Hepatic encephalopathy (HE) is a common complication in cirrhotics and is associated with an increased healthcare burden. Our aim was to study independent predictors of 30-day readmission and develop a readmission risk model in patients with HE. Secondary aims included studying readmission rates, cost, and the impact of readmission on mortality.
Materials and methodsWe utilized the 2013 Nationwide Readmission Database (NRD) for hospitalized patients with HE. A risk assessment model based on index hospitalization variables for predicting 30-day readmission was developed using multivariate logistic regression and validated with the 2014 NRD. Patients were stratified into Low Risk and High Risk groups. Cox regression models were fit to identify predictors of calendar-year mortality.
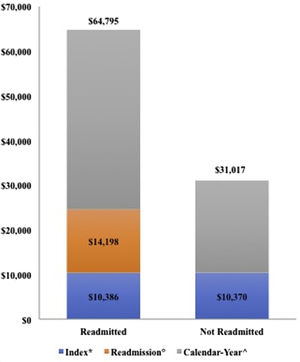
ResultsOf 24,473 cirrhosis patients hospitalized with HE, 32.4% were readmitted within 30 days. Predictors of readmission included presence of ascites (OR: 1.19; 95% CI: 1.06–1.33), receiving paracentesis (OR: 1.43; 95% CI: 1.26–1.62) and acute kidney injury (OR: 1.11; 95% CI: 1.00–1.22). Our validated model stratified patients into Low Risk and High Risk of 30-day readmissions (29% and 40%, respectively). The cost of the first readmission was higher than index admission in the 30-day readmission cohort ($14,198 vs. $10,386; p-value <0.001). Thirty-day readmission was the strongest predictor of calendar-year mortality (HR: 4.03; 95% CI: 3.49–4.65).
ConclusionsNearly one-third of patients with HE were readmitted within 30 days, and early readmission adversely impacted healthcare utilization and calendar-year mortality. With our proposed simple risk assessment model, patients at high risk for early readmissions can be identified to potentially avert poor outcomes.
Hepatic encephalopathy (HE) is a common complication of cirrhosis with a prevalence of 30–45% and is associated with recurrent episodes [1,2]. Hepatic encephalopathy is responsible for nearly 0.33% of all hospitalizations in the United States, with a yearly inpatient mortality rate of 7–15.6% [1,2]. Development of HE is a poor prognostic factor, associated with low 1-year (20–50%) and 3-year (15–23%) survival rates. Additionally, patients with overt HE at the time of waitlist registration for liver transplantation have a significantly higher risk of 90-day mortality than cirrhosis patients without HE [1,3].
The management of cirrhosis patients hospitalized with HE carries a substantial economic burden. Data from a Nationwide Inpatient Sample (NIS) study on the economic burden of HE revealed annual national costs of $4.67 to $7.24 billion for HE-related hospitalizations, with individual inpatient costs of $46,000 to $63,000. Severity of illness and the number of procedures (paracentesis and esophagogastroduodenoscopy [EGD]) per admission were reported to be the most important predictors of mortality [2].
Given the economic burden of hospital readmissions, the Patient Protection and Affordable Care Act (ACA) instituted the Readmission Reduction Program that required the Centers for Medicare and Medicaid (CMS) to reduce payment for hospitals with higher readmission rates [4]. Roughly one-quarter of cirrhotics are readmitted after discharge within 30 days [5,6]. Smaller studies have reported readmission rates of 17–38% after hospitalization for HE [1,5–13]. Readmissions not only put these patients at risk for infections, but also increase their morbidity and mortality [14,15]. The cost of readmissions and the toll of their healthcare utilization is vast [16]. However, the 30-day readmission rate, its risk factors and costs in patients with HE have not been studied in a large population database. Therefore, we sought to develop and validate a risk model for 30-day readmissions in patients with HE based on variables derived from index admission using the largest publically available all-payer nationally representative database in the United States. We also studied the impact of 30-day readmission in patients with HE on calendar year mortality.
2Materials and methods2.1Data sourceWe utilized the 2013 Nationwide Readmission Database (NRD), developed by the Agency for Healthcare Research and Quality (AHRQ) as part of the Healthcare Cost and Utilization Project (HCUP) for our study. The NRD is a publically available database of all-payer hospital inpatient stays, with patients from the State Inpatient Databases. The NRD includes data from 21 geographically distributed states, representing 49.3% of the US citizen population, as well as 49.1% of all hospitalizations. Patient-linkage numbers are able to track individual patients (while following stringent privacy regulations) across institutions within each state, allowing the database to include all discharge records from the included hospitals [17].
The 2013 NRD database was queried using validated International Classification of Diseases, Ninth Edition Clinical Modification (ICD-9-CM) codes to define variables of interest. Hospitalizations for HE were selected using the ICD-9-CM diagnostic code 572.2 [18]. The “cases” were defined as those with a principle discharge diagnosis of HE and a secondary diagnosis of cirrhosis who were readmitted within 30 days, whereas the “control” group was defined as those with a principle discharge diagnosis of HE and a secondary diagnosis of cirrhosis who were not readmitted. Discharges between January 1st and November 30th were included to allow for a minimum 30-day follow-up prior to the end of the calendar year. ICD-9-CM codes that were queried are located in Supplemental Table 1.
