Laparoscopic splenectomy (LS) is a supportive intervention for cirrhotic patients. However, its efficacy for patients with cirrhotic portal hypertension (CPH) still needs clarification. Studies indicated YKL-40 might be effective targets for treatment of splenomegaly, however deeper insights are unclear. The aim of this study was to investigate the effect of LS on the formation of portal vein thrombosis (PVT) and serum levels of a fibrosis marker, YKL-40, in patients with CPH.
Materials and methodsA total of 80 patients who underwent LS and 30 healthy controls were investigated in this study. Serum levels of YKL-40 were measured by enzyme-linked immunosorbent assay (ELISA). Demographic characteristics including age and gender were recorded. Clinicopathological and laboratory examinations included the severity of esophageal varices and the presence of viral hepatitis. The liver function was assessed according to the Child–Pugh classification. The incidence of PVT before and after operation was also monitored.
ResultsSerum YKL-40 was significantly increased in CPH patients, and was associated with Child–Pugh score and HBV infection. Furthermore, elderly patients had an increased risk for postoperative PVT. Higher serum YKL-40 was observed in patients with thrombus at postoperative 7, 14 and 21 days than those without thrombus.
ConclusionsLS could reduce serum YKL-40 levels and PVT progression and was a useful treatment for patients <40 years of age with CPH.
Liver cirrhosis is the terminal stage of diverse chronic liver diseases, which is regarded as the leading cause of portal hypertension [1]. Portal hypertension is a multiple organ dysfunction syndrome (MODS) characterized by elevated portal vein pressure and abnormal hemodynamics [2]. However, the pathogenesis of cirrhotic portal hypertension (CPH) characterized by the opening of portal collateral circulation, ascites and splenomegaly [3] has not been fully elucidated. Splenectomy is one of the commonly used devascularization procedure in clinical practices, which could reduce portal vein pressure, correct hypersplenism and improve liver function [4]. Though it is considered that liver transplantation is a good way for treatment of cirrhotic portal hypertension [5,6], in some countries or regions, its application is limited by too many patients and very limited donor. Thus under this condition, splenectomy becomes a good alternate choice, especially for severe patients with hypersplenism, hemorrhage due to splenic rupture, severe cirrhosis and varicosity.
Over decades, laparoscopic splenectomy (LS), as a therapeutic modality, has become the standard approach for most splenectomy cases, which has the advantages of less trauma and hemorrhage, fewer postoperative complications, and shorter hospitalization as compared with traditional open splenectomy (OS) [7]. However, the incidence of complications after LS is relatively high due to the abnormal preoperative liver function, accompanied by hypoproteinemia and poor coagulation function in patients with portal hypertension [8]. Portal vein thrombosis (PVT) is defined as occlusive thrombosis of the main portal veins, mesenteric vein, inferior veins or splenic veins, leading to ischemic intestinal necrosis, gastrointestinal bleeding and liver failure [3]. It has become increasingly clear that PVT after splenectomy is not a rare complication in CPH patients with an incidence of 5–25% [9].
YKL-40, also called Chitinase-3-like 1 or human cartilage glycoprotein 39, is a glycoprotein containing 383 amino acids with a molecular weight of 40kDa. Numerous studies have shown that YKL-40 is involved in the pathophysiological processes of inflammation, cell migration, tissue remodeling, fibrosis and tumorigenesis. With regard to liver cirrhosis, YKL-40 serum levels are significantly increased in patients with alcoholic cirrhosis, post-hepatitic cirrhosis, non-cirrhotic fibrosis and hepatitis C virus (HCV)-induced liver fibrosis [10,11]. Previously, Wang et al. showed that YKL-40 acted as a crucial biomarker involved in the remodeling of spleen tissues in patients with portal hypertension. Additionally, YKL-40 inhibitors or antibodies might be effective targets for treatment of splenomegaly [12]. Therefore, we speculated that serum YKL-40 was closely associated with PVT in patients with portal hypertension. However, the expression and clinical significance of YKL-40 protein in patients with CPH and the association between YKL-40 and PVT after LS remain to be explored.
