We present the case of a 56-yr-old woman with vague abdominal pain of approximately 5 months duration. An ultrasound study showed moderate dilation of the common bile duct. Magnetic resonance cholangiopancreatography confirmed a cystic dilatation of the right hepatic duct with intra and extra hepatic component. The patient underwent right hepatectomy and complete excision of the cyst. Microscopically, the cyst wall was formed by fibrous tissue with mild acute and chronic inflammatory infiltrate, the inner surface showed a single layer of columnar epithelium and extensive squamous metaplasia without atypia, wich expressed p63 and high molecular weight cytoqueratin (34BE12).
Choledochal cysts (CC) are rare medical conditions and consist of cystic dilatations of the extrahepatic biliary tree, intrahepatic biliary ducts or both, with an incidence in the western population of 1 in 100,000-150,000 live births, although the incidence has been reported to be as high as 1 in 13,500 births in the United States and 1 in 15,000 births in Australia.1 The rate is remarkably higher in Asian populations with a reported incidence of 1 in 1000, and about two thirds of cases occur in Japan. The reason for this Asian preponderance is still unclear. There is also an unexplained female:male preponderance, commonly reported as 4:1 or 3:1.2.
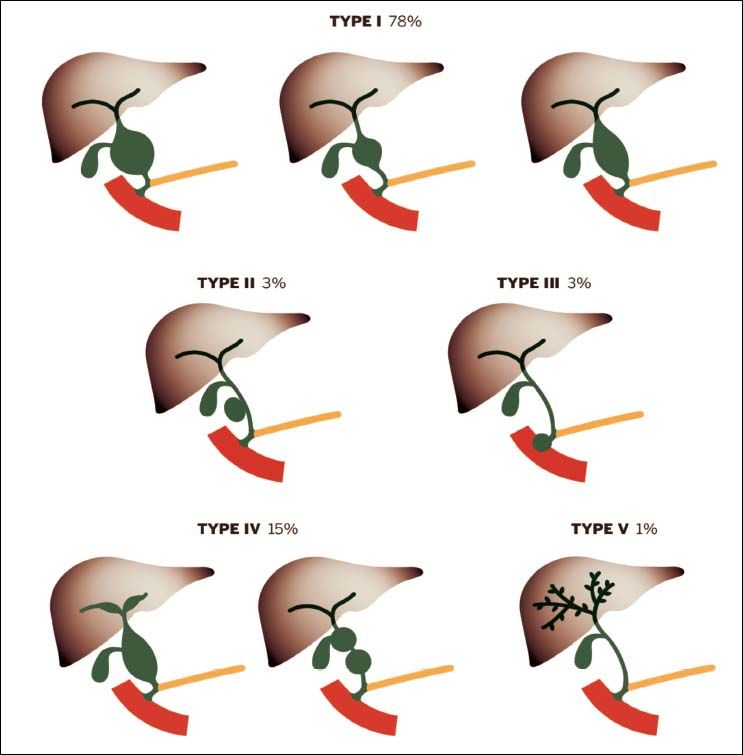
CC are classified into five main types with several subtypes. Anatomical configurations, which do not readily fall into the Todani modification, have been described.3
Case ReportA 56-yr-old woman presented initially complaining of vague abdominal pain of approximately 5 months duration. She denied nausea, vomiting, or weight loss, and had a normal appetite. She had no other medical problems, took no medications regularly, and she had no previous surgical procedures.