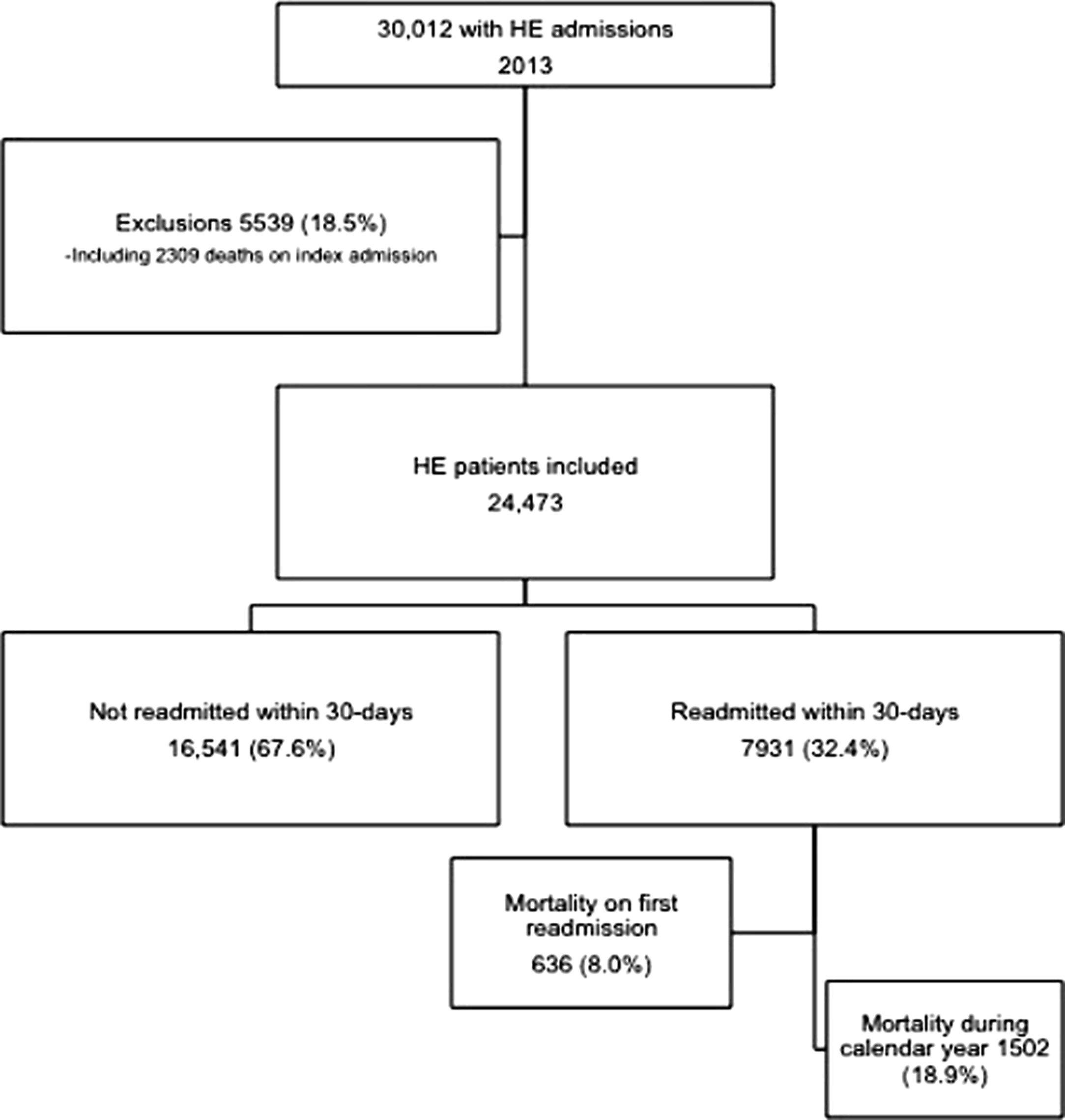
The following exclusions were applied: (a) age ≤17 years, (b) all codes describing status of pregnancy, (c) December admissions, (d) end-stage renal disease, (e) cerebrovascular disease, (f) post-liver transplantation, (g) transjugular intrahepatic portosystemic shunts (TIPS), and (h) missing information on length of stay or readmission (Fig. 1). Patients with index hospitalization mortality (n=2309) were also excluded. Given the nature of the NRD, this study was exempt from review by The Ohio State University Institutional Review Board.
2.2Patients and outcomesPatient characteristics included age, gender, and type of insurance. Race and ethnicity are not available in the NRD. Hospital characteristics (rural, urban non-teaching, urban teaching) and hospital size (small, medium, large) were based on an HCUP algorithm. Comorbidities were quantified according to the Elixhauser comorbidity index and stratified into <4 or ≥4 comorbidities (modified to exclude liver disease) [19]. Mortality was defined as index (death during index admission) or calendar-year (death during any hospitalization during the calendar-year other than index admission).
ICD-9-CM codes from previously published papers were used to capture patients with HE and cirrhosis [18]. Etiology of cirrhosis, in-hospital procedures (paracentesis, EGD, mechanical ventilation) and in-hospital complications (acute kidney injury [AKI], hyponatremia, ascites, variceal bleed, and spontaneous bacterial peritonitis [SBP]) were also included. Disposition, length of stay, and costs (index admission, 30-day readmission, and calendar-year totals) were analyzed. All causes of readmission were compiled by ICD-9-CM frequency, and the ten most common causes were noted. Liver-related causes of readmission were determined by aforementioned ICD-9-CM coding. Two authors (AK and FA) separately reviewed the list of causes of readmission. All conflicts were resolved after discussion and review with KM.
We identified the incidence, causes, and predictors of 30-day readmissions in patients hospitalized with HE. Predictive variables from index admission were used to derive a risk model for 30-day readmission. This risk model was validated with the 2014 NRD database. Finally, we also studied the impact of 30-day readmission on overall cost and calendar year mortality.
2.3Statistical analysisIndex admission patient and hospital characteristics were compared between patients readmitted vs. not within 30 days using chi-squared tests (categorical) and Student t-tests (continuous variables). To determine the independent predictors of 30-day readmission a logistic regression model was fit; similarly, Cox proportional hazards regression was used to determine predictors of calendar-year mortality. Odds ratios (OR) or hazard ratios (HR), as appropriate, and 95% confidence intervals (CI) summarize the models. Terms included in both the logistic regression and Cox proportional hazards models were determined through the use of stepwise selection where the variables eligible for inclusion were: age, gender, type of insurance, income, Elixhauser index, hospital size, hospital type, etiology of cirrhosis, paracentesis, EGD, mechanical ventilation, AKI, variceal bleed, SBP, hyponatremia, ascites, constipation, length of stay, disposition, and 30-day readmission (for the Cox model only). A Kaplan–Meier curve further demonstrated the survival differences between patients with and without 30-day readmission.
After identifying significant independent predictors of readmission (p-value ≤0.05), a risk-scoring model based on these variables was derived. The weights for each variable were determined by taking each coefficient from the logistic regression and rounding to the nearest whole number after multiplying by 10. The risk score is then calculated by summing the values for each individual parameter. The model was validated with the NRD 2014 data. Statistical significance was defined by a p-value <0.05 and all analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC) with survey procedures to produce national estimates.
