Blunt trauma of the axillary and subclavian arteries is uncommon. Conventional surgery presents significant morbidity associated to the need of extensive exposure and challenging dissection through traumatized tissues. Endovascular treatment is an alternative that has increasingly been used in traumatic arterial injuries. This report presents three cases that were managed by endovascular techniques.
MethodsWe report the cases of three patients with blunt traumatic injuries of the subclavian and axillary arteries who were treated at our Institution in 2013 with endovascular techniques. Each case presented distinctly, resulting from different traumatic mechanisms and the therapeutical approach was adapted accordingly.
ResultsCase 1: A 68-year-old man was admitted with an acute limb ischemia of the left upper limb after a fall from his own walking height. A computerized tomography angiography demonstrated a dissection of the left subclavian artery. Resource to a proximal angioplasty with stent allowed the recovery of the limb perfusion fixating the flap. Case 2: A 34-year-old male who fell from a height of 8m, with multiple costal arch fractures and the complete transection of the subclavian artery. In this case, a covered stent excluded the rupture. Case 3: A 45-year-old woman presented to our department with an acutely ischemic left upper limb with 3 days of progression after a distension of the scapuloh-umeral articulation. Although a digital amputation was ultimately necessary, hand-salvage was accomplished through thrombectomy and catheter-directed thrombolysis.
ConclusionBlunt trauma of the axillosubclavian arteries is rare and its diagnosis may be challenging. Endovascular treatment of blunt traumatic injuries of the subclavian and axillary arteries is an alternative to traditional surgical treatment, which may be used solely or in combination with the latter to reduce invasiveness and improve outcome of arterial injuries.
O traumatismo arterial subclávio-axilar é raro, sendo a maioria das lesões produzidas por traumatismo penetrantes. A Cirurgia Convencional está associada a morbilidade significativa devido à necessidade de uma exposição extensa para obtenção de controlo vascular e devido ao risco de iatrogenia durante a dissecção cirúrgica em tecidos traumatizados. A abordagem endovascular é uma alternativa que tem vindo a ser utilizada mais frequentemente em traumatismos vasculares.
MétodosReportamos os casos de 3 doentes que foram tratados na nossa Instituição em 2013 com lesões fechadas das artérias subclávia e axilar com recurso a técnicas endovasculares. Cada caso teve uma apresentação clínica distinta, tendo resultado de mecanismo de traumatismo diferentes, e a abordagem terapêutica foi adaptada à apresentação clínica, assim como à patologia subjacente.
ResultadosCaso 1: um homem de 68 anos foi admitido com uma isquemia aguda do membro superior esquerdo após uma queda da sua própria altura com traumatismo do ombro. Uma angiografia por tomografia computorizada (AngioTC) demonstrou a dissecção da artéria subclávia. A revascularização realizada incluiu a realização de uma angioplastia da artéria subclávia com stent descoberto com fixação do flap de dissecção proximal. Caso 2: um homem de 34 anos foi vítima de uma queda de 8 metros em altura, da qual além de múltiplas fraturas de arcos costais resultou a rotura completa da artéria subclávia direita. Neste doente, foi realizada e exclusão endovascular da rotura com um stent coberto. Caso 3: uma mulher de 45 anos foi admitida com um quadro de isquemia aguda do membro superior esquerdo com 3 dias de evolução após um estiramento da articulação escapulo-umeral sem luxação de ombro ou fratura associada. Embora tenha sido necessária a realização de uma amputação digital por irreversibilidade da isquemia, a trombectomia complementada com trombólise arterial dirigida por cateter permitiu a conservação da mão.
ConclusõesO traumatismo fechado das artérias subclávia e axilar é raro e o seu diagnóstico pode ser desafiante caso não haja uma elevada suspeição clínica. As técnicas endovasculares podem ser utilizadas em alternativa ou em conjugação com a Cirurgia Convencional, reduzindo a invasibilidade e morbilidade associadas ao tratamento dos traumatismos arteriais neste território.
