We report an example of a cystic hepatic angiosarcoma that to our knowledge has not been previously described. The patient was a 70 year old woman who was admitted to the emergency room because of hypovolemic shock. A computed tomography showed four heterogeneous hepatic cystic masses varying from 2.5 to 11.2 cm; one of these with rupture and formation of a subcapsular hematoma. The cyst wall was lined by several layers of neoplastic epithelioid and spindle shaped endothelial cells that in some areas extended to the underlying stroma. They expressed CD31 and CD34, and were negative for cytokeratin. The patient is alive with residual hepatic cystic angiosarcoma. However, follow up is too short to be significant.
Angiosarcomas are malignant mesenchymal vasoformative neoplasms that arise in various soft tissues and visceral organs. The most common sites, in decreasing order, are the skin, breast, deep soft tissues, liver, adrenal gland and bone.1–3 Primary angiosarcoma of the liver is an uncommon vascular neoplasm that is usually solid and associated with poor prognosis. The largest series of hepatic angiosarcomas includes 168 cases none of which were described as cystic.4 The purpose of this study is to report what appears to be the first example of a cystic hepatic angiosarcoma.
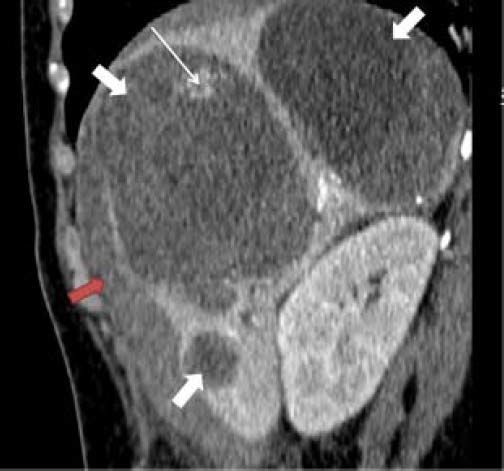
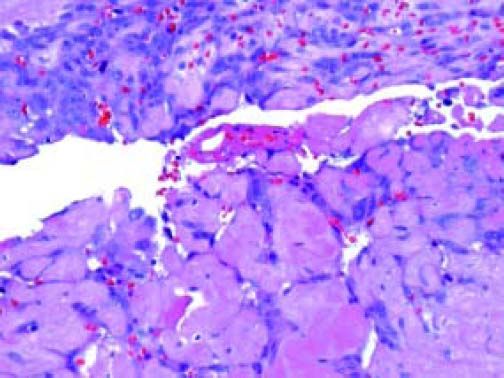
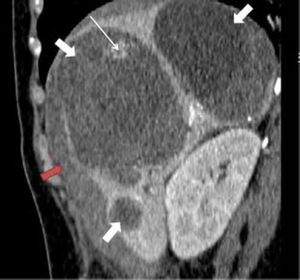
Clinical HistoryThe patient was a 70 year old woman with no history to exposure to vinyl chloride, inorganic arsenic or steroids. One month prior to admission she developed abdominal pain accompanied with diarrhea. She was admitted to the emergency room because of hypovolemic shock and she received intravenous saline solution without response. A computed tomography showed four heterogeneous hepatic cystic masses varying from 2.5 to 11.2 cm, one of these with rupture and formation of a subcapsular hematoma (Figure 1). The patient underwent an exploratory laparotomy to establish hepatic hemostasis and drainage of one of the cysts; during surgery 2 L of blood were found in the peritoneal cavity. Because of the clinical diagnosis of liver abscess after laparotomy, the patient received antibiotic therapy.
Material and MethodsMultiple sections of the cystic liver tumor were available for review. From representative paraffin blocks additional sections were obtained for immunohistochemical analysis. The following antibodies were used:
- •
CD31 (BioSB, Santa Barbara CA, 1:50).
- •
CD34 (BioSB, Santa Barbara CA, 1:50).
The slides were analyzed by two pathologists. The immunohistochemical reactions were interpreted as positive when the cytoplasm of the neoplastic cells was stained.