In light of these, the objective of the present study was to investigate the underlying effect of LS on the formation of PVT and the levels of serum YKL-40 in patients with CPH. This study may provide more clinical evidences for LS for reducing PVT formation in treatment of cirrhotic portal hypertension and give deeper understanding for role of serum YKL-40 concentration for cirrhotic patients.
2Material and methods2.1Study populationA total of consecutive 80 CPH patients (male/female, 63/17) with a mean age of 43 years (range, 34–56 years) undergoing LS were recruited for this study who were admitted to Chinese PLA General Hospital between June 2011 and December 2017. All patients meeting the inclusion criteria during the study period were consecutively included. All patients had cirrhosis, hypersplenism, varicosity, splenomegaly or hemorrhage due to splenic rupture. The clinical exclusion criteria were as follows: (1) patients with cardiopulmonary dysfunction; (2) patients with prehepatic or retrohepatic portal hypertension; (3) patients with severe medical diseases. Meanwhile, age- and gender-matched healthy volunteers (n=30) were enrolled as controls in this study. Peripheral blood samples were collected before and after surgery. All participants were signed informed consent before performing analgesia and follow up, and this study was approved by the ethics committee of Medical Faculty of Chinese PLA General Hospital.
2.2Surgical proceduresThe operation was performed under general anesthesia with tracheal intubation. The patients were placed in the right semidecubitus position and a Trocar with a diameter of 12mm was introduced into approximately 1cm inferior to the umbilicus. The abdominal cavity was insufflated with 8mmHg CO2 and a 30° laparoscope was then inserted. A main operating hole was opened at inferior spleen margin in the left midclavicular line. The other two Trocars were separately implanted on the right-sided ligamentum teres hepatis and left midclavicular line under the costal margin as the auxiliary operating holes. Perisplenic ligaments were dissociated using a vascular occlusion device, and the spleen was freed. The resected spleen was placed in a plastic sac and cut into pieces. All incisions were sutured after removing the fragmented spleen from the abdomen.
2.3Data collectionDemographic and clinical data including age, gender, the severity of cirrhosis or esophageal varices and the presence of hepatitis virus infection or portal vein thrombosis were recorded. The severity of cirrhosis was graded according to Child–Pugh classification (A, 5–6 points; B, 7–9 points; C, 10–15 points). Hepatitis B virus (HBV) or HCV infection was detected by means of polymerase chain reaction (PCR) assays for HBV or HCV. All patients were followed-up for 6 months.
2.4Determination for serum YKL-40One day preoperatively and on postoperative day 1, 3, 7, 14 and 21, peripheral blood samples (5ml) were collected from each patient. The samples were centrifuged at 3000rpm for 10min at 4°C and stored at −70°C until analysis. The serum levels of YKL-40 were then determined using commercial ELISA kit (BD Biosciences, San Diego, CA, USA) on an Elecsys 300 analyzer (Roche Diagnostics) following the manufacturer's protocols.
2.5Statistical analysisAll data were presented as mean±standard deviation (SD) and analyzed by SPSS version 22.0 (SPSS, Chicago, IL, USA). Comparisons between groups were performed using two-sided Student's t test. P-value <0.05 was considered statistically significant.