Acute arterial traumatic lesions involving the axillary and subclavian arteries are uncommon, accounting for 1–9% of all traumatic vascular injuries.1–5 Most cases are caused by penetrating mechanisms, with only up to 5% of these injuries produced by blunt trauma.3,6 Blunt trauma may involve multiple structures but presentation of a subclavian or axillary arterial lesion may not be clinically notorious,3 delaying diagnosis and adversely affecting patient outcome.7
Direct surgical repair of these vessels requires extensive exposure obtained through frequently traumatized tissues which is not free from complications.8 When feasible, endovascular techniques are a less invasive and also effective alternative to standard conventional surgery9 and have increasingly been applied as an alternative or complementary to surgical treatment of vascular traumatic injuries.10
The aim of this publication is to report 3 cases where presentation and management following blunt trauma of the arterial thoracic outlet differed significantly, illustrating the potential use of different endovascular armamentaria to achieve adequate revascularization.
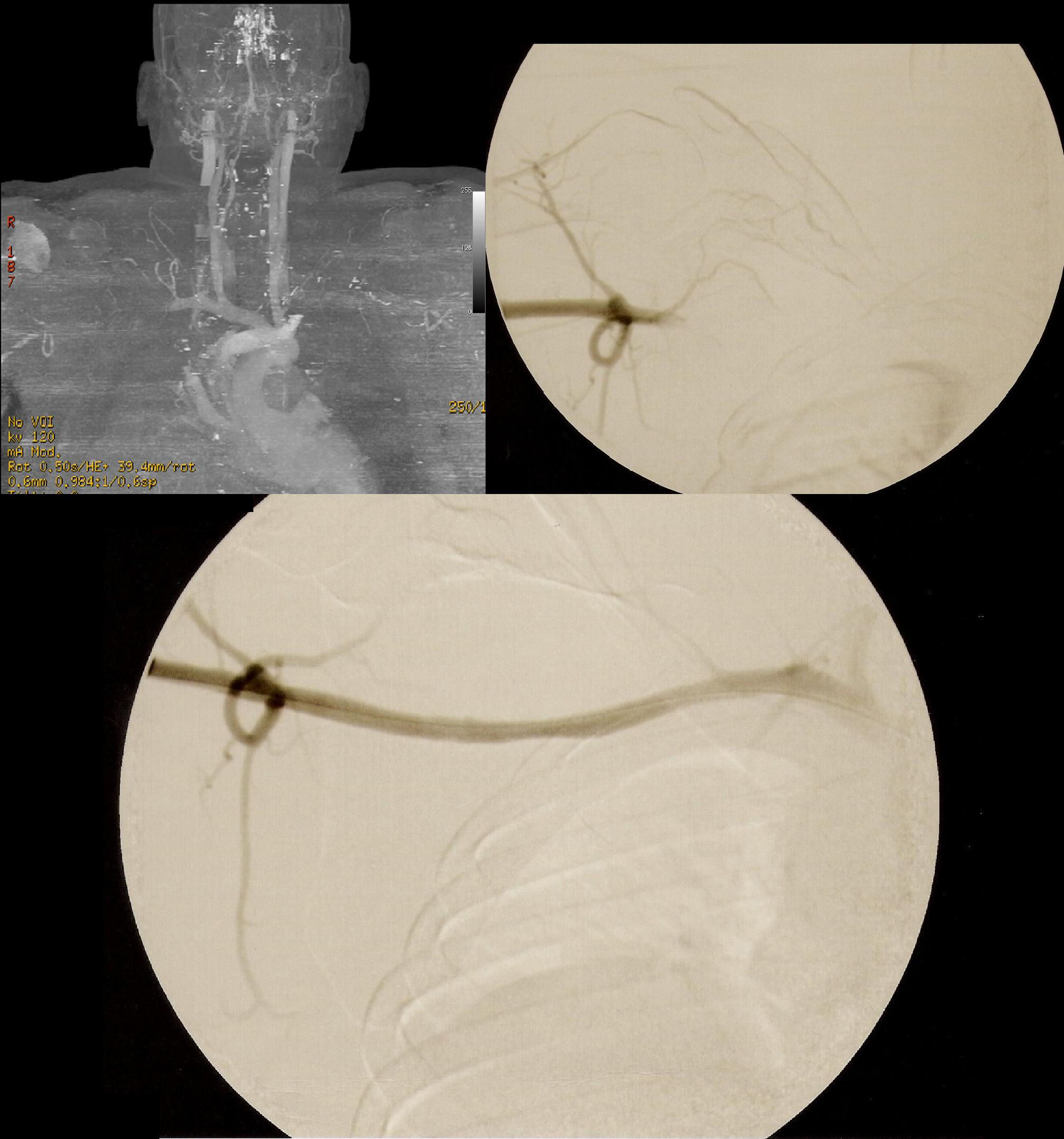
Case 1A 68-year-old man, without any relevant past medical history, was referred with acute left upper limb pain. The patient mentioned trauma of his left shoulder as a consequence of a fall from ground level, 2h before presentation. At observation, he presented with high blood pressure (170mmHg systolic), decreased temperature of the left hand and absent pulses in the upper left limb. Plain X-rays excluded bone fractures. Color-flow Doppler showed the presence of a triphasic arterial waveform in the proximal subclavian artery, a monophasic arterial waveform in the distal subclavian and axillary artery as well as an occluded brachial artery from its origin down to the elbow. A Computerized Tomography Angiography (CTA) was performed which confirmed the findings and revealed a dissected proximal subclavian artery as shown in Fig. 1.
