Malnutrition is a common cause of impeding recovery in patients with acute alcoholic hepatitis (AAH). Previous reports have shown that appropriate nutritional supplementation reduce short and long-term mortality in patients with AAH. Despite these clear recommendations, the element of nutrition in AAH is often neglected. We designed a quality improvement project to evaluate and improve compliance with appropriate nutrition in patients presenting with AAH at our institution. Patients admitted with AAH between December 2015 to December 2016 were included. Our primary outcome was compliance with appropriate nutrition. Secondary outcomes included nutrition consultation and hepatology consultation. A total of fifty-four patients were included. Nine of the 53 patients (17%) received high calorie and high protein diets. Hepatology was consulted in 72% (38/53) of the patients, and 21% (8/38) of these patients received appropriate nutrition as compared to only 8.3% (1/12) in whom hepatology was not consulted. Nutrition was consulted in 55% (29/53) of these patients and 67% (19/28) of those patients received appropriate nutrition. In conclusion, our compliance of appropriate nutrition in AAH is low. Our initial investigation suggests that hepatology and nutrition consultation improved compliance with appropriate nutrition. The next step will be to implement protocolized care for appropriate nutrition in AAH by incorporating consultation of hepatology and nutrition services, assess the effect on adherence to appropriate nutrition, and determine the impact on patient outcomes.
Acute alcoholic hepatitis (AAH) is a form of liver disease that develops in patients with heavy alcohol use, and is manifested by jaundice, malaise, anorexia, and tender hepatomegaly. In recent years, there has been an increase in hospitalizations for AAH, with an average length of stay of approximately 6 days.1
The American Gastroenterological Association (AGA) best practice advisory states, “Patients with AAH who have jaundice should be admitted to the hospital to encourage abstinence [and] restore adequate nutrition”. Malnutrition is a cause of impeding recovery in AAH. Previous studies have shown that appropriate nutritional supplementation reduces short and long-term mortality in patients with AAH.2 Current consensus guidelines by the AGA and American Association for the Studies of Liver Disease (AASLD) recommend a “1–1.5 gram protein and 30–40 kcal/kg body weight” daily intake for adequate recovery. If the patient is unable to eat because of anorexia or altered mental status, enteral feeding should be considered.3 Despite consensus in all guidelines, the element of nutrition in AAH is often neglected. We designed a quality improvement project to assess whether patients presenting to our institution with a diagnosis of AAH receive appropriate nutrition.
This study took place at a tertiary care academic institution. All patients with AAH admitted to our institution from December, 2015 to December, 2016 were included. The diagnosis of AAH was identified with the following criteria:
- •
History of active alcohol use.
- •
Total bilirubin ≥ 3.0 mg/dL.
- •
Elevated aspartate aminotransferase (AST) (50–400 U/ L), and
- •
AST:ALT (alanine aminotransferase) ratio > 1.5.
Patients with AAH who could not tolerate oral diet or were on enteral feeding were excluded from the study. Electronic medical records (EMR) were reviewed and baseline demographic information were collected including age, sex, and presenting complaint. Laboratory values of total bilirubin, prothrombin time/international normalized ratio, AST, ALT, and serum creatinine were also recorded. Data regarding placement of orders for appropriate nutrition and consultation for gastroenterology/hepatology and nutrition services were collected. Outcomes including length of stay, 30-day readmissions, transfer to higher level of care, and mortality rates were also recorded. The institutional review board (IRB) of our institution provided exemption from IRB purview due to the nature of the study.
The primary outcome was provider adherence to ordering a high-protein, high-calorie diet for patients admitted with primary or secondary diagnosis of AAH. We also looked at outcomes including length of stay (LOS), 30-day readmissions, and mortality. Categorical variables were reported as percentages and continuous variables were reported as mean values. Pearson’s χ2 tests were used to compare categorical variables and two-sample t-tests were used for continuous variables. A two-sided p-value of 0.05 was used to determine statistical significance.