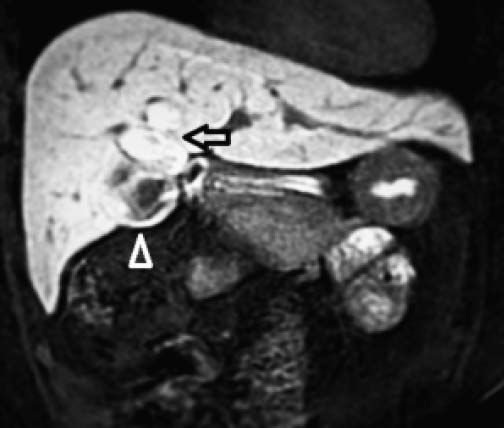
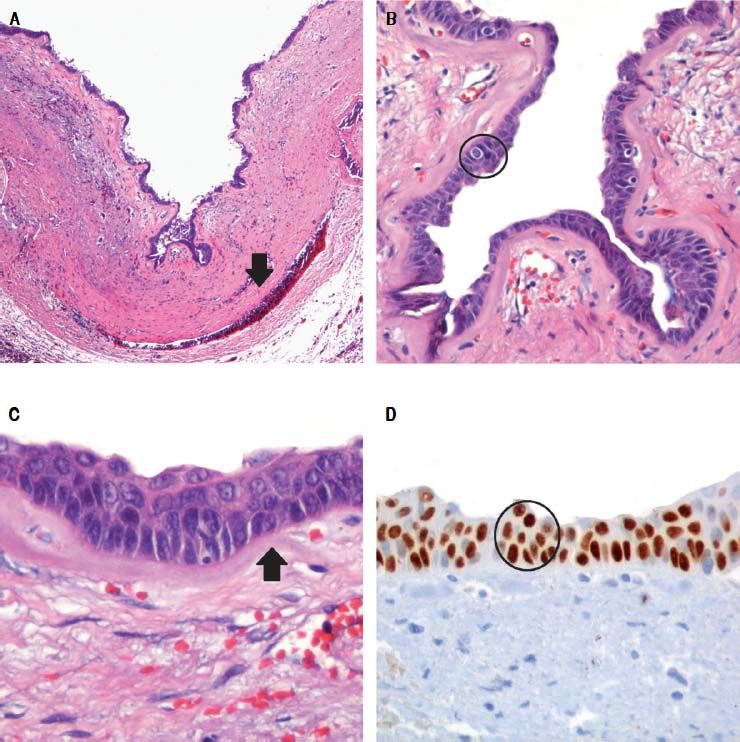
There was no evidence of jaundice or palpable abdominal mass on physical examination. She had mild tenderness at the right upper quadrant but no Murphy’s sign. An ultrasound study showed moderate dilation of the common bile duct and a large cystic mass of unclear origin in the liver, there was no certainty that the cyst continue to the intrahepatic bile tract (Figure 1). A magnetic resonance cholangiopancreatography was obtained to help clarify the anatomy. The magnetic resonance cholangio-pancreatography showed a cystic dilatation of the right hepatic duct with intra and extra hepatic component, the head of the pancreas appeared normal, as did the stomach, kidney, liver, and adrenal gland. There were no other abnormalities (Figures 2 and 3). The patient underwent exploratory laparotomy through a supraumbilical middle line incision. The gallbladder was removed and a sacular dilatation of the right hepatic duct was observed after the removal of the gallblader. The right bile duct was transected distally, at the level of the confluence. Small duct stones were found inside the right hepatic duct. The left and common bile ducts remained intact. A right hepatectomy was performed (Figure 4). There were no intraoperative complications. The specimen consisted of an 18.2 cm liver and biliary duct segment; a 5.6 cm unilocular cyst was identified on the right hepatic duct, the external surface was regular and green, in the inner surface solid areas were not identified. Microscopically, the cyst wall was formed by fibrous tissue with mild acute and chronic inflammatory infiltrate, the inner surface showed a single layer of columnar epithelium and extensive squamous metaplasia without atypia, which expressed p63 and high molecular weight cytoqueratin (34BE12). The residual inner parenchymal was normal (Figure 5). The patient experienced a full recovery and was discharged on postoperative day 5.