Case 1. Top left: CTA showing distal extension of dissection to the axillary artery and occlusion of the brachial artery. Top right: Intraoperative selective digitally subtracted arteriography confirming CTA findings, diagnostic catheter placed distally to proximal dissection entry flap. Bottom: Completion arteriography.
After informed consent, a brachial artery cutdown and a right femoral percutaneous access were obtained. A diagnostic catheter was positioned in the aortic arch from the femoral access and an endovenous bolus of 5000 units of non-fractioned heparin was given. Mechanical thrombectomy of the brachial artery with a Fogarty catheter under fluoroscopic control was performed, with care not to traumatize the dissected subclavian artery. Subsequently, the dissection was crossed from brachial retrograde access through its true lumen and snared from the femoral access. Finally, one balloon-expandable bare-metal stent 10mm×60mm (Assurant® Cobalt Iliac) and one self-expanding stent 10mm×40mm (Complete SE Iliac®) were sequentially implanted at the proximal dissection site and at a secondary distal dissection flap. Completion angiography showed a persistent flow limiting dissection of the distal axillary artery and thus another self-expandable 8×40 bare-metal stent was deployed with immediate resolution of the dissection. Final 2-plan angiography excluded the persistence of flow-limiting dissection with adequate runoff to the arm (Fig. 1).
The patient was discharged 48h after the intervention under double-platelet inhibition with acetylsalicylic acid and clopidogrel for the first 30 days. From thereafter, single-platelet inhibition was continued. The patient was started on statins and anti-hypertensive drugs. After a follow-up period of 10 months, the patient was free from in-stent stenosis and all upper limb pulses were palpable and symmetric.