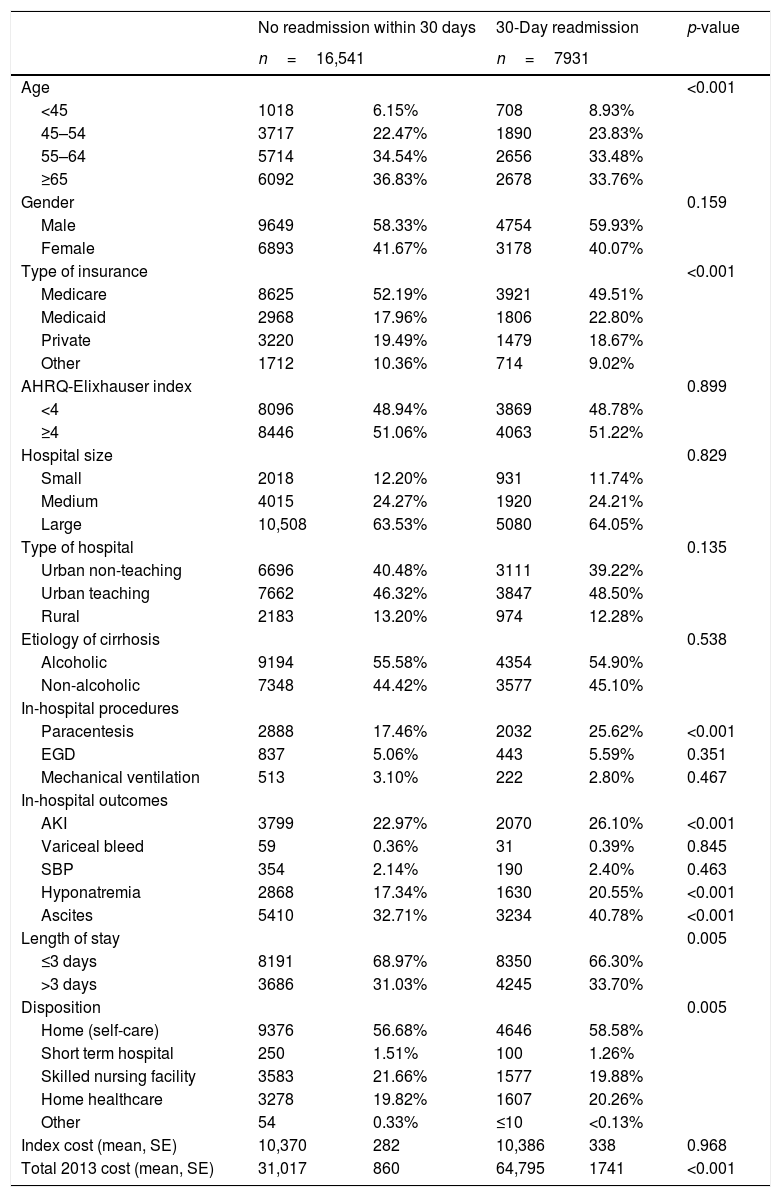
3Results3.1Baseline characteristicsA total of 333,452 patients were admitted with cirrhosis in 2013. Of the 24,473 (7.34%) patients hospitalized with HE, 7931 (32.4%) patients were readmitted within 30 days. Out of all patients readmitted within 30 days, 33.9% were readmitted with HE. Among patients readmitted within 30 days, 1762 (22.2%) were readmitted more than one time during the calendar-year. The mean age of the study cohort was 60.5±0.14 years, with 58.9% males. On univariate analysis (Table 1, Supplemental Table 2), the patients readmitted within 30 days were more likely to be younger; possess Medicaid insurance; undergo paracentesis; develop AKI, hyponatremia, ascites; have prolonged hospitalizations; differences in ultimate disposition; and higher calendar-year costs.
Baseline characteristics of patients readmitted and not readmitted within 30 days with hepatic encephalopathy.
| No readmission within 30 days | 30-Day readmission | p-value | |||
|---|---|---|---|---|---|
| n=16,541 | n=7931 | ||||
| Age | <0.001 | ||||
| <45 | 1018 | 6.15% | 708 | 8.93% | |
| 45–54 | 3717 | 22.47% | 1890 | 23.83% | |
| 55–64 | 5714 | 34.54% | 2656 | 33.48% | |
| ≥65 | 6092 | 36.83% | 2678 | 33.76% | |
| Gender | 0.159 | ||||
| Male | 9649 | 58.33% | 4754 | 59.93% | |
| Female | 6893 | 41.67% | 3178 | 40.07% | |
| Type of insurance | <0.001 | ||||
| Medicare | 8625 | 52.19% | 3921 | 49.51% | |
| Medicaid | 2968 | 17.96% | 1806 | 22.80% | |
| Private | 3220 | 19.49% | 1479 | 18.67% | |
| Other | 1712 | 10.36% | 714 | 9.02% | |
| AHRQ-Elixhauser index | 0.899 | ||||
| <4 | 8096 | 48.94% | 3869 | 48.78% | |
| ≥4 | 8446 | 51.06% | 4063 | 51.22% | |
| Hospital size | 0.829 | ||||
| Small | 2018 | 12.20% | 931 | 11.74% | |
| Medium | 4015 | 24.27% | 1920 | 24.21% | |
| Large | 10,508 | 63.53% | 5080 | 64.05% | |
| Type of hospital | 0.135 | ||||
| Urban non-teaching | 6696 | 40.48% | 3111 | 39.22% | |
| Urban teaching | 7662 | 46.32% | 3847 | 48.50% | |
| Rural | 2183 | 13.20% | 974 | 12.28% | |
| Etiology of cirrhosis | 0.538 | ||||
| Alcoholic | 9194 | 55.58% | 4354 | 54.90% | |
| Non-alcoholic | 7348 | 44.42% | 3577 | 45.10% | |
| In-hospital procedures | |||||
| Paracentesis | 2888 | 17.46% | 2032 | 25.62% | <0.001 |
| EGD | 837 | 5.06% | 443 | 5.59% | 0.351 |
| Mechanical ventilation | 513 | 3.10% | 222 | 2.80% | 0.467 |
| In-hospital outcomes | |||||
| AKI | 3799 | 22.97% | 2070 | 26.10% | <0.001 |
| Variceal bleed | 59 | 0.36% | 31 | 0.39% | 0.845 |
| SBP | 354 | 2.14% | 190 | 2.40% | 0.463 |
| Hyponatremia | 2868 | 17.34% | 1630 | 20.55% | <0.001 |
| Ascites | 5410 | 32.71% | 3234 | 40.78% | <0.001 |
| Length of stay | 0.005 | ||||
| ≤3 days | 8191 | 68.97% | 8350 | 66.30% | |
| >3 days | 3686 | 31.03% | 4245 | 33.70% | |
| Disposition | 0.005 | ||||
| Home (self-care) | 9376 | 56.68% | 4646 | 58.58% | |
| Short term hospital | 250 | 1.51% | 100 | 1.26% | |
| Skilled nursing facility | 3583 | 21.66% | 1577 | 19.88% | |
| Home healthcare | 3278 | 19.82% | 1607 | 20.26% | |
| Other | 54 | 0.33% | ≤10 | <0.13% | |
| Index cost (mean, SE) | 10,370 | 282 | 10,386 | 338 | 0.968 |
| Total 2013 cost (mean, SE) | 31,017 | 860 | 64,795 | 1741 | <0.001 |
AHRQ: Agency for Healthcare Research and Quality; EGD: esophagogastroduodenoscopy; AKI: acute kidney injury; SBP: spontaneous bacterial peritonitis; SE: standard error.
