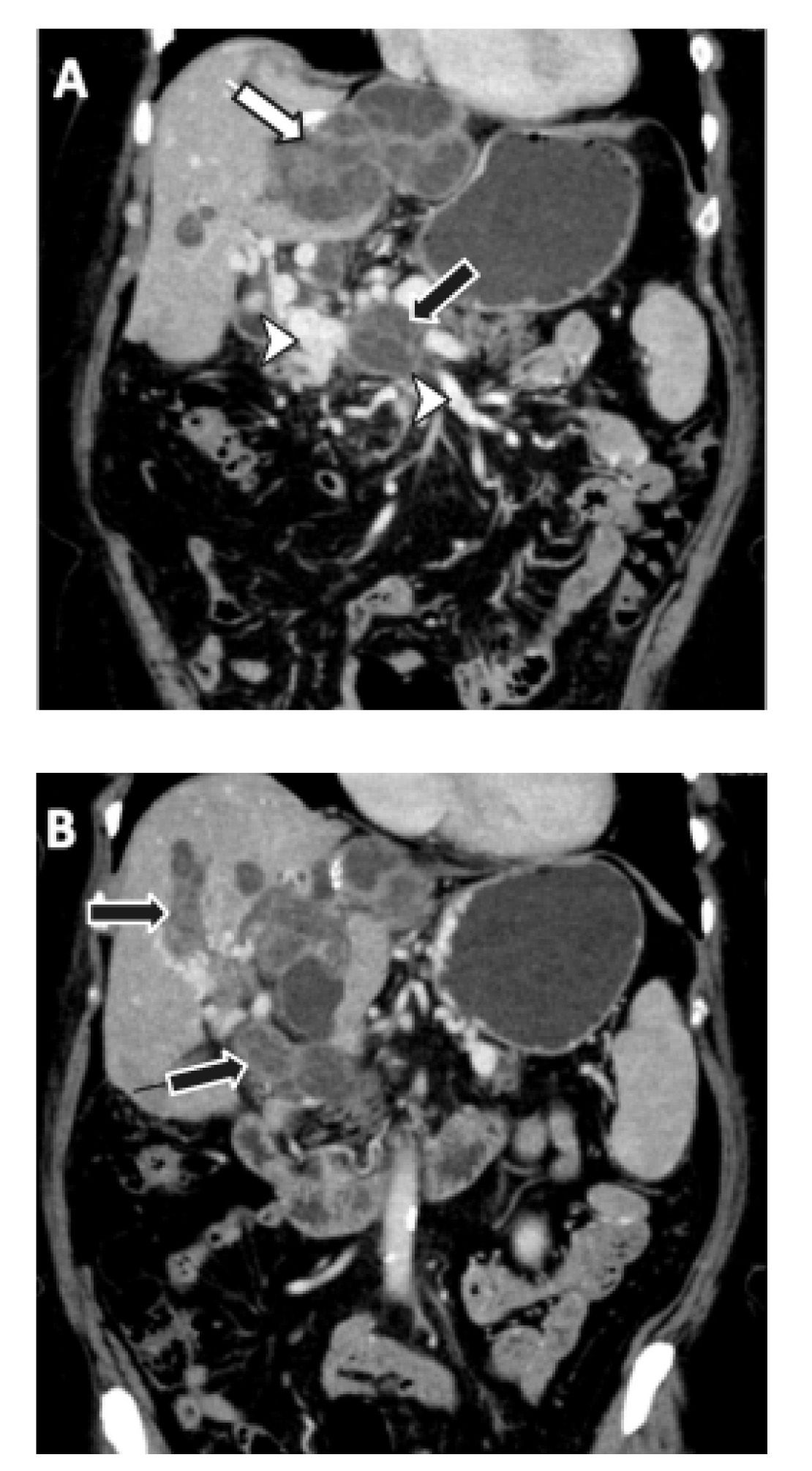
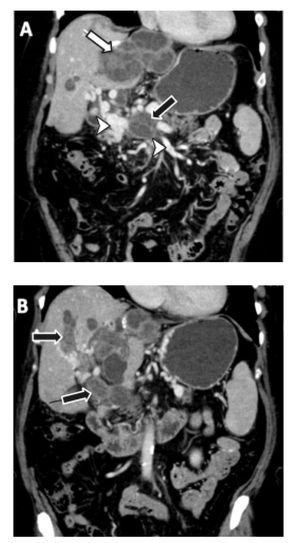
A 62-year-old, rural female patient was referred after one week of nonspecific abdominal pain with spontaneous resolution and without other symptoms. The physical exam revealed a painless hepatomegaly without other abnormalities. Her only medical history was a surgical drainage of a liver abscess of hydatic origin 15 years ago in a rural hospital, without subsequent medical checks. Laboratory values obtained on admission were: white blood count of 6,000/mm3 with 10% lymphocytes, 79% neutrophils and 8% eosinophils, hemoglobin of 11 g/dL, and a platelet count of 198,000/mm3. Hepatic laboratory parameters showed no abnormalities. An imaging study was requested. Abdominal and pelvic CT (Figure 1) showed multiple hepatic masses, the largest being 10 x 5 x 7 cm, in the left liver lobe with intra and extrahepatic portal invasion and secondary cavernomatosis. Upper GI endoscopy showed a grade I esophageal varices.
Given this patient’s antecedents and the characteristics of the acquired images, the potential for a diagnosis of hydatid liver disease with portal invasion was raised. Multiple hydatid cysts and main portal vein occlusion with absence of flow caused by multiple daughter vesicles replacing the lumen were seen in the abdominal and pelvic CT. A serological study (ELISA test) was positive for hydatid disease.
Echinococcus granulosus is a parasite that infects humans, which can act as intermediate hosts.1,2 This disease is endemic in India, Africa and South America.3 The involvement of the portal vein, with portal hypertension and cavernomatosis, is a very rare complication of hydatid disease.1,3 Diagnostic suspicion should be raised if a patient lives in an endemic zone and presents with a mass in the liver.1 An accurate diagnosis is determined by radiological and serological studies.
The best option for the treatment of hydatid cysts is surgical resection with pericystectomy.2 In addition, complementary anti-echinococcal chemotherapy is usually used to prevent recurrence.2 Very few cases of portal invasion with cavernomatosis have been published.1,3 In general, the surgical approach has yielded disappointing results in these patients as well as high mortality.1
In our patient, surgical treatment was not feasible due to the spread of the disease. Neither a peri-cystectomy nor a liver resection would have left her free of disease. Given her good health condition and the fact that she was currently asymptomatic and had normal liver function, a multidisciplinary team proposed that she receive albendazol therapy and variceal bleeding prophylaxis with propranolol. If her liver function deteriorates or if she develops intractable portal hypertension, she could be a candidate for liver transplantation or a mesocaval shunt.
DisclaimerNo sources of funding or conflicts of interest to disclose.