CC are rare congenital cystic dilation of the biliary tract, first described by Vater and Ezler in 1723.4 They present primarily in female infants and young children and are more prevalent in East Asian populations. Although benign, CC can be associated with serious complications including malignant transformation, cholangitis, pancreatitis, and cholelithiasis.5
Approximately 80% of the CC are diagnosed in infants and young children within the first decade of life. The incidence of CC ranges from 1 in 100,000 to 1 in 150,000 individuals in Western countries and 1 in 13,000 individuals in Japan.6 CC are 4 times more common in females.1,6 Although the exact etiology is unknown, anomalous pancreaticobiliary duct union (APBDU) is seen in 30% to 70% of all CC where the common bile duct (CBD) and pancreatic duct junction occurs outside the duodenum, allowing reflux of pancreatic fluid into the biliary tree.7
It is well accepted that a CC is a premalignant state. The overall risk of cancer has been reported to be 10%-15%, and increases with age. The risk rises from 2.3% in patients aged 20-30 years to 75% in patients aged 70-80 years, and histopathology shows increasing dysplasia with increasing age. Distribution of the types of cancer found in patients with CC are as follows: adenocarcinoma 73%-84%, anaplastic carcinoma 10%, undifferentiated carcinoma 5%-7%, squamous cell carcinoma 5% and other carcinoma 1.5%.8
Bile duct cysts are classified based on location, extent and shape of the cystic anomaly within the bile duct system. Currently, Todani’s modification3 of the Alonso-Lej classification9 is most commonly used which includes both extrahepatic and intrahepatic bile duct cysts and the variants of Caroli’s disease (Figure 6). This classification includes five types: type I, a solitary fusiform or saccular dilation of the common hepatic and common bile duct; type II, a supraduodenal diverticulum of the common hepatic or common bile duct; type III (also known as choledochocele), an intraduodenal diverticulum of the distal common bile duct; type IV, intrahepatic and extra-hepatic fusiform cysts (IVA), or multiple extrahepatic cysts (IVB); type V (also known as Caroli’s disease), multiple intrahepatic cysts. The classification of bile duct cysts is important as it guides the clinical management and may provide prognostic information.10
In a recent review of the literature, the relative frequency of bile duct cysts using the Todani classification is type I (78%), type II (3%), type III (3%), type IV (15%), and type V (1%). Intrahepatic variants of bile duct cysts with isolated saccular or fusiform cysts arising from the main lobar bile ducts near the confluence have been noted anecdotally and are not classifiable by current typing schemes. Whether these cysts are true bile duct cysts or cystadenoma variants is unknown.11
CC in our patient was classified as Todani type IV, but the morphology of the cysts was unusual. The cyst only took part of the right hepatic duct and its location was totally intrahepatic. Because of this, it is not in any classification and malignant potential was unknown so a wider resection was considered. This variant of CC has not been recognized previously and we propose the classification of this variant under Todani’s system, as type IVC. Surgeons should be aware of the possibility of variant anatomy in choledochal cysts, which is outside the normal classification for this condition.
Clinical presentation varies with age, and 80% of the patients present before the age of 10 years. Children usually have signs and symptoms, but adults are asymptomatic. 82% of children present with two or more symptoms, whereas symptoms are found in only 23% of adults. The most common findings in the infant group are jaundice, hepatomegaly, and an abdominal mass, but abdominal pain is not usually evident. Jaundice is found in 64% of infant patients, and an abdominal mass is found in 82% of infants, but few of the patients present with pancreatitis and cholangitis. The classic triad is abdominal pain, jaundice, and an abdominal mass but is present in a minority of infant patients (0%-17%). In adults, the most common findings are abdominal pain, fever, jaundice and vomiting. Abdominal pain is the most common symptom in adult patients, with an incidence ranging from 78% to 90%. Jaundice, nausea, and cholangitis are found in 40%-50% of adults. Cholangitis or pancreatitis is a common symptom in adult. Dilatation of the bile ducts and stricture cause bile stasis, stone or sludge formation, resulting in ascending cholangitis or pancreatitis.12
With the increased use of axial imaging, more CC are being diagnosed as incidental findings. CC diagnosis is typically accomplished using multimodality imaging including ultrasound, CT, and MRI, including MRCP. Ultrasound is the most frequently used imaging modality given its low cost and accessibility, and has been shown to be reliable and cost effective as single modality imaging. A CBD measuring greater than 10 mm in an adult should alert the physician to the possibilities of cystic dilatation of the biliary tree or obstructive biliary lithiasis. Importantly, intrahepatic biliary dilatation is an indication for further imaging in order to differentiate type I cysts from type IVA disease.13 Additionally, a right upper quadrant cyst separate from the gallbladder is suggestive of CC disease. Choledochal cyst diagnosis is further supported by the presence of a direct communication between the biliary tree and the cystic duct. Endoscopic ultrasound has been shown to be safe and accurate, particularly in its ability to detect a long common channel and choledochoceles although ERCP remains the gold standard for these diagnoses.14