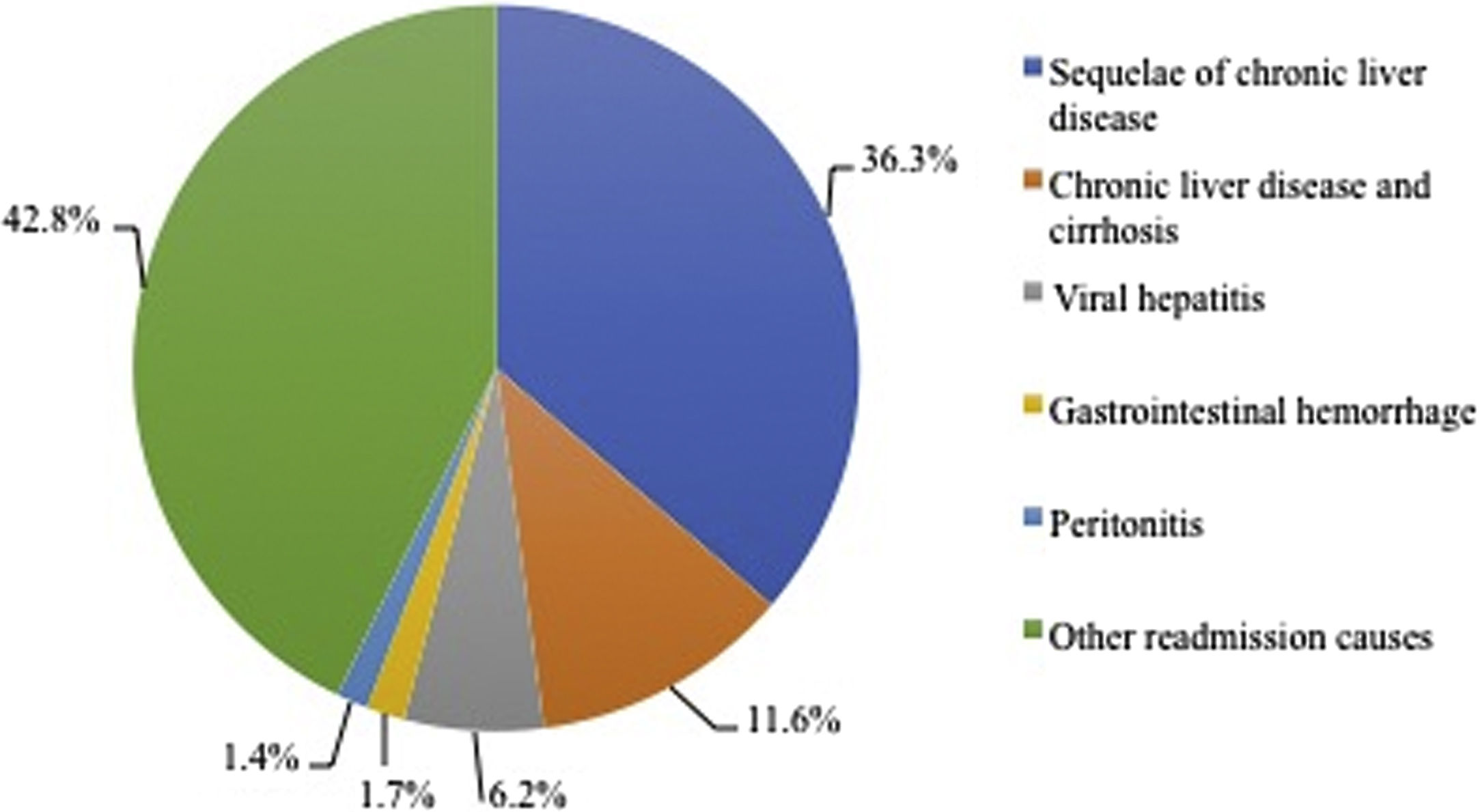
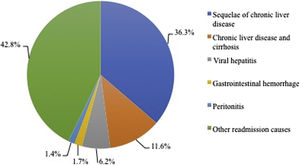
Of the top 10 most frequent causes of readmissions (which encompassed 71% of all readmissions), five were due to liver-related etiologies. They included sequelae of chronic liver disease (36.3%), chronic liver disease & cirrhosis (11.6%), viral hepatitis (6.2%), gastrointestinal hemorrhage (1.7%) and SBP (1.4%) (Supplemental Figure 1).
