Background. Early hepatic artery thrombosis (HAT) is a potentially lethal complication after orthotopic liver transplantation (OLT) requiring immediate intervention.
Aim. To report an infrequent cause of HAT after OLT and by itself a controversial clinical entity, the median arcuate ligament celiac artery compression.
Case report. A 59-year-old female with hepatitis C virus-induced cirrhosis, Child B, MELD 15, underwent cadaveric-donor OLT with complete vena cava exclusion. Type 1 hepatic artery anatomy was found both in the donor and the recipient, the gastroduodenal artery was ligated. During the first eight postoperative days, clinical and analytical evolution was satisfactory and Doppler ultrasound showed no abnormalities. On the ninth postoperative day, the patient developed hypovolemic shock due to bleeding at the hepatic artery anastomosis, surgical reconstruction was performed. Postoperative color Doppler showed absent hepatic artery flow and an angiography suggested celiac artery compression. The patient was explored again the same day, liberating the celiac artery from the median arcuate ligament and performing thrombectomy and reconstruction of the hepatic artery anastomosis. The patient made a satisfactory recovery and color Doppler showed adequate flow in the hepatic artery. She is alive, free of biliary complications and enjoying a good quality of life 12 months after transplantation.
Conclusion. Median arcuate ligament celiac artery compression is an infrequent anatomical variant that should be intentionally evaluated in the recipient at the time of arterial reconstruction in OLT and specifically be considered in early HAT to allow recognition and effective correction.
Hepatic artery thrombosis is a potentially fatal complication after orthotopic liver transplantation (OLT), representing its more common vascular complication, with an incidence of 5% at high-volume centers.1 Hepatic artery thrombosis is a graft and life-threatening complication in the early postoperative course (≤ 30 days) presenting as rapid deterioration of hepatic function tests, ischemic biliary necrosis, primary dysfunction and/or graft loss.2 Hepatic thrombosis can present in the late course (> 30 days) as abnormal liver function tests in an otherwise asymptomatic patient, or as biliary complications including biliary stenosis or necrosis, bile leak, cholangitis and hepatic abscesses.3 Urgent retransplantation is considered mainstay therapy for survival after early-onset hepatic artery thrombosis, as only 10% graft salvage with anastomotic revision or thrombolysis has been observed in large series;1 making avoidance of these complications a critical issue, especially with current scarcity of donor livers in our country and worldwide.