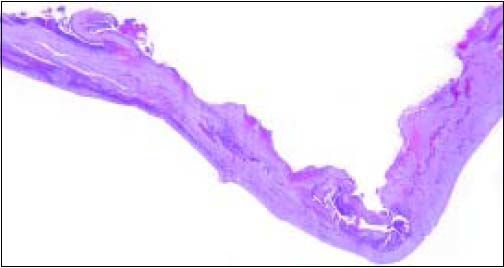
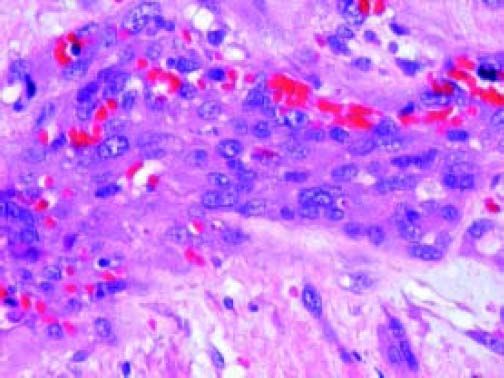
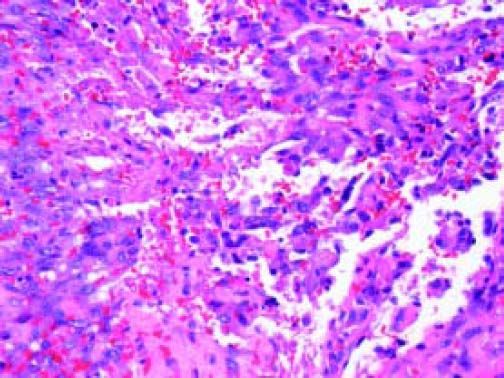
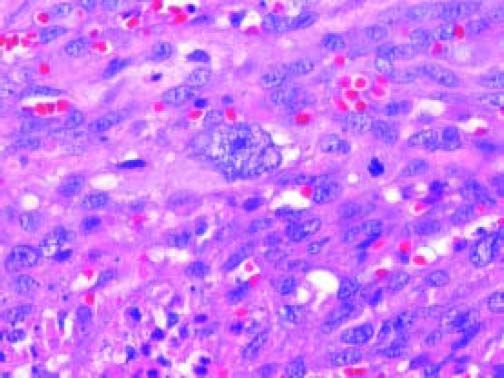
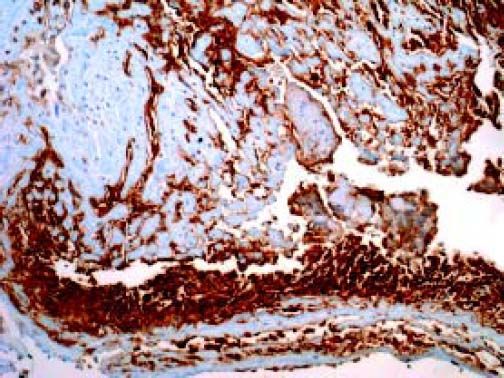
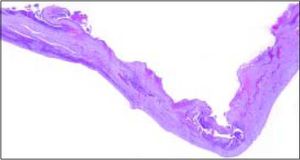
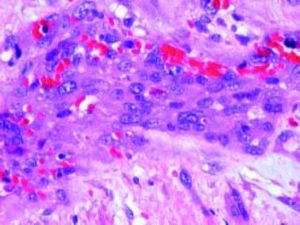
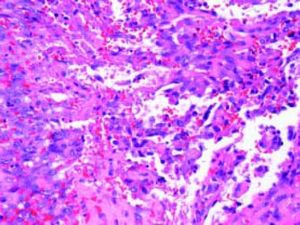
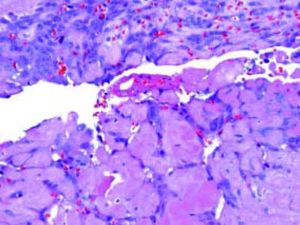
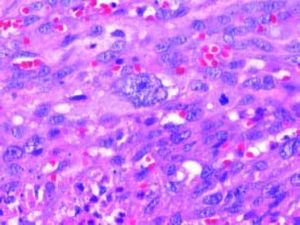
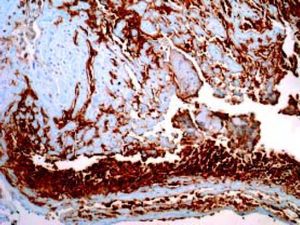
Gross and microscopic featuresThe specimen consisted of a laminar fragment of cyst wall measuring 2 × 1 cm (Figure 2). It had haematic content with clotted blood. Microscopically, the external surface of the cyst wall had a rim of hepatocytes while several layers of spindle shaped or epithelioid neoplastic cells covered the luminal surface (Figures 3 and 4). Small vascular channels lined by low cuboidal cellsseparated by hyalinizedstroma where present in the wall of the cyst (Figure 5). The epithelioid cells had abundant eosinophilic cytoplasm while the spindle cells displayed eosinophilic elongated cytoplasm. Both neoplastic cells showed prominent atypia with nucleomegaly, prominent nucleoli, clumped chromatin and nuclear membrane irregularities (Figure 6). Abnormal mitotic figures and focal areas of hyalinized collagen with nests of neoplastic spindle cells were also seen. These histologic features are diagnostic of angiosarcoma. The neoplastic cells expressed CD31 and CD34 (Figure 7), and were non reactive for cytokeratin AE1/AE3. This immunoprofile is consistent with angiosarcoma.