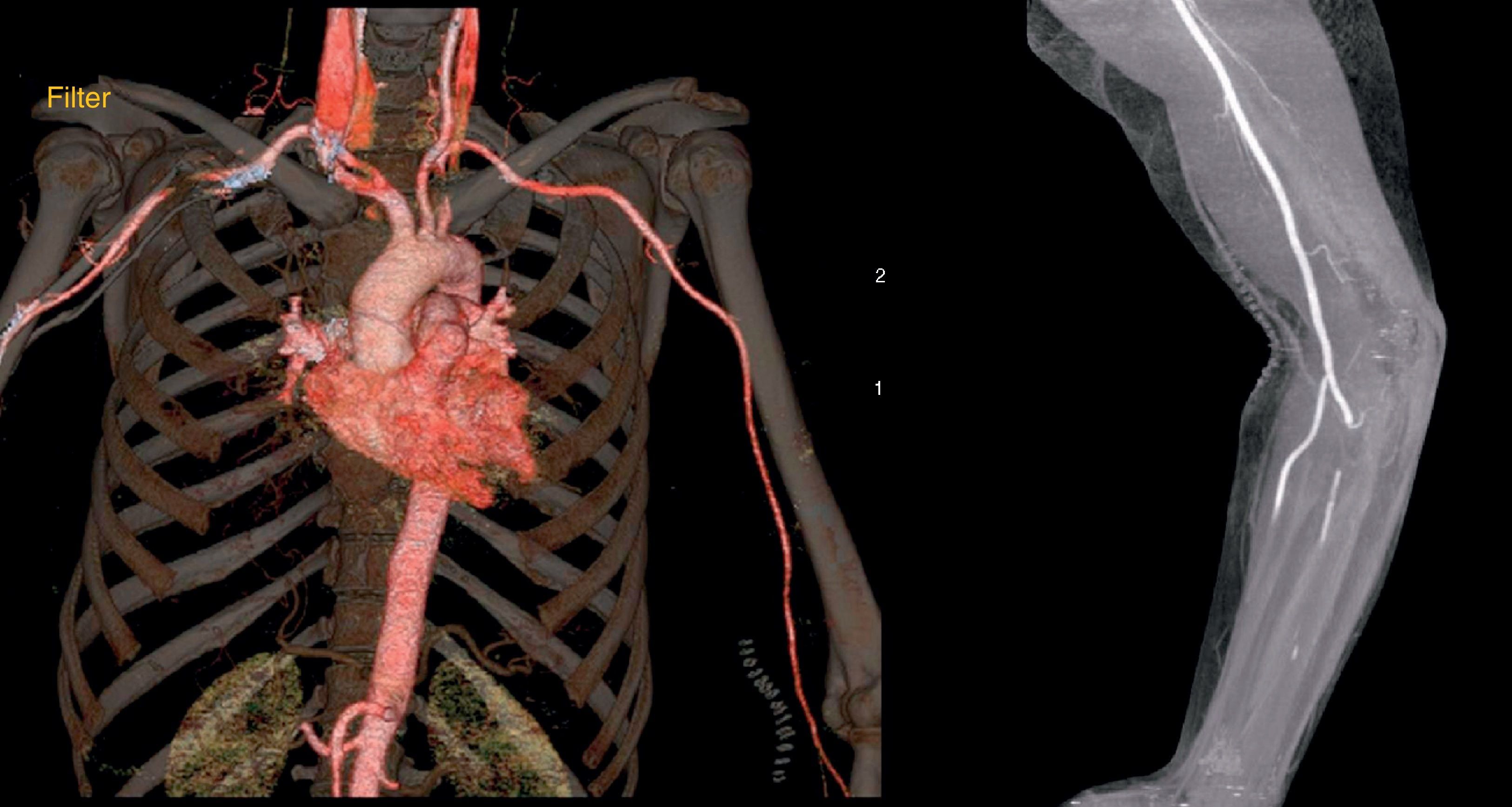
Case 2A 34-year-old man with a body-mass index of 34 and a history of endovenous drug abuse sustained a fall from a height of 8 meters. The impact point was his right hemithorax, shoulder and pelvis. On admission the patient was awake, hemodynamically stable and referred numbness and paralysis of his right upper limb. The right arm was cyanosed, cold and pulses were not palpable. Neurological exploration identified a flaccid paralysis of right upper limb with an associated Claude–Bernard–Horner Syndrome.
Plain X-rays showed only a fracture of the ischio-pubic ramus. A head and cervical CT-scan were performed and identified a hematoma that originated from the middle segment of right subclavian artery injury and occupied the whole right thoracic outlet (Fig. 2). There was also a C6 spinous process fracture.