Cholangiography, specifically ERCP and percutaneous transhepatic cholangiography, is the most sensitive technique to define the anatomy of the biliary system. An ERCP allows for direct visualization of the pancreaticobiliary junction. In addition to its diagnostic yield, ERCP can be therapeutic by allowing biliary drainage and endoscopic sphincterotomy of choledochoceles. Percutaneous transhepatic cholangiography also permits sensitive evaluation of the intrahepatic bile ducts, but sometimes can fail to adequately delineate the distal and intraduodenal portions of the CBD. Notably, both procedures are associated with potential complications, including bleeding, cholangitis, acute pancreatitis, and perforation. As a result, noninvasive imaging with MRCP has gained popularity and is replacing direct cholangiography’s diagnostic role in CC.15
Magnetic resonance cholangiopancreatography is a noninvasive procedure and does not require irradiation or oral or intravenous contrast. The MRCP is highly sensitive (70% to 100%) and specific (90% to 100%) in CC diagnosis and classification. Computed tomography is also commonly used and can help demonstrate important anatomic relationships for surgical planning. Although both ultrasound and CT have a sensitivity and specificity of more than 90% in the diagnosis of CC, MRI leads to improved delineation of the exact pathologic anatomy and therefore is generally the imaging technique of choice.16
The pathological characteristics of pediatric CC includes fibrous cystic wall lined by columnar epithelium and lymphocytic infiltration; adult CC include evidence of inflammation and epithelium hyperplasia.17 Most CC show some degree of pathologic changes in the liver including portal fibrosis, central venous distention, parenchymal inflammation, and bile duct proliferation. Except for portal fibrosis and central venous distention, these resolve after appropriate surgical management. Other common findings across all classes of CC include acute and chronic mucosal inflammation, mucosal dysplasia, and a few to no mucus-producing glands.18
Surgical treatment has changed over the years. Previously, the surgical procedure involved a cystoenterostomy. However, in view of postoperative complications, such as cholangitis, pancreatitis and hepatolithiasis (re-operation rate of 70%) and the risk of malignant degeneration of the cyst this procedure is no longer used. At present, the standard treatment involves excision of the cyst and biodigestive derivation. There is some controversy regarding treatment of Type IV and Type V cysts. The excision of an extra-hepatic cyst is the rule, but there are doubts as to whether intra-hepatic cysts should be removed or not. The tendency is to carry out a hepatectomy if the cysts are localized. If they are dispersed, this procedure is not possible.19
The surgical treatment of bile duct cysts focuses on two main objectives: treat cyst-related complications and prevent or treat cyst-associated malignancy. Prior to definitive operative intervention for bile duct cysts, three essential tasks must be completed: the cyst must be defined with cholangiography, the biliary and ampullary anatomy have to be delineated, and biliary infection controlled. Complete cyst excision is recommended for all bile duct cysts with the possible exception of type III bile duct cysts, which may be treated by endoscopic marsupialization with sphincterotomy. Potential advantages of complete excision over partial excision or cyst-enteric drainage include reduced incidence of cyst-related complications (stones, strictures, cholangitis) and intracystic malignancy. If complete excision is not feasible due to local factors, partial cyst excision with Roux-en-Y cystojejunostomy is preferred. Outcomes of complete cyst excision with Roux-en-Y hepaticojejunostomy are excellent; the majority of patients remaining asymptomatic long-term.20
Type I cysts are treated with complete cyst excision and Roux-en-Y hepaticojejunostomy. Cyst excision in adults is frequently more complicated than in children due to prior cyst procedures and inflammation related to recurrent cholangitis and pancreatitis. Type II bile duct cysts, or extrahepatic duct diverticuli, are treated with complete cyst excision. Frequently the cyst neck can be ligated and the cyst excised without the need to reconstruct the common hepatic or common bile duct as required for wide mouth diverticuli. Type III cysts (choledochoceles) historically were treated with transduodenal excision and sphincteroplasty with good results. An observed low risk of malignancy and excellent results with sphincterotomy alone prompted acceptance of endoscopic sphincterotomy as the preferred treatment. Moreover, surveillance for subsequent malignancy can be maintained endoscopically.21
Type IV cysts are subclassified into intrahepatic and extrahepatic cysts (IVA) and multiple extrahepatic cysts (IVB). For both types, resection of the extrahepatic cystic components with Roux-en-Y hepaticojejunostomy is preferred. The technique of excision is similar to that for type I cysts. For type IVB cysts, the choldochocele component is treated with transduodenal sphincteroplasty.