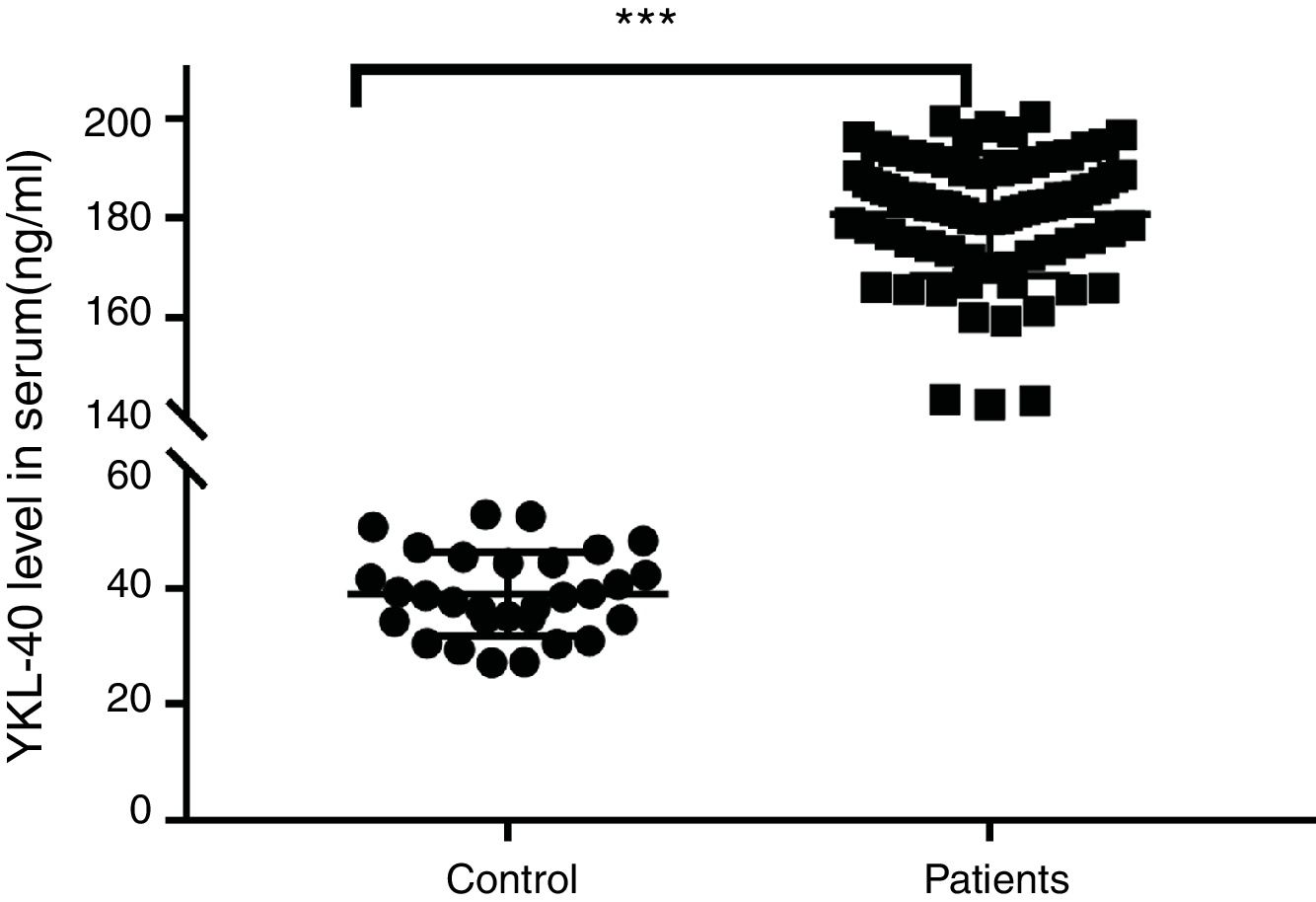
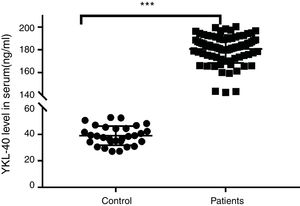
3Results3.1Serum YKL-40 levels were upregulated in patients with CPHThe serum levels of YKL-40 in CPH patients (n=80) and healthy controls (n=30) were accessed by ELISA. The data revealed that higher expression of YKL-40 in CPH subjects than that in controls (P<0.001; Fig. 1). We concluded that serum YKL-40 was upregulated in patients with CPH, which is likely to be a molecular marker of CPH. The indication for splenectomy and the outcomes of patients were shown in Table S1.