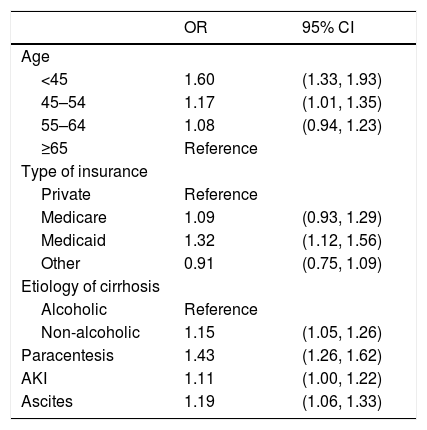
3.2Risk model for 30-day readmissionOn multivariable logistic regression analysis (Table 2, Supplemental Table 3), age groups of <45 years (OR: 1.60; 95% CI: 1.33–1.93) and 45–54 years (OR: 1.17; 95% CI: 1.01–1.35), Medicaid insurance (OR: 1.32; 95% CI: 1.12–1.56), non-alcoholic etiology of cirrhosis (OR: 1.15; 95% CI: 1.05–1.26), receiving paracentesis (OR: 1.43; 95% CI: 1.26–1.62), AKI (OR: 1.11; 95% CI: 1.00–1.22), and presence of ascites (OR: 1.19; 95% CI: 1.06–1.33) were all predictors of 30-day readmission in patients with HE.
Multivariable analysis of predictors for 30-day readmission in patients with hepatic encephalopathy.
| OR | 95% CI | |
|---|---|---|
| Age | ||
| <45 | 1.60 | (1.33, 1.93) |
| 45–54 | 1.17 | (1.01, 1.35) |
| 55–64 | 1.08 | (0.94, 1.23) |
| ≥65 | Reference | |
| Type of insurance | ||
| Private | Reference | |
| Medicare | 1.09 | (0.93, 1.29) |
| Medicaid | 1.32 | (1.12, 1.56) |
| Other | 0.91 | (0.75, 1.09) |
| Etiology of cirrhosis | ||
| Alcoholic | Reference | |
| Non-alcoholic | 1.15 | (1.05, 1.26) |
| Paracentesis | 1.43 | (1.26, 1.62) |
| AKI | 1.11 | (1.00, 1.22) |
| Ascites | 1.19 | (1.06, 1.33) |
OR: odds ratio; CI: confidence interval; AKI: acute kidney injury.
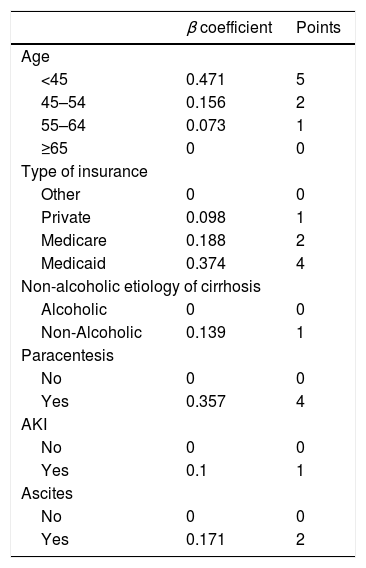
Based on these predictors of readmission, a novel scoring system to stratify a patient's risk of readmission was generated (Table 3). Patients were stratified into Low Risk (0–6 points) and High Risk (7–19 points) groups. Those in the Low Risk group had a 29.1% risk of readmission, whereas the High Risk group had a 40% readmission risk (p-value <0.001). Compared to those with Low Risk, patients in the High Risk group had 1.65 times the odds of readmission (95% CI: 1.51, 1.80).
Risk score stratification for prediction of 30-day readmission in patients with hepatic encephalopathy.
| β coefficient | Points | |
|---|---|---|
| Age | ||
| <45 | 0.471 | 5 |
| 45–54 | 0.156 | 2 |
| 55–64 | 0.073 | 1 |
| ≥65 | 0 | 0 |
| Type of insurance | ||
| Other | 0 | 0 |
| Private | 0.098 | 1 |
| Medicare | 0.188 | 2 |
| Medicaid | 0.374 | 4 |
| Non-alcoholic etiology of cirrhosis | ||
| Alcoholic | 0 | 0 |
| Non-Alcoholic | 0.139 | 1 |
| Paracentesis | ||
| No | 0 | 0 |
| Yes | 0.357 | 4 |
| AKI | ||
| No | 0 | 0 |
| Yes | 0.1 | 1 |
| Ascites | ||
| No | 0 | 0 |
| Yes | 0.171 | 2 |
AKI: acute kidney injury.
Risk stratification for risk of readmission: Low Risk (0–6; 29.1%), High Risk (7–19; 40%).
The performance of this scoring system was validated in the 2014 NRD (Supplemental Table 4). Logistic regression analyses of the odds of readmission in the 2014 validation cohort resulted in (OR: 1.65; 95% CI: 1.51–1.82) which was similar to that of the 2013 cohort. The percent of patients readmitted in the validation and test cohorts were nearly identical, as the 2014 NRD cohort Low Risk group also had a 29% risk of readmission and the High Risk group had a 40% readmission risk.