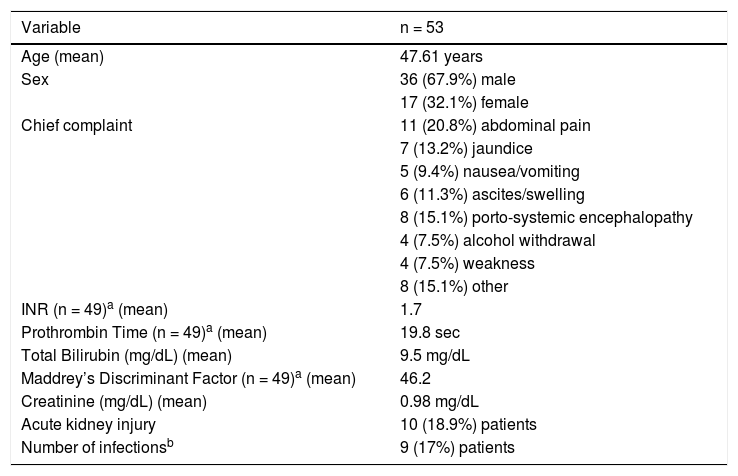
A total of 53 patients were identified with either primary or secondary diagnosis of acute alcoholic hepatitis (Table 1). Average age was 47 years and 68% were males. The majority of patients presented with the chief complaint of abdominal pain, followed by altered mental status and jaundice. Of the 53 patients, laboratory values were available for 49 patients to calculate the Maddrey’s Discriminant Function (MDF) for each patient, resulting an average MDF of 46. Overall, 9 of the 53 patients (17%) had concomitant infection, majority being urinary tract infections. Acute kidney injury was present in 19% of the patients.
Patient demographics and baseline laboratory values.
| Variable | n = 53 |
|---|---|
| Age (mean) | 47.61 years |
| Sex | 36 (67.9%) male |
| 17 (32.1%) female | |
| Chief complaint | 11 (20.8%) abdominal pain |
| 7 (13.2%) jaundice | |
| 5 (9.4%) nausea/vomiting | |
| 6 (11.3%) ascites/swelling | |
| 8 (15.1%) porto-systemic encephalopathy | |
| 4 (7.5%) alcohol withdrawal | |
| 4 (7.5%) weakness | |
| 8 (15.1%) other | |
| INR (n = 49)a (mean) | 1.7 |
| Prothrombin Time (n = 49)a (mean) | 19.8 sec |
| Total Bilirubin (mg/dL) (mean) | 9.5 mg/dL |
| Maddrey’s Discriminant Factor (n = 49)a (mean) | 46.2 |
| Creatinine (mg/dL) (mean) | 0.98 mg/dL |
| Acute kidney injury | 10 (18.9%) patients |
| Number of infectionsb | 9 (17%) patients |
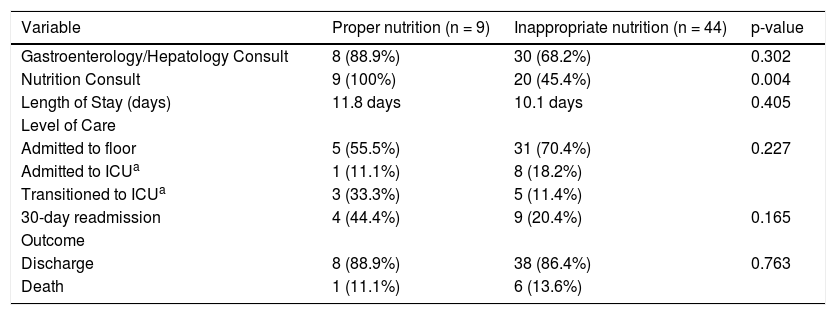
Only 9 patients (17%) had both high-protein and highcalorie diets ordered as part of the treatment plan for AAH. Consultations for Gastroenterology/Hepatology and Nutrition were placed for 72% and 55% of the patients, respectively. Patients who had nutrition consultations were significantly more likely to receive appropriate nutrition (Table 2). There was no difference in LOS, 30-day readmissions and mortality in patients who received appropriate nutrition versus those who did not in our cohort.