The aim of this report is to describe a rare cause of hepatic artery thrombosis after OLT and by itself a controversial clinical entity, the median arcuate ligament celiac artery compression. Intermittent obstruction of the hepatic artery during expiration caused by the median arcuate ligament may result in hepatic artery thrombosis or as an ischemic damage to the bile ducts leading to strictures, cholangitis, and eventual loss of the liver graft. Jurim, et al.,4 reported that 10% of their patients undergoing OLT exhibited celiac artery compression syndrome, however, only five cases of hepatic artery thrombosis have been reported in the literature, although only the case of Jiang, et al., has been fully described.5-7
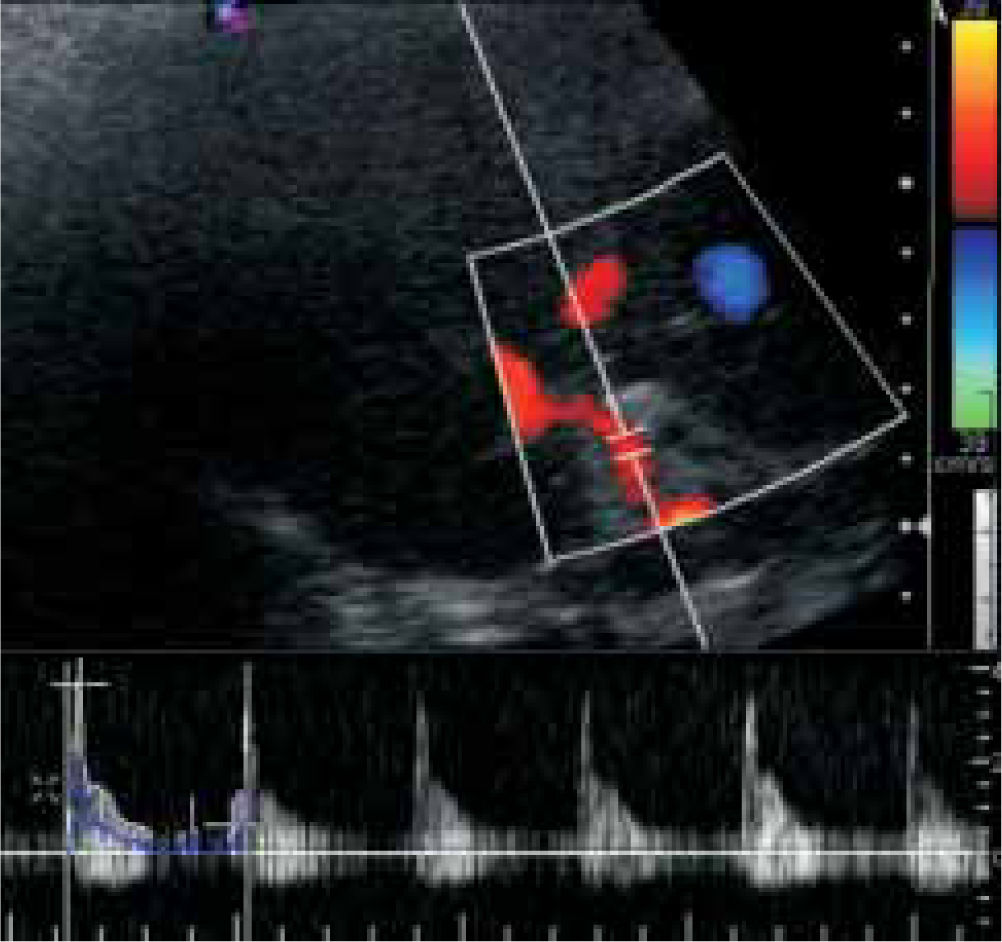
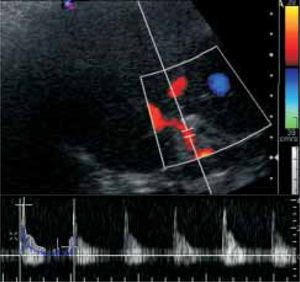
Case ReportA 59-years old female with chronic hepatitis C virus infection genotype 1b and liver cirrhosis Child-Pugh B (8 points) and MELD score 15 with a history of ascites and variceal bleeding in 2002 and 2003 began liver transplantation evaluation in 2006. The patient had a history of hypersplenism, iron-deficiency anemia, varicella-zoster infection and positive serology for cytomegalovirus (IgG). For laboratory data, see table 1. She underwent cadaveric donor orthotopic liver transplantation with total inferior vena cava exclusion in September, 2008. The hepatic artery of the donor had a Carrel's patch and receptor's hepatic artery was divided at the point of origin of the gastroduodenal artery, the arterial anastomosis was performed using continuous 7-0 nonabsorbable polypropylene suture at the bifurcation of the common hepatic artery and the gastroduodenal artery. The donor was a previously healthy 18-years-old male with brain death due to head trauma, the graft had a cold ischemia time of 12 hrs and the preoperative biopsy revealed mild steatosis. A total of 2 liters of transoperative bleeding was quantified and a total of four red blood cell packs were transfused. During the first eight postoperative days, clinical and analytical evolution was satisfactory and color Doppler ultrasound showed a hepatic artery with flow velocity of 36 cm/sec and a resistance index of 0.84 (Figure 1).
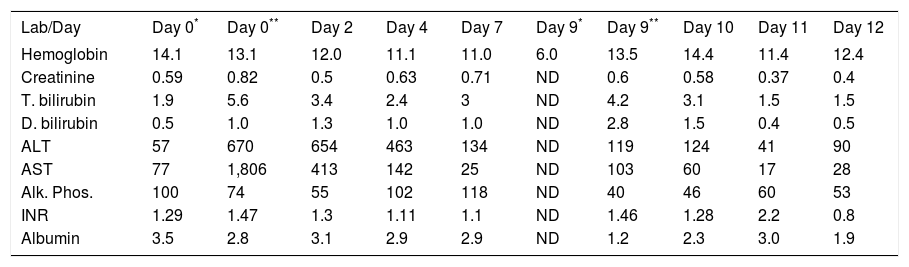
Laboratory data. Day 0 indicates OLT day prior to surgery. The second and third operations took place during Day 9.