Case 2. Top left: CTA showing large hematoma and occlusion of the distal subclavian and axillary arteries. Top right: retrograde arteriography confirming occlusion of the axillary subclavian artery. Bottom: Completion angiography showing rapid antegrade flow without evidence of endoleaks. Right vertebral artery takeoff is also observed.
Informed consent was obtained and a right brachial artery cutdown was executed along with a retrograde right femoral percutaneous access. Arteriography confirmed the middle subclavian segment rupture. Crossing of the lesion required snaring of the femoral wire from the brachial access. An ePTFE-lined stent-graft (Viabahn® Gore 9mm×100mm) was implanted excluding the lesion but preserving vertebral artery perfusion. Post-implantation balloon dilation was performed to ensure adequate proximal and distal seal. Restored anterograde direct blood flow to the right upper limb was confirmed on final arteriography, with a patent vertebral artery and absence of endoleaks (Fig. 2).
The patient recovered from ischemia, and the hematoma progressively subdued. He was discharged 5 days after intervention under single antiplatelet therapy. After 10 months of follow-up, the patient remains with palpable and symmetric upper limb pulses and is undergoing physiotherapy for neurological rehabilitation.
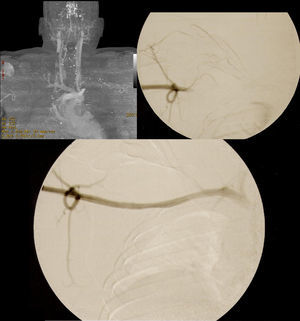
Case 3A 45-year-old female with a past medical history of arterial hypertension and non-insulin dependent diabetes mellitus, presented to the emergency department with complaints of pain, diminished strength and poikilothermia of the left upper limb. Symptoms had started after a jerk of that limb when she was attempting to move a heavy object and had progressively worsened during 3 days. Although assessed by an insurance assisting physician during those days, vascular evaluation was only sought when her forearm progressively became cyanotic and she lost hand motor function. Upon admission, left upper limb pulses were absent and cyanosis had extended to the upper third of the arm. Initial evaluation included a color Duplex-ultrasonography, which demonstrated thrombosis of the axillary, brachial, cubital and proximal radial artery.
At that time, an urgent thromboembolectomy was performed with immediate success. The patient was kept on unfractioned heparin perfusion with an aPTT goal of 60–120s. After 5h, pain recurred and palpable ulnar and radial pulses were again lost. A CTA was performed and identified nearly occlusive thrombosis of the proximal subclavian artery (Fig. 3). In addition, distal thrombosis of the ulnar and radial arteries was observed. A second thrombectomy was performed under fluoroscopic guidance and after intraoperative arteriography confirmed permeability from the distal subclavian artery to the palmar arch; a thrombolysis catheter was positioned in the proximal subclavian artery to resolve residual thrombus present at that location. A bolus of 2mg of recombinant tissue plasminogen activator (rtPA) was given and an infusion of rtPA was started at a rate of 2mg/h. Heparin perfusion was reduced to 600UI/h, and fibrinogen was controlled periodically according to department protocol. Despite initial clinical improvement with significant pain relief, after 24h, pain had worsened. The whole hand and the forearm were then cyanosed and no arterial flux was detected on continuous Doppler. An arteriography confirmed resolution of the thrombotic lesion of the proximal subclavian artery but ulnar and radial arteries had rethrombosed. A third thrombectomy was required and the thrombolytic catheter was positioned selectively in the ulnar artery. Infusion rate of rtPA and unfractioned heparin were maintained. Thrombolysis was suspended after 72h and, despite anticoagulation there was confinement of ischemic signs to the 2nd and 4th fingers which progressed to irreversible necrosis and were amputated.
