Prosthetic graft infection is one of the most feared complications in arterial revascularization surgery. Its management is challenging, may compromise durability of reconstructions, limb viability and can pose a life-threatening condition.
Established concepts for successful management of prosthetic graft infection required total prosthetic resection, extensive tissue debridement and extra-anatomic bypass to ensure limb perfusion.
Vacuum assisted closure therapy (VAC-therapy) as adjunctive treatment for groin infections following vascular procedures, has been associated with successful treatment without graft explantation, in some published series. However, in the presence of very aggressive microorganisms may not be sufficient for a successful treatment. Staphylococcus species are the most prevalent pathogens causing vascular prosthesis infection; the introduction of more selective bacteriostatic and bactericide antibiotics with synergistic interactions and direct action on biofilm in association with VAC-therapy emerged as an experimental alternative treatment for infected functioning grafts with good early results.
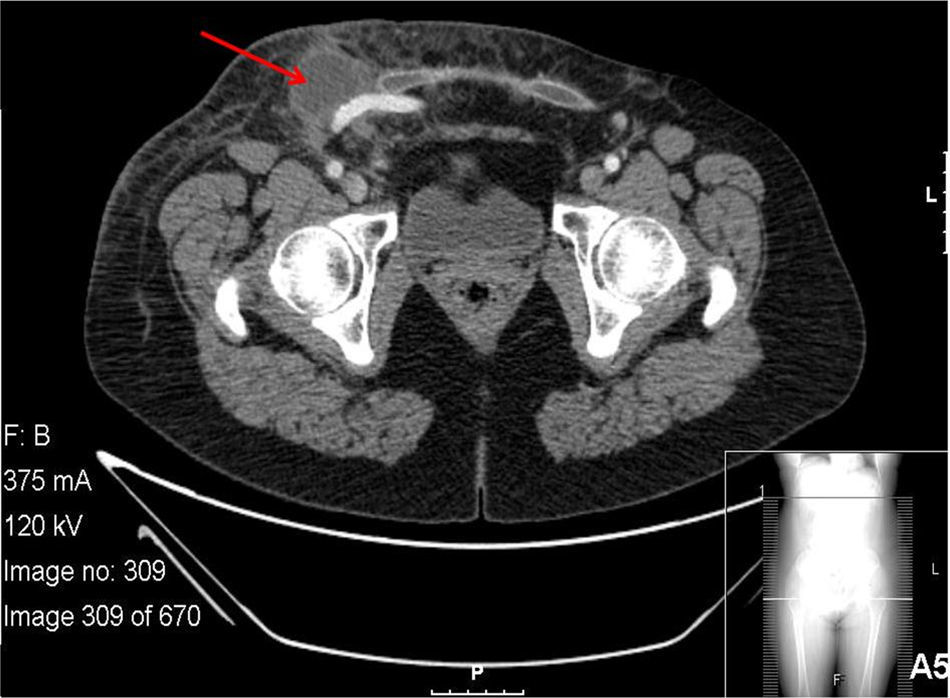
We report a case of a 45-year-old female patient, submitted to femoro-femoral bypass two months before, who was admitted at our institution with a tender mass on the right groin associated with local and systemic signs of infection. Angio-CT scan showed an occluded stent in the right iliac artery and two femoro-femoral bypasses in place with only one functioning and a 8.3cm collected abscess in the right femoral region (Fig. 1) in close contact with the prosthetics grafts. There were no signs of hemorrhage or false-aneurysms.
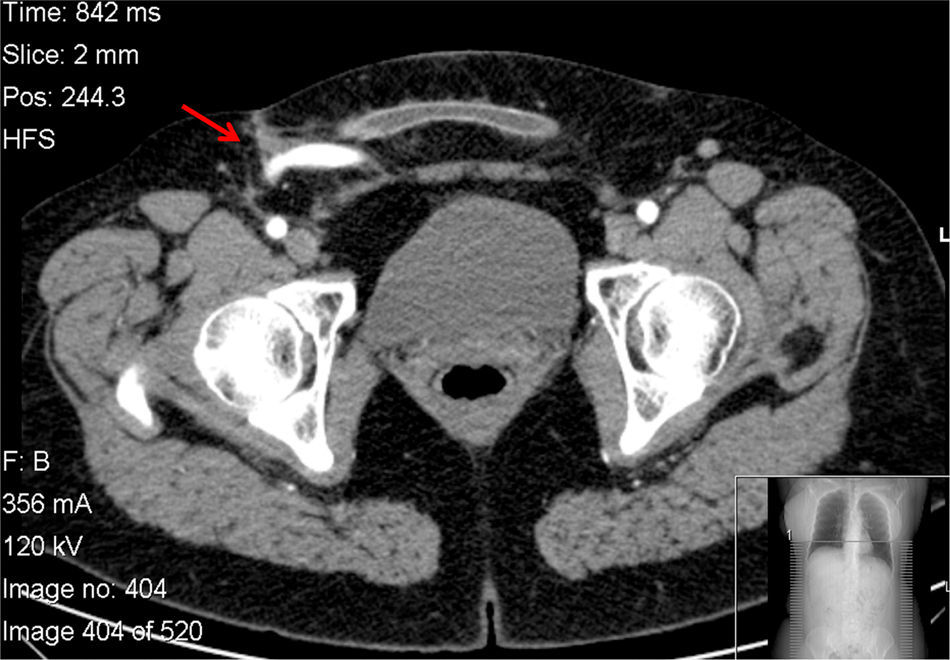
Pus was collected and gram stain and cultures were positive for methicillin sensitive Staphylococcus aureus (MSSA). The patient was submitted to conservative treatment with local surgical abscess drainage, “in situ” application of VAC-therapy and double bactericide and bacteriostatic antibiotic regimen with intravenous daptomycin and rifampicin for 3 weeks with good evolution and total remission of fever, local or systemic signs of infection (Fig. 2). The patient was maintained with oral trimetoprim-sulfametoxazol bid, for more 6 months.
Follow-up was performed at 1, 3 and 6 months, with blood tests and ecography of the right groin and at one year with a CT scan that showed no signs of prosthesis infection (Fig. 3). At 2 years follow-up she remains asymptomatic, in good health condition without signs of systemic or local infection (Fig. 4) with a patent graft and normal limb function.
Treatment with abscess drainage, VAC-therapy and oriented bactericide and bacteriostatic antibiotic regimen for S. aureus can be a safe alternative treatment of graft infections with good early results, thus delaying eventually more aggressive surgical treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.