| Lab/Day | Day 0* | Day 0** | Day 2 | Day 4 | Day 7 | Day 9* | Day 9** | Day 10 | Day 11 | Day 12 |
|---|---|---|---|---|---|---|---|---|---|---|
| Hemoglobin | 14.1 | 13.1 | 12.0 | 11.1 | 11.0 | 6.0 | 13.5 | 14.4 | 11.4 | 12.4 |
| Creatinine | 0.59 | 0.82 | 0.5 | 0.63 | 0.71 | ND | 0.6 | 0.58 | 0.37 | 0.4 |
| T. bilirubin | 1.9 | 5.6 | 3.4 | 2.4 | 3 | ND | 4.2 | 3.1 | 1.5 | 1.5 |
| D. bilirubin | 0.5 | 1.0 | 1.3 | 1.0 | 1.0 | ND | 2.8 | 1.5 | 0.4 | 0.5 |
| ALT | 57 | 670 | 654 | 463 | 134 | ND | 119 | 124 | 41 | 90 |
| AST | 77 | 1,806 | 413 | 142 | 25 | ND | 103 | 60 | 17 | 28 |
| Alk. Phos. | 100 | 74 | 55 | 102 | 118 | ND | 40 | 46 | 60 | 53 |
| INR | 1.29 | 1.47 | 1.3 | 1.11 | 1.1 | ND | 1.46 | 1.28 | 2.2 | 0.8 |
| Albumin | 3.5 | 2.8 | 3.1 | 2.9 | 2.9 | ND | 1.2 | 2.3 | 3.0 | 1.9 |
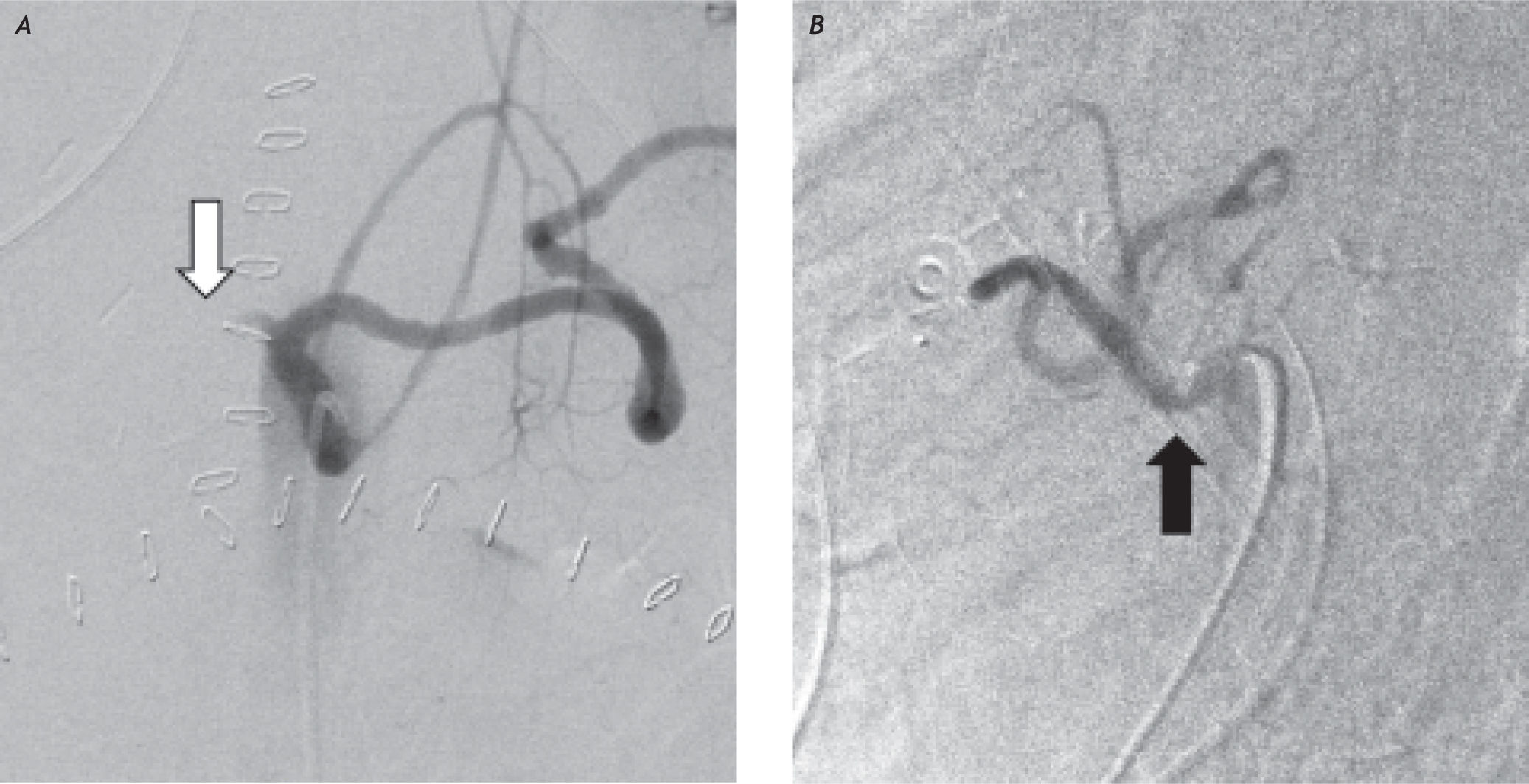
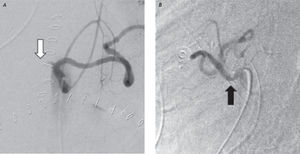
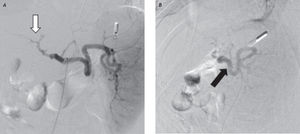