The patient was sent home after 24 days of hospitalization due to infection of the amputations. At discharge, distal pulses were not palpable but bitonal waveforms on continuous Doppler were present and the surgical wounds were healing well. The patient was started on oral anticoagulation with warfarin with an international normalized ratio goal of 2–3. Thrombophilia was excluded by laboratorial and genetic workup. After 7 months of follow-up, surgical wounds have all healed and the patient has resumed functional rehabilitation.
DiscussionBlunt trauma of the subclavian and axillary arteries is uncommon and may present differently.11,12 The subclavian artery is particularly protected by an important muscular-skeletal-ligamentous apparatus formed by the subclavius muscle, the clavicle, the first rib, the deep cervical fascia and the costo-coracoid ligament.13 For this reason, most blunt lesions of the subclavian artery resulting from downward forces applied to the thorax require involvement of great energies and are associated with important bone or soft tissue injuries in the majority of cases.14 In cases where an upward force is applied on the chest, the subclavian artery may be pinched between the rib and the clavicle, causing distal subclavian or axillary lesions. Additionally, the axillary and subclavian arterial axis is prone to stretch/traction forces that may result from shear/deceleration trauma or from isolated shoulder impact.3,7 Resulting arterial injuries may be proximal, and not associated to bone or soft tissue lesions. These types of forces may explain the pathophysiology of the lesions found in cases 1 and 3 of our report. Additionally, in both cases, atherosclerotic risk factors were identified and therefore, resulting intimal thickening may also have some importance on the development of the arterial lesion.
Diagnosis of acute arterial injury may not pose a great challenge in the presence of ominous findings such as first rib fracture, diminished or absent upper limb pulses, palpable supraclavicular hematoma, widened mediastinum on chest roentgenogram, brachial palsy or severe bleeding in penetrating trauma.13 Nevertheless a vascular lesion may be present without these findings.12 Furthermore, other associated injuries may divert attention from limb perfusion resulting in delayed recognition of arterial lesions. An arterial injury should always be suspected in the presence of a brachial-ankle index below 0.9.12 In case 3 of our report, a delay of 3 days between the traumatic event and patient presentation with an immediately threatened ischemic limb had a negative impact on clinical outcome.
In a trauma setting, diagnostic exams may be performed if the patient is hemodynamically stable, and provide valuable information. Plain chest and neck roentgenograms may give away the presence of a hemothorax or a mediastinal hematoma besides associated bone fractures. Color-flow Doppler may provide accurate hemodynamic characterization of the axillary and subclavian axis. However, associated traumatic lesions and inaccessibility of the proximal segment of the subclavian artery are limiting factors. Currently, angiography has been replaced by multidetector CTA. Increased availability in most trauma centers, accurate diagnosis regarding vascular pathology (sensitivities of 97–99.3% and specificities 87.1–99.8%) and detection of associated lesions of the surrounding structures have turned CTA into the diagnostic exam of choice.15,16 Extreme cases with hemodynamic instability may be transferred to the operating theater and surgically explored, or a diagnostic angiography may be performed on-table, followed by exploration or endovascular repair, as necessary.
Complex surgical access and limited collective experience make the management of axillary and subclavian arterial lesions particularly challenging.17,18 Vascular repair may require extensive paraclavicular incisions for control; dissection though hematoma-distorted planes is feasible but not without a significant risk of neurovascular injury and significant hemorrhage.21 In comparison, endovascular treatment is a safe and attractive alternative to conventional surgery in trauma patients.17,19
Endovascular repair has been defended as the first choice of treatment for stable patients17 however, appropriate patient selection for endovascular approach is critical.20 Indications for potential endovascular repair include pseudoaneurysm, arteriovenous fistula, first-order branch vessel injury/avulsion, arterial intimal flap and focal arterial injury.21 Active uncontrollable hemorrhage, limb-threatening ischemia, airway or brachial plexus compression, concomitant aero-digestive injuries or infected wounds have all been cited as contraindications for endovascular management.17 Additionally, arteriographic contraindications include excessive luminal discrepancy between the proximal and distal arterial involvement site, inability to cross the lesion with a guidewire17 and acute occlusion.22 Other limitations reported regarding endovascular treatment are complete vessel transection, involvement of critical branch vessels and distal axillary involvement.21 However, many discrepancies can be found between reports on exclusion criteria. Also, the creation of a brachial-femoral wire has allowed the treatment of complex lesions such as completely transected and occluded arteries.23 In case 2, after a failed attempt of crossing the lesion in a retrograde fashion, a femoral percutaneous access was obtained and a snare was performed successfully, as described by others.23 Regarding hemodynamically unstable patients, proximal balloon occlusion has been successfully used for hemorrhage control prior to a definitive repair24 and may still allow further wire advancement and lesion crossing and treatment.23 Failure to obtain lesion exclusion due to proximal and distal luminal mismatch is a concern. The axillosubclavian axis is very elastic and prone to extreme spasm in response to injury and poor distal perfusion and so preoperative valorization is difficult. Further, a luminal discrepancy cutoff for endovascular treatment exclusion is yet to be quantitatively established.