Angiosarcoma is the most common primary mesenchymal malignancy of the liver which accounts for one third of primary liver sarcomas, 1.8% of all hepatic malignant tumors and only 4% of all angiosarcomas in all anatomic sites.5–7 These tumors usually occur in patients between 50-70 years of age with a higher incidence in males (4:1).8,9 The clinical symptoms are nonspecific, the most common being abdominal pain, weakness, weight loss and hepatomegaly.9
Several risk factors have been identified for the development of hepatic angiosarcoma including exposure to inorganic arsenic, chronic exposure to thorotrast, vinyl chloride, radium, possibly copper, androgenic anabolic steroids and chronic idiopathic hemochromatosis. In 60% of cases there are no risk factors and these angiosarcomas are considered idiopathic.5,10,11
From 2004 to 2007 the SEER Program (Surveillance, Epidemiology and End Results) collected 207 patients with angiosarcoma (28 epithelioid angiosarcoma-13.5%-). The median age was 63 years, 39% (80) were females, 25% (42) were localized and 75% (127) had already metastasized; the tumor size varied from 6.1 to 12cm; the median overall survival was 1 month; most tumors were metastatic at presentation and the majority did not undergo surgical therapy;5 none of them were described as cystic with formation of a subcapsular hematoma; the current case was cystic and bled. In several series multifocal tumors had been identified in approximately 100% of cases, 74.3% have shown 10 or more lesions; 91.4% has been bilateral and from 2.6 to 20 cm.8
The definitive diagnosis is established by the pathologic examination of a biopsy or resected specimen. Histological features include the presence of endothelial neoplastic cells with epithelioid or spindle appearance with pleomorphic and hyperchromatic nuclei and prominent nucleoli, and formation of cytoplasmatic vascular spaces.9 Main differential diagnoses include epithelioidhemangioendothelioma, intrahepatic cholangiocarcinoma and hypervascular metastasis.12
To our knowledge, there has been no report of a cystic hepatic angiosarcoma, although we found a case of cystic angiosarcoma located in the adrenal gland5,13 and one hepatic angiosarcoma in a 7 year old boy which was partially cystic and 10 × 9cm in size.14
The current case presented with a subcapsular hematoma due to rupture of a cystic tumor. In the English literature we found a case of hepatic angiosarcoma complicated by spontaneous hepatic rupture in a 68 year old female farmer who presented with acute onset of abdominal pain and shock.15
Primary hepatic angiosarcomas progress rapidly and most patients are diagnosed at advanced stage. The overall survival was estimated at 6 months. The majority of patients die within a year after diagnosis and only 3% survive more than 2 years.7,10 Extrahepatic metastatic disease may be seen in approximately 60% of patients at presentation, generally in the lungs and spleen (60% of cases).8,12
Because angiosarcoma of the liver is unusual, very little information regarding optimal management is available and this needs to be addressed empirically.16 Surgery is the definitive treatment and may improve survival in some cases.9 Radical surgery with adjuvant chemotherapy appears to be the most promising treatment with the possibility of cure if the tumor is solitary and diagnosed early. The reported median survival stands around 17 months.12 Chemotherapy may help for patients with advanced hepatic angiosarcoma.17 Park,et al. reported that angiosarcomas treated with transcatheter arterial chemoembolization have a reasonable positive response.18 Liver transplantation is not recommended due to rapid recurrence and early mortality.1,19,20
The patient is alive with residual hepatic cystic angiosarcoma; she received liver chemmoembolization without tumor response, however, follow up is too short to be significant.