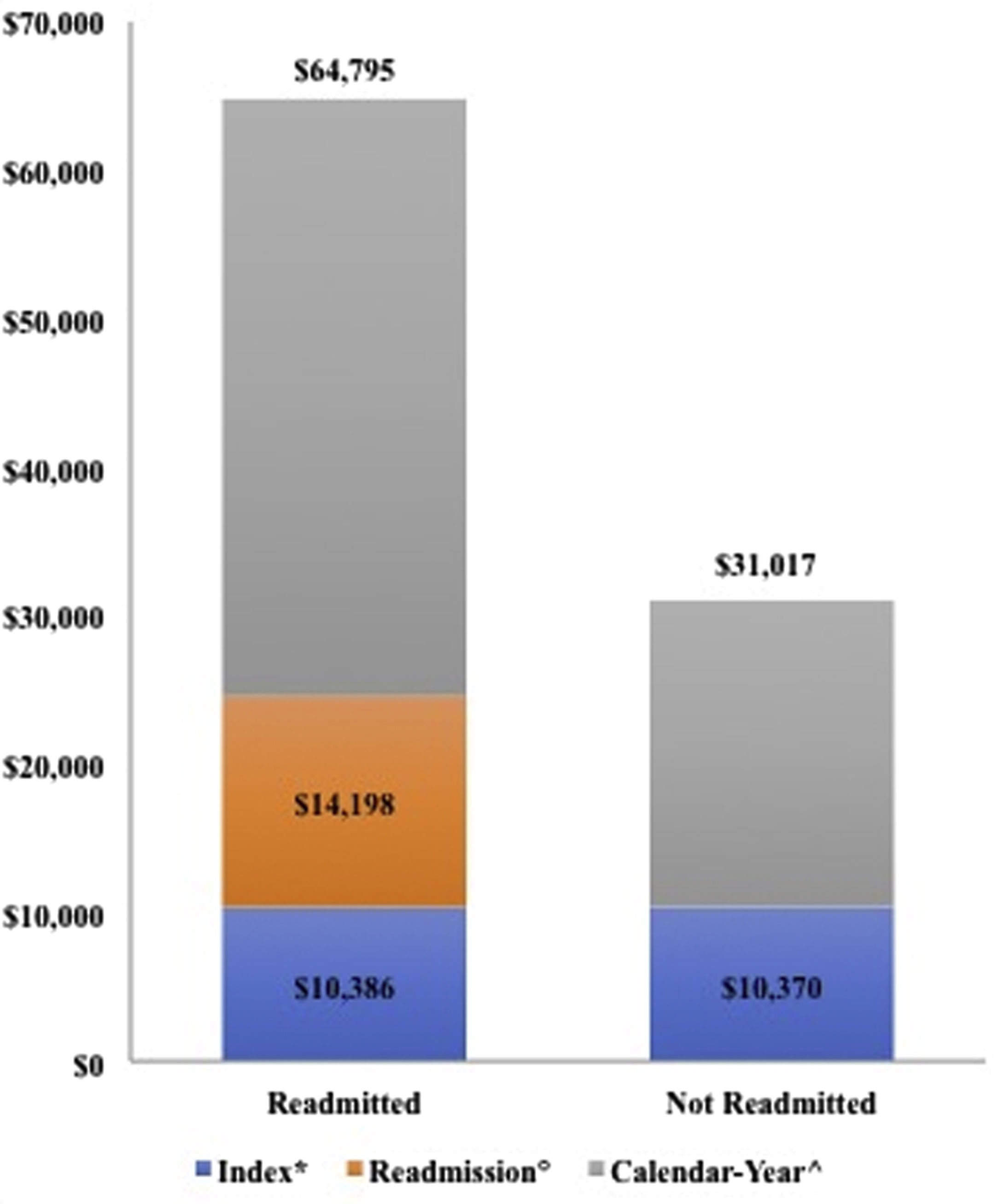
3.3Cost of 30-day readmissionThe cost of index hospitalization was similar between those readmitted and not readmitted ($10,386 vs. $10,370, p-value=0.96). However, among those readmitted within 30 days, the cost of the first readmission was significantly higher than the index admission ($14,198 vs. $10,386, p-value <0.001). When adding the total calendar-year cost of all hospitalizations, 30-day readmission had a significant impact on calendar-year total cost of hospitalizations ($64,795 vs. $31,017, p-value <0.001; Table 1 and Fig. 2).
Cost of hospitalization in cirrhosis patients admitted with hepatic encephalopathy: 2013 Nationwide Readmission Database.
Comparing index admission and total-calendar year costs of hospitalizations in those readmitted versus not readmitted; comparing index admission versus first readmission costs in those readmitted within 30 days.
*: $10,386 vs. $10,370; p-value=0.968.
°: $14,198 vs. $10,386; p-value <0.001.
^: $64,795vs. $31,017; p-value <0.001.
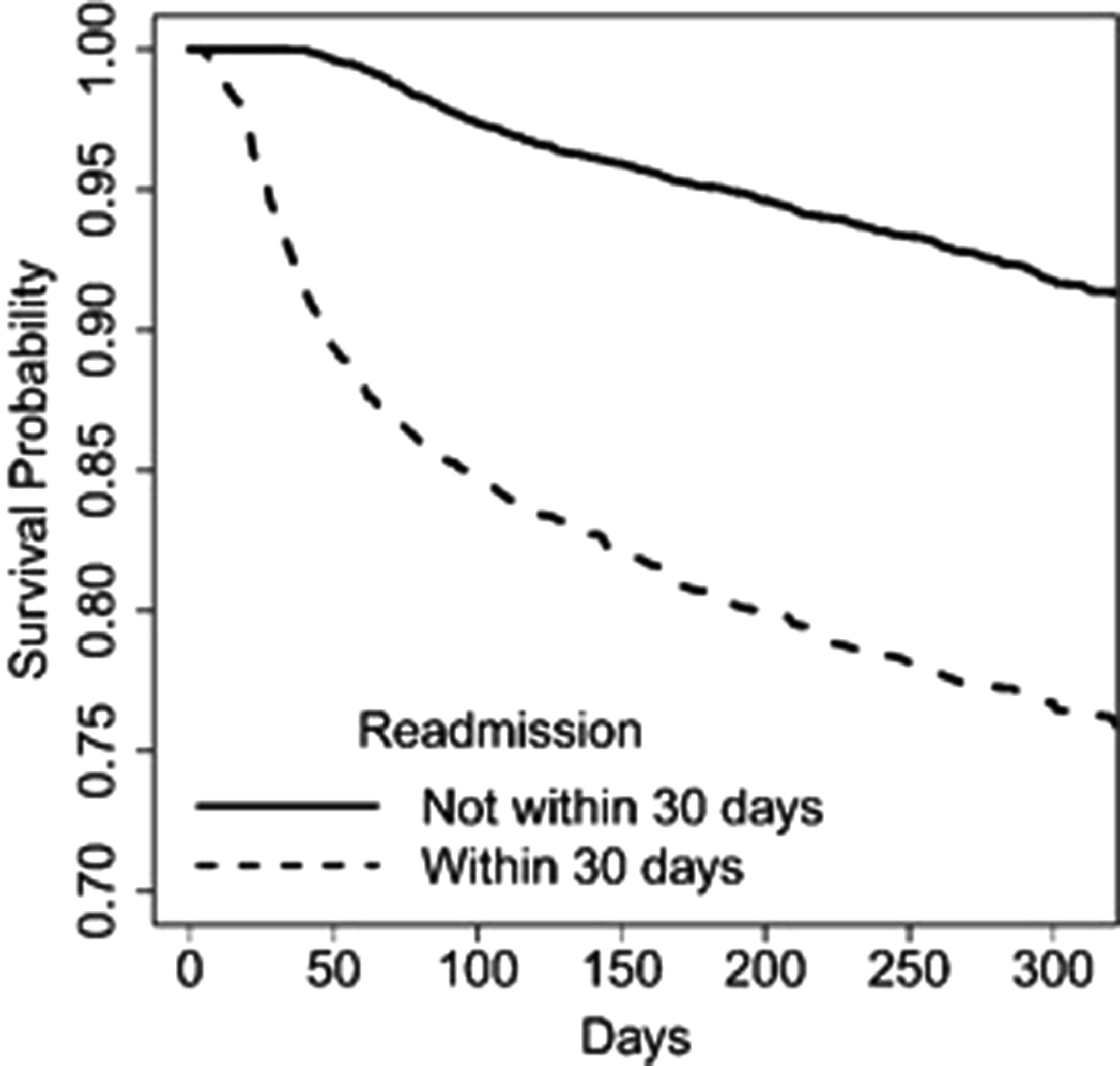
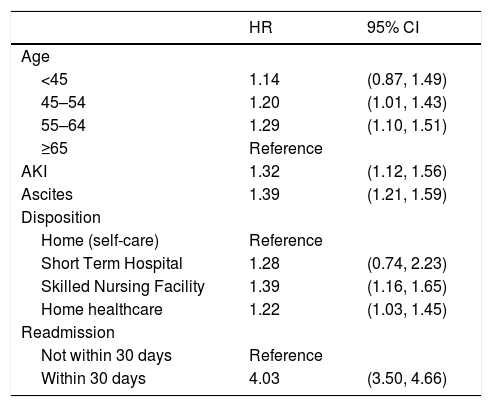
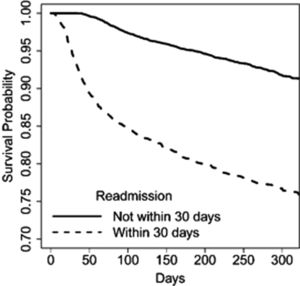
For our overall cohort with HE (n=24,473), 995 (4.1%) patients died during their first calendar-readmission and 2328 (9.5%) died at any point during 2013. Of the patients readmitted within 30 days (n=7931), 636 (8.0%) died on their initial readmission, and 1502 (18.9%) died during the calendar-year (Fig. 1). On multivariable analysis (Table 4 and Supplemental Table 5), age groups 45–54 years (HR: 1.20; 95% CI: 1.01–1.43) and 55–64 years (HR: 1.29; 95% CI: 1.10–1.51), AKI (HR: 1.32; 95% CI: 1.12–1.56), ascites (HR: 1.39; 95% CI: 1.21–1.59), and discharge to a skilled nursing facility (HR: 1.39; 95% CI: 1.16–1.65) or with home healthcare (HR: 1.22; 95% CI: 1.03–1.45) independently predicted calendar-year mortality. Most notably, readmission within 30 days (HR: 4.03; 95% CI: 3.50–4.66) was the strongest predictor of calendar-year mortality (Fig. 3).
Multivariable analysis of predictors for calendar-year mortality in patients with hepatic encephalopathy.
| HR | 95% CI | |
|---|---|---|
| Age | ||
| <45 | 1.14 | (0.87, 1.49) |
| 45–54 | 1.20 | (1.01, 1.43) |
| 55–64 | 1.29 | (1.10, 1.51) |
| ≥65 | Reference | |
| AKI | 1.32 | (1.12, 1.56) |
| Ascites | 1.39 | (1.21, 1.59) |
| Disposition | ||
| Home (self-care) | Reference | |
| Short Term Hospital | 1.28 | (0.74, 2.23) |
| Skilled Nursing Facility | 1.39 | (1.16, 1.65) |
| Home healthcare | 1.22 | (1.03, 1.45) |
| Readmission | ||
| Not within 30 days | Reference | |
| Within 30 days | 4.03 | (3.50, 4.66) |
HR: hazard ratio; CI: confidence interval; AKI: acute kidney injury.
