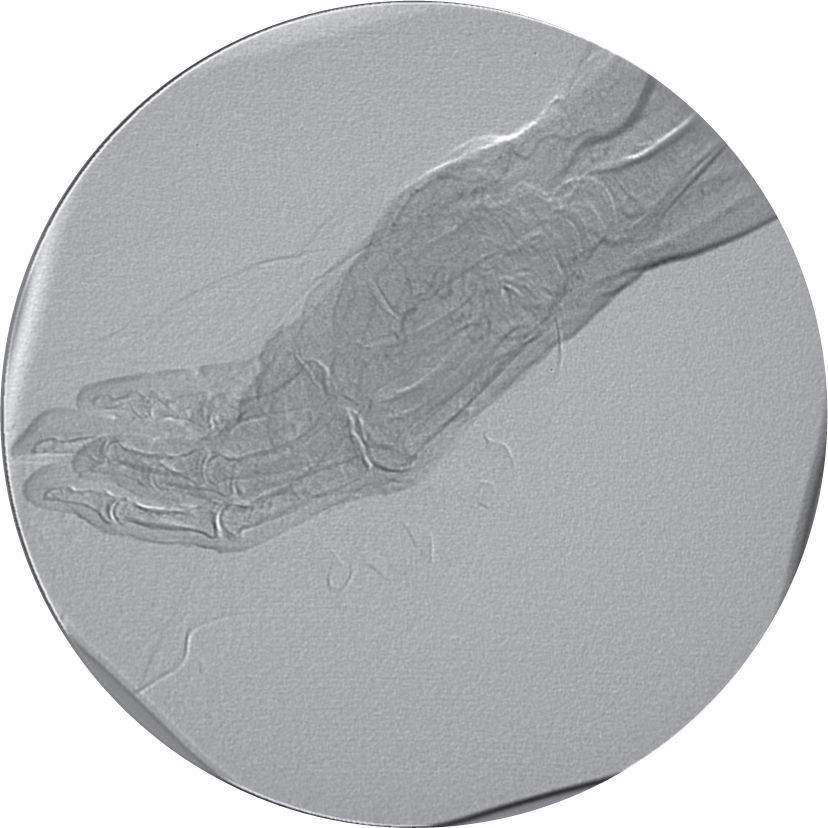
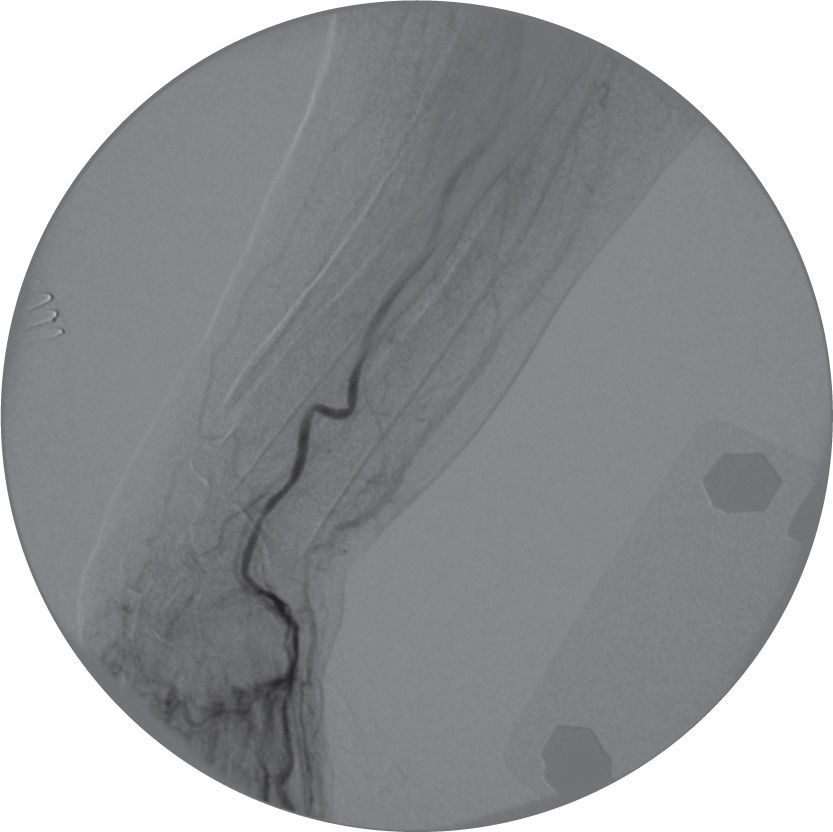
An angiogram (Fig. 1) was done, through a standard surgical approach of the brachial bifurcation. It revealed: a soft brachial artery with no atheromatous plaques; an elongated and patent radial artery, with two 180° loops; and the occlusion of both the ulnar artery and the superficial palmar arch. Following a transverse arteriotomy over the brachial bifurcation, a #3 Fogarty embolectomy catheter was introduced into the ulnar artery down to the wrist, feeling no resistance, extracting little thrombus and failing to produce any backbleeding. Next, 50000UI of urokinase were infused into the ulnar artery though a multipurpose 4F catheter. Another 50000UI were infused systemically. After 15 minutes, a new angiogram (Fig. 2) revealed that the superficial palmar arch had become patent. The patient's intense pain stopped and she recovered normal ulnar pulse and good perfusion in her hand.
A duplex scan was repeated the next day, and it confirmed radial and ulnar artery patency, with triphasic doppler signals over the interdigital arteries.
DiscussionWe do not really know the chain of events which ultimately led to what we believe was an intrarterial drug injection. The patient had a thick arm and several puncture marks on her left antecubital fossa, which suggested a difficult puncture. The fact that only the ulnar artery was occluded was also surprising. We can only speculate on a direct puncture of the proximal ulnar artery. The pathophysiological mechanisms that occur when certain intravenous drugs are injected into the arterial tree are not well known. These may be a combination of intimal damage, small vessel thrombosis and vasospasm, and may depend on the specific drug which is injected. Talc particles used to dilute heroin, can cause an additional septic process.1,2
Brachial plexus blockage was useful in the management of the present case, as it resulted in quick relief of the patient's pain, as well as beneficial vasodilation. The tortuosity of the radial artery compelled us not to navigate into it with the Fogarty catheter or the multipurpose catheter, so as to avoid damage to her single patent artery to the hand. Thus, we decided to try to recover the ulnar artery and infuse the urokinase into the palmar arch through it, a strategy which proved successful. Some previous reports have described successful treatment with intraarterial papaverin or other fibrinolytic agents,3–5 but there is still no consensus about the ideal treatment for these events.