Primary success (defined as complete exclusion of the lesion and restoration of anterograde blood flow without flow-limiting stenosis) in 100% of cases has been reported on an intention-to-treat analysis in small series.17,22,23,25 However, Carrick et al. reported a primary success in only 3 in 8 endovascular treated patients. Two of these cases were misdiagnosed and indication for treatment was withdrawn after angiography, one other patient became hemodynamically unstable during lesion crossing with the wire and had his endovascular repair deferred to the next day after proximal balloon occlusion and appropriate resuscitation. In another patient anterograde crossing of the lesion failed and conversion to open surgery took place and finally in one other patient failure to exclude the lesion occurred due to inadequate proximal sealing.24 Danetz et al. on a retrospective analysis determined endovascular feasibility in 17 of 46 axillosubclavian vascular injuries.21 However, long lesions, total or subtotal transections that have been successfully treated in other reports23 were considered contraindications in this report.
The main setbacks of endovascular treatment are treatment-related early thromboembolic events and the uncertain long-term outcome particularly in young patients, which are more frequently involved in trauma.17 Neointimal hyperplasia with consequent late stenosis and occlusion regarding non-traumatic disease affecting other territories is well documented but extrapolation to the traumatic setting may not be linear.22 A 32% of significant in-stent stenosis or occlusion was reported in a group of 25 patients who had a mean follow-up period of 49 months.17 Importantly, those 8 patients with significant stenosis or occlusion did not present limb-threatening ischemia and the 3 occluded stent-grafts showed no structural defects. In addition, those patients who were treated were amenable to endovascular correction of the underlying pathology.17 Another report found a 14.2% rate of stenosis over a mean follow-up time of 22.6 months, and no treatment was deemed necessary in this single patient.24 Also, in regard to outcome, one-year exclusion rate of the arterial injury was 90% and freedom from bypass was 100% in another report.26
We acknowledge that self-expandable stents, due to their memory force and elasticity, are to be preferred in the management of traumatic subclavian or axillary arterial lesions if bare-metal stent implantation is indicated. These vessels are extremely elastic and highly mobile, which are also prone to external compressive forces from the structures forming thoracic outlet that may ultimately lead to stent deformity/fracture. However, in case 1, a balloon-expandable stent was preferred to enhance deployment accuracy, which was deemed necessary to securely treat a near ostial proximal dissection entry site of the left subclavian artery. Although balloon-expandable stents have been consistently associated to increased risk of fracture25,27–29 self-expanding stents are also not free from risk of fracture as reported by Phipp et al.30
ConclusionClinical presentation of traumatic axillosubclavian lesions may be subtle and result from apparently unsuspicious mechanisms delaying diagnosis with a hazardous impact on patient outcome. Endovascular management of traumatic lesions of the subclavian and axillary arteries, alone or in combination with open surgery is safe and results in less invasiveness and surgical trauma. However, experience and follow-up are limited and more evidence is still required to access long-term outcomes of this type of treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Patients’ data protectionWe followed our institution's protocols.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.