Kaplan–Meier curves showing survival probability in patients with hepatic encephalopathy comparing those readmitted versus not readmitted within 30 days.
Patients readmitted within 30 days of index hospitalization had significantly lower calendar-year survival than those not readmitted within 30 days (HR: 4.03; 95% CI: 3.50–4.66).
Out of the 995 patients who died on their first readmission, five of the top ten most frequent ICD-9-CM codes for readmission (which encompassed 67.6% of all readmissions for this cohort) were due to liver-related etiologies. They included HE (21.3%), alcoholic cirrhosis (5.1%), hepatorenal syndrome (4.0%), non-alcoholic cirrhosis (2.9%), and other sequelae of chronic liver disease (1.8%). Sepsis (24.5%), acute respiratory failure (4.8%), and AKI (3.3%) were the top three causes for readmission for non-cirrhosis related causes of readmission.
4DiscussionIn this study based on a large national readmission database involving cirrhosis patients admitted with HE, we have shown that approximately one-third of patients were readmitted within 30 days and one-third were readmitted with HE. Modifiable factors such as paracentesis, AKI, and ascites increased the risk of 30-day readmission. Based on this administrative database, we proposed a simple and convenient scoring system utilizing variables from index admission to estimate the risk of 30-day readmission in patients with HE. Not only is the healthcare resource utilization higher among patients admitted within 30 days, but early readmission also predicts calendar-year mortality.
Interestingly, indicators of volume status (AKI, ascites, and need for paracentesis) were associated with early readmission. Patients with cirrhosis develop ascites and volume overload due to complex pathophysiology including systemic vasodilation and its multiple downstream effects. As such, these patients require diuresis for volume control [20]. Acute kidney injury occurs often, with a prevalence up to 50% [21]. Hepatic encephalopathy patients are not candidates for TIPS, and patients with renal injury and/or frequent AKIs are not candidates for diuretic therapy [21,22]. Thus, HE patients with refractory ascites and/or recurrent AKI require repeated paracentesis [23]. Measures for optimal management of volume status and consideration of scheduled outpatient paracentesis may reduce readmissions. Multiple prior studies have evaluated strategies to prevent readmissions in cirrhotics, including interventions that have had profound reductions in those with HE [10,24]. For example, a prospective study evaluating 30-day readmissions found a reduction in readmissions with an electronic checklist provided in the electronic medical record [10].