Patient outcomes.
| Variable | Proper nutrition (n = 9) | Inappropriate nutrition (n = 44) | p-value |
|---|---|---|---|
| Gastroenterology/Hepatology Consult | 8 (88.9%) | 30 (68.2%) | 0.302 |
| Nutrition Consult | 9 (100%) | 20 (45.4%) | 0.004 |
| Length of Stay (days) | 11.8 days | 10.1 days | 0.405 |
| Level of Care | |||
| Admitted to floor | 5 (55.5%) | 31 (70.4%) | 0.227 |
| Admitted to ICUa | 1 (11.1%) | 8 (18.2%) | |
| Transitioned to ICUa | 3 (33.3%) | 5 (11.4%) | |
| 30-day readmission | 4 (44.4%) | 9 (20.4%) | 0.165 |
| Outcome | |||
| Discharge | 8 (88.9%) | 38 (86.4%) | 0.763 |
| Death | 1 (11.1%) | 6 (13.6%) |
Our analysis showed that adherence to appropriate nutrition in patients presenting with acute alcoholic hepatitis is low. To our knowledge, this is the first report evaluating the adherence of appropriate nutrition in patients with AAH.
Approximately 0.71–0.83% of hospital admissions in the United States are due to AAH, with a significant increase seen over the past decade alone.1 The average length of stay is approximately 6 days with average cost per hospitalization increasing 40% from 2002 to 2010.1 Medicare/Medicaid was the primary payer for a little over 50% of the hospitalizations. These numbers alone convey the impact on our economic system. It is even more important to assess physician adherence to the treatment guidelines, which have been shown to provide clinical benefit.
Acute alcoholic hepatitis can be associated with a high mortality, up to 40–50%, depending on concomitant infection or renal dysfunction.4 Due to a growing population with alcohol abuse, it is critical to recognize barriers to appropriate therapy, particularly nutritional support. Those with alcoholic liver disease have protein-calorie malnutrition due to both lack of nutritional intake and their bodies’ constant systemic inflammatory state.5 The degree of malnutrition can be a prognostic factor of both disease severity and outcomes. Previously, nutritional status in patients diagnosed with AAH was found to correlate with 6-month and 1-year survival.6 Supplemental nutrition has been explored for patients admitted with AAH, especially for those with porto-systemic encephalopathy and unable to adequately eat. Studies on parenteral nutrition in AAH have not shown an impact on mortality but do correlate with decreasing laboratory markers that suggest improvement with nutrition-associated complications, including hepatocellular inflammation.7 Aggressive enteral nutrition, which is the preferred route because it maintains gut integrity and decreases risk of infection, is associated with improvement in both biochemical and nutritional status, as well as disease state, such as encephalopathy.8
Because patients with chronic liver disease have baseline sub-optimal nutritional and immune states, they are highly susceptible to infection for multiple reasons. They are considered immunosuppressed in the setting of uncontrolled activation of both innate and adaptive immunity.5 AAH is considered an increased cytokine storm state, eliciting a systemic inflammatory response syndrome (SIRS). The immune dysfunction in the presence of SIRS puts patients with AAH at higher risk for infection, multiorgan failure, and death.9 When patients are admitted to the hospital with primary or secondary diagnoses of AAH, it is recommended to screen the patient for infection, as this has a major impact on morality.2,3 Increased nutritional supplementation has been posited to provide building blocks to assist in fighting infection and restoring immune homeostasis especially in the critically ill, in addition to increasing total lymphocyte count in patients with AAH.10 Thus, nutrition is not only a direct treatment for AAH, but also it indirectly provides supportive care for common infections in this immunocompromised population.
Although there is significant data on the importance of nutrition in AAH, there is paucity of literature on adherence to appropriate nutrition in routine clinical practice. Our study highlights that despite consensus in all guidelines, adherence to appropriate nutrition is low in AAH.
Our report is subject to certain limitations. It is a small sample size from a single center. Since our study is a quality improvement project, we cannot compare the effect of appropriate nutrition on outcomes such as LOS, 30-day readmissions and mortality. The impact of appropriate nutrition has already been validated in prior studies.8 Despite these limitations, our study highlights an important gap in adherence to guidelines in patients with AAH.
Based on these findings, our next steps include:
- •
Educational campaign for Gastroenterology/Hepatology, Internal Medicine, and Family Medicine physicians.
- •
Direct feedback on guidelines adherence.
- •
Develop a multidisciplinary task force to coordinate with clinical nutrition and dietary services.
- •
Develop Electronic Medical Record pathways (i.e. smart phrases, templates) for proper nutritional orders.
- •
Assess barriers to proper diet administration.
- •
Develop patient education for post-hospitalization.
- •
Monitor and collect post-intervention data to assess improvement in adherence.