On the early morning of the ninth postoperative day, while preparing her discharge, the patient developed hypovolemic shock. Exploratory laparotomy was immediately done; no pulse was palpated on the hepatic artery and a partial dehiscence was detected at the arterial anastomosis. Small thrombus were detected and removed distal to the anastomosis, surgical reconstruction was performed using continuous 7-0 nonabsorbable polypropylene suture. Intraoperative color Doppler ultrasound showed a patent intrahepatic HA. A total of four red blood cell packs were transfused. At the ICU, hemodynamic instability persisted and postoperative color Doppler ultrasound showed no flow in the hepatic artery. Digital subtraction angiography was performed, showing a characteristic indentation at the origin of the celiac trunk, due to compression by the median arcuate ligament; only the splenic artery was opacified by contrast injection (Figure 2). The patient was re-explored later the same day, finding hepatic artery thrombosis. This was corrected with thrombectomy and arterial anastomosis reconstruction.
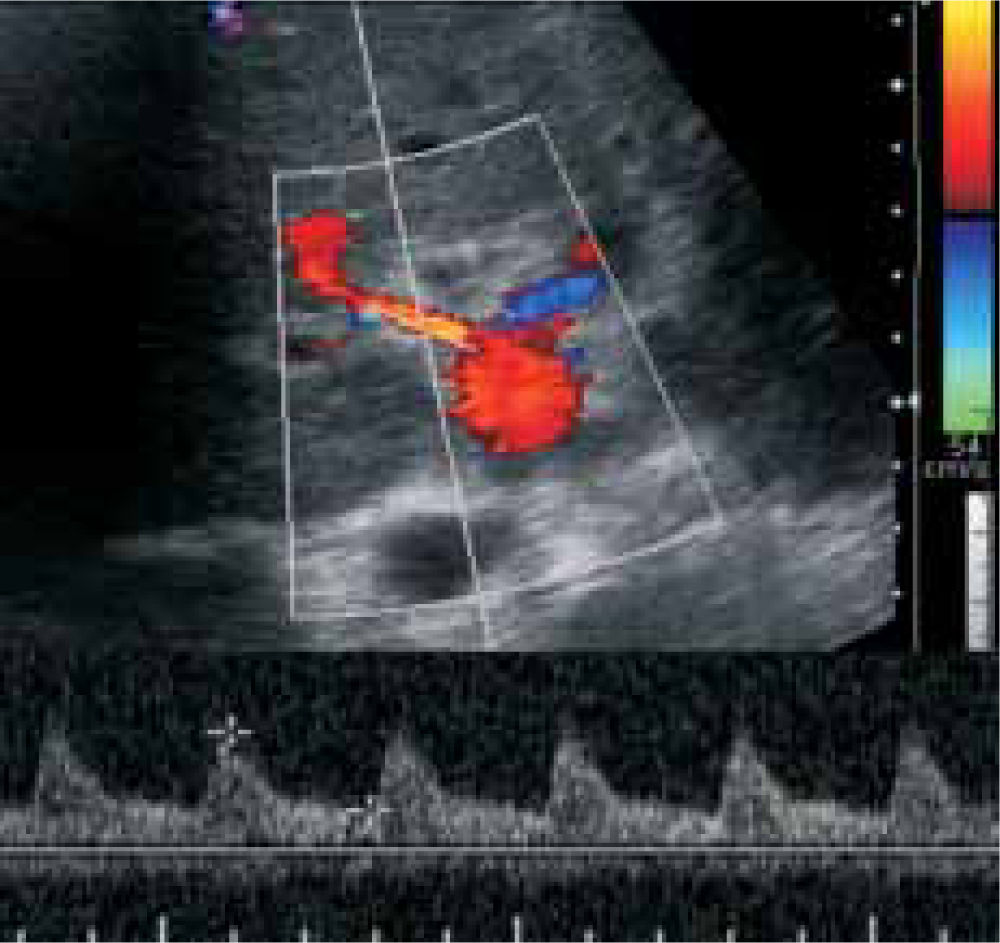
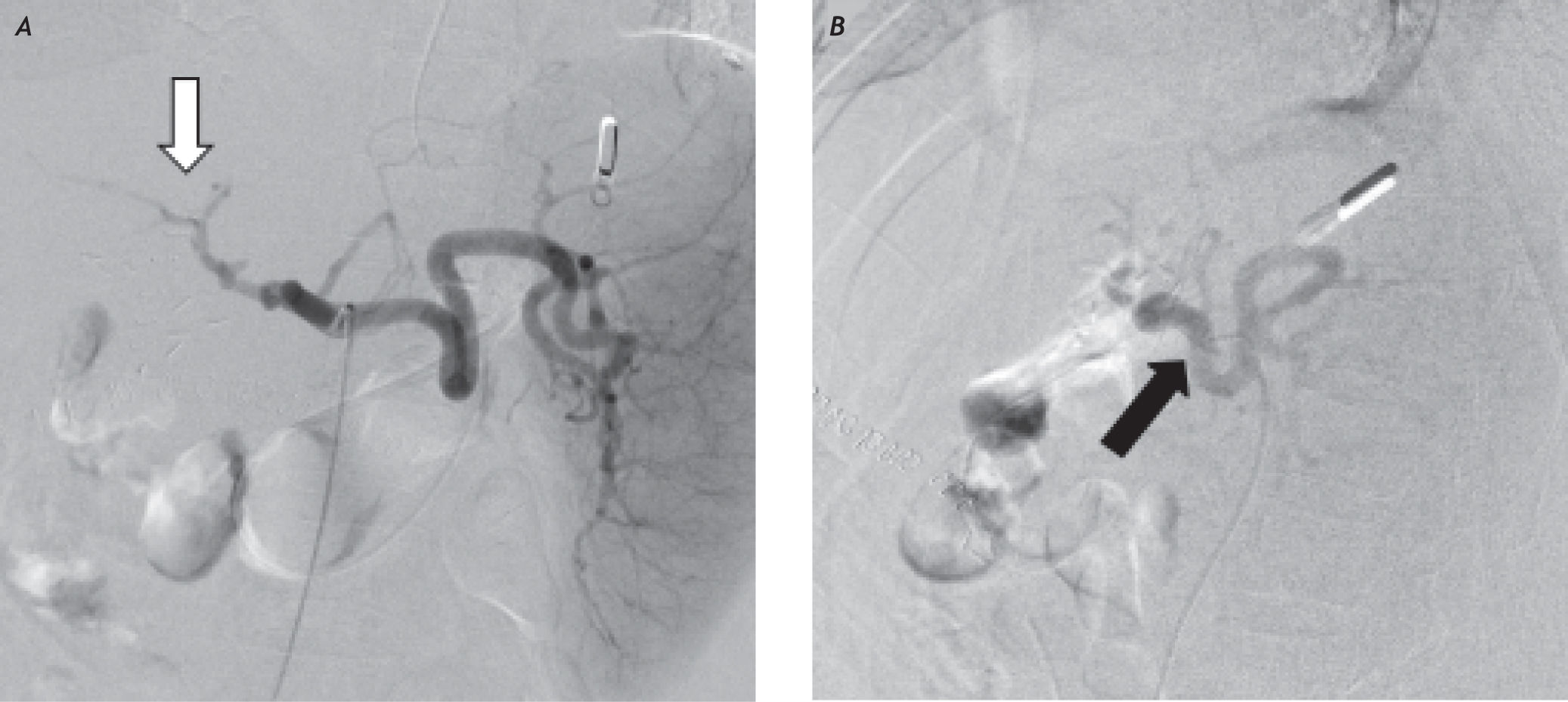
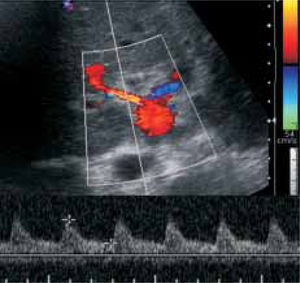
The celiac artery was liberated from the median arcuate ligament by dividing its fibers. Immediately, an adequate pulse was palpated in the hepatic artery. The patient made a satisfactory recovery and color Doppler ultrasound showed adequate flow in the hepatic artery (Figure 3). Three days later, angiography showed normal flow through the hepatic artery (Figure 4) and the patient was discharged ten days after the last intervention. Fortunately, no biliary complication overcame and she is alive and well 12 months after transplantation, with normal hepatic artery flow by color Doppler ultrasound.