We have identified multiple risk factors associated with early readmission in HE, which allowed for the development of a readmissions risk model. National databases have been used to develop risk scores previously in the field of gastroenterology. The NIS has been utilized to create a scoring system for hospitalization severity in Crohn's disease patients, as well as for a model calculating the risk of colectomy in ulcerative colitis patients [25,26]. Given the high overall early readmission risk in cirrhotics with HE, our scoring system will assist healthcare providers in identifying patients at a higher risk for readmission. For example, a patient with ascites who undergoes paracentesis is characterized as ‘low risk’ for early readmission, assuming no other risk factors. However, the presence of one additional other risk factor (such as AKI, non-alcoholic etiology of cirrhosis, insurance status, or age <65) will immediately place them in the ‘high risk’ category, increasing their overall risk of early readmission by more than 10%. We were able to validate the model through the 2014 NRD, therefore strengthening this risk scoring system. Identifying patients at an increased risk of early readmission may drastically improve outcomes in HE patients.
This is the first study to our knowledge that has proposed a risk model for readmission in patients with HE on such a large magnitude. Therefore, the potential implications of a low- and high-risk scoring system model for 30-day readmission deserves comment. From a clinical standpoint, quantifying the 30-day readmission risk at the time of hospital discharge is valuable, as it would provide an opportunity to follow high-risk patients more closely with a proactive management plan. This risk scoring system is based on readily available variables at the time of index admission and during the hospital stay, which can easily differentiate those with low risk from high risk; this is a much more precise process than assuming that all hospitalized patients have equally high risk. Through our scoring system, the initial goal would be to prevent an early readmission. In turn, mortality rates should improve, as we’ve shown early readmission to be the strongest predictor of calendar-year mortality. Additionally, identifying such patients could lower both immediate and long-term healthcare costs. Our hope is that the use of this risk score will aid in early identification of patients who need more aggressive discharge planning and follow-up. Moreover, we are planning to further validate this scoring system in a prospective way on our inpatient hepatology service, which would allow us to include other variables that are not available through the NRD (MELD-Na, race, medications, etc.). This study should further strengthen the validity of our scoring system, as well as improve its accuracy in clinical practice.
We found that the total calendar-year cost of hospitalizations ($64,795) is markedly higher in those that were initially readmitted within 30 days, and is similar to a previous national database study ($63,108) [2]. The costs of index hospitalizations were nearly identical among cases and controls, whereas the cost of the first readmission in our ‘early readmission’ cohort was significantly higher than their index cost. Early readmission is therefore not only a poor prognostic sign for the patient, but also a significant contributor to the overall healthcare burden in those with HE. Thus, strategies to reduce readmissions will have a significant impact on reducing the cost of HE care [10,24].
As is demonstrated in this national database, hospitalization for HE is associated with high mortality. Both our readmission and calendar-year mortality rates are similar to prior smaller studies [1,2,5,6,8–13]. Admission for HE was associated with a calendar-year mortality of 9.5%, similar to previously reported rates of 7–15% [1,2]. In patients who were readmitted within 30 days, approximately 1-in-12 died on their first readmission, and 1-in-5 died during the calendar year. While we can only report on calendar-year mortality on readmission to a hospital, previous studies have noted a 1-year survival rate of 20–50% and 3-year survival rate of 15–23% [1,3]. Most importantly, we demonstrate predictors for calendar-year mortality. Of these, modifiable variables include early readmission, AKI, ascites, and disposition. Future studies focused on improving these modifiable factors will be vital in reducing mortality in this population. As we demonstrated the most common causes of death on readmission (primarily cirrhosis-related and/or infectious-related), further investigations which we have proposed will allow for a focused examination of exact causes of death and the specific treatments that patients did – or did not – receive.
This study has several inherent limitations as an administrative database that relies on accurate ICD-9-CM coding. The NRD does not provide information based on race, ethnicity, severity of HE, or laboratory parameters. Additionally, Child and Model for End-Stage Liver Disease (MELD) scores are unavailable; therefore, a misclassification error is possible, although it is expected to be non-differential. Moreover, medications and other treatment goals (such as lactulose and bowel movement frequency) are not recorded. With the help of the statistical tests used, an association of variables with readmission has been established but not causality. Information on mortality outside of hospital admissions is also not available and therefore the reported mortality may be under represented in our study. However, an advantage to using the NRD is that individual patients can be studied longitudinally over the course of a calendar year. Despite such limitations, the overall power of using a nationwide database outweighs them. Results of studies based on large database are also generalizable to all patients with HE. Finally, a study evaluating a cohort to this scale would otherwise be unachievable.
In conclusion, approximately one-third of patients with HE are readmitted within 30 days. Early readmission, AKI, and ascites are among modifiable risk factors that predict calendar-year mortality. Hepatic encephalopathy patients with refractory ascites and/or AKI are neither candidates for diuretics nor TIPS, and therefore require repeated paracentesis. A focus on improving modifiable risk factors, including measures to improve access for paracentesis and reducing readmissions, may improve outcomes for this tenuous population. Thirty-day readmission is associated with increased mortality and healthcare utilization. Using a readmission risk score may help to identify those at higher risk, and should be used to assist inpatient teams when caring for HE patients.AbbreviationsHE
hepatic encephalopathy
NISNationwide Inpatient Sample
EGDesophagogastroduodenoscopy
ACAAffordable Care Act
CMSCenters for Medicare and Medicaid
NRDNationwide Readmission Database
AHRQAgency for Healthcare Research and Quality
HCUPHealthcare Cost and Utilization Project
ICD-9-CMInternational Classification of Diseases, Ninth Edition Clinical Modification
TIPStransjugular intrahepatic portosystemic shunts
AKIacute kidney injury
SBPspontaneous bacterial peritonitis
ORodds ratio
HRhazard ratio
CIconfidence interval
MELDModel for End-Stage Liver Disease
FundingNone.
Conflict of interestThe authors declare that they have no conflict of interest.