Treatment of the extrahepatic cyst(s) alone is sufficient when intrahepatic cysts are not complicated by ductal strictures, hepatolithiasis, hepatic abscess, or suspicion of malignancy.22
Diffuse forms of type V cysts remain a therapeutic problem. In patients with these cysts, combined procedures with partial hepatectomy and biliodigestive anastomoses have been described, but transplantation offers the only curative option. The progression of congenital hepatic fibrosis in CS and the development of secondary biliary cirrhosis in patients with CD may also lead to portal hypertension that is not treatable by conservative procedures. De Kerckhove, et al. reported congenital hepatic fibrosis in 27% of their patients and the primary indication for orthotopic liver transplantation was recurrent cholangitis (90%).23
An important argument for liver transplantation is the avoidance of cholangiocarcinoma development. Concerns include the choice of an appropriate time point for transplantation, procedural risks, and the use of immunosuppression in young and otherwise healthy individuals. Potential postoperative complications include rejection and vascular thrombosis. Pre-transplant workup of these patients for occult cholangiocarcinoma is crucial.24
Minimally invasive resection of CC has gained popularity. Laparoscopic CC resection with RYHJ reconstruction has been shown to be safe with comparable outcomes to open resection in retrospective analyses. Reported advantages of the laparoscopic approach include improved intraoperative visualization of deeper structures, decreased postoperative pain, shorter hospital stay, improved cosmetic result, and decreased postoperative ileus. However, these cases remain reserved for highly specialized surgeons with a deep understanding of hepatobiliary anatomy and minimally invasive techniques.25 Finally, limited case series of robotic CC resection and reconstruction have been reported with acceptable outcomes, although more studies are needed before widespread acceptance and implementation of this technique.26
Postoperative morbidity and mortality are typically very low in children, while postoperative complications are more commonly seen in adult patients. Late complications (greater than 30 days postoperatively) occur in up to 40% of adult patients and include anastomotic stricture, cancer, cholangitis, and cirrhosis. Type IVA cysts are most commonly associated with complications after management including intrahepatic stones and anastomotic stricture. Overall, CC resection has an excellent prognosis, with an 89% event-free rate and 5-year overall survival rates well over 90%.However, the risk of biliary malignancy remains elevated even more than 15 years after CC excision, and CC-associated biliary malignancy is associated with extremely unfavorable outcomes, with a reported median survival of 6 to 21 months.27
ConclusionsIn conclusion, choledochal cysts in adults are rare and usually present with complications of longstanding cysts. Diagnosis is made by ultrasound, CT contrast cholangiography and MRCP. Total cyst excision is performed to minimize malignant transformation and prevent complications of pancreatitis and recurrent cholangitis. In this report we presented an atypical cyst localize in the right hepatic duct just above the confluence. Microscopically, the cyst wall was formed by fibrous tissue with mild acute and chronic inflammatory infiltrate, the inner surface showed a single layer of columnar epithelium and extensive squamous metaplasia without atypia, which expressed p63 and high molecular weight cytoqueratin (34BE12). The residual inner parenchymal was normal. In conclusion, we describe a new variant of choledochal cyst that has not been recognized previously and we propose the classification of this variant under Todani’s system, as type IVC.