The median arcuate ligament is a fibrous arch that passes superior to the origin of the celiac axis, at the level of the first lumbar vertebral body, uniting the two diaphragmatic crura over the aorta, outlining the anterior margin of the aortic hiatus.8 In about 3.710% of the population undergoing OLT,4,9 median arcuate ligament produces compression of the celiac artery causing a characteristic indentation, particularly during end expiration, due to the movement of the retroperitoneal contents (including the aorta and its branches) in a cephalic direction with respect to the diaphragmatic ligament which is relatively fixed.9,10
A small subset of patients suffer a hemodynamically significant compression that cause symptoms, a condition first reported by Harjola in 196311 and Dunbar, et al., in 1965,12 with radiological confirmation by Colapinto, et al., in 1972.13 The original group of patients described at Columbus experienced intermittent epigastric pain, usually in the postprandial period associated with nausea, vomiting, diarrhea (occasionally malabsorptive) and weight loss.12 An abdominal bruit was found in the epigastrium in some patients. The patients improved after surgical division of the median arcuate ligament and the adjacent cords of the celiac plexus, although it was not entirely clear whether this was due to release of compression of the artery or disruption of the neural pathways. More recently, it has been pointed out that not all patient's symptoms resolves after the operation.14 Some authors have even questioned the mere relationship of clinical symptoms and isolated narrowing of the celiac axis due to the vast collateral circulation.15,16
Paulsen, et al.,17 showed that hepatic artery blood flow is increased after OLT (425.7 ± 25.6 mL/ min). Jurim, et al.,4 found that celiac artery compression decreased the hepatic arterial blood flow after OLT to around 200 mL/min during expiration, which corresponds to two thirds of the respiratory cycle and therefore the majority of the perfusion time. Usually, such a phenomenon would be compensated by collateral circulation from the superior mesenteric and pancreaticoduodenal arteries.18 However, the same scenario in a surgically dissected, newly reconstructed artery could induce decreased flow and predispose recipients to thrombosis after OLT. Probably the thrombosis distal to the anastomosis found in our patient lead to an increased resistance to hepatic artery blood flow and eventually to the bleeding through the anastomosis that we found in the second operation. Fortunately, our patient belongs to that reduced group of patient whose hepatic artery thrombosis resolves with surgical reconstruction without retransplantation, as hepatic artery blood flow was restored after thrombectomy in the third operation, apparently due to an insignificant intrahepatic arterial thrombosis component. Lubrano, et al.,7 showed a greater risk of hepatic artery thrombosis in patients with celiac artery compression undergoing OLT (20% vs. 6.9%; p = 0.17); although not statistical significant, probably due to a small sample size, the fact that the incidence of hepatic artery thrombosis increases more than two-fold in this group is clinically significant.
ConclusionMedian arcuate ligament celiac artery compression is an infrequent anatomical variant that should be intentionally evaluated in the recipient at time of hepatic artery reconstruction in OLT(and maybe at recipient evaluation in thin, nutritionally waisted patients), by direct examination or through imaging studies, to prevent potentially fatal complications, such as early-onset hepatic artery thrombosis and bleeding, as seen in our patient.