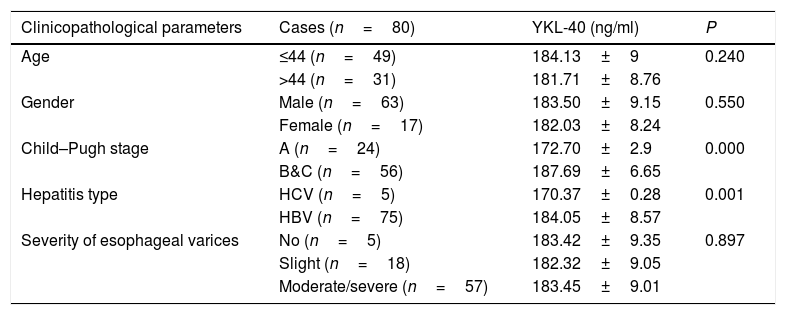
3.2Serum YKL-40 was associated with liver function in patients with CPHAccording to the Child–Pugh scoring system, 24 CPH patients were categorized as class A with mean YKL-40 levels of 172.70ng/ml and 56 as class B and C who had mean YKL-40 levels of 187.69ng/ml (P=0.000; Table 1). HBV infection was the main cause of CPH (93.75%). Additionally, patients with HBV-related CPH had higher YKL-40 levels than those with HCV infection (P=0.001; Table 1). No statistically significant associations were found in the other variables including age, gender, the severity of esophageal varices (P>0.05; Table 1). All data suggested that a significantly increased serum YKL-40 was noted in CPH patients who had a higher Child–Pugh score and HBV infection.
Relationship between serum YKL-40 expression and clinicopathological parameters in patients with CPH.
| Clinicopathological parameters | Cases (n=80) | YKL-40 (ng/ml) | P |
|---|---|---|---|
| Age | ≤44 (n=49) | 184.13±9 | 0.240 |
| >44 (n=31) | 181.71±8.76 | ||
| Gender | Male (n=63) | 183.50±9.15 | 0.550 |
| Female (n=17) | 182.03±8.24 | ||
| Child–Pugh stage | A (n=24) | 172.70±2.9 | 0.000 |
| B&C (n=56) | 187.69±6.65 | ||
| Hepatitis type | HCV (n=5) | 170.37±0.28 | 0.001 |
| HBV (n=75) | 184.05±8.57 | ||
| Severity of esophageal varices | No (n=5) | 183.42±9.35 | 0.897 |
| Slight (n=18) | 182.32±9.05 | ||
| Moderate/severe (n=57) | 183.45±9.01 |
CPH, cirrhotic portal hypertension; HBV, hepatitis B virus; HCV, hepatitis C virus.
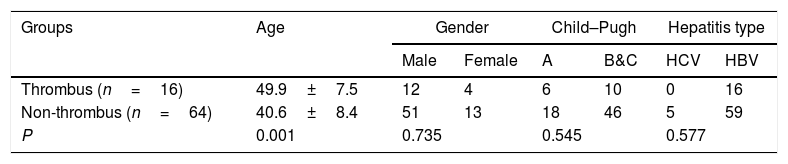
Postoperatively, all patients were divided into thrombus group (n=16) and non-thrombus group (n=64) according to abdominal ultrasonography detection of portal vein system. The rate of postoperative thrombosis was 21.2%. To investigate the risk factors for the PVT after LS operation, the following risk factors were assessed: age, gender, Child–Pugh and infection of hepatitis viruses. As a result, age was an independent predictor for postoperative PVT (P=0.0001; Table 2).
Association between thrombosis and age, sex and liver function of CPH patients.
| Groups | Age | Gender | Child–Pugh | Hepatitis type | |||
|---|---|---|---|---|---|---|---|
| Male | Female | A | B&C | HCV | HBV | ||
| Thrombus (n=16) | 49.9±7.5 | 12 | 4 | 6 | 10 | 0 | 16 |
| Non-thrombus (n=64) | 40.6±8.4 | 51 | 13 | 18 | 46 | 5 | 59 |
| P | 0.001 | 0.735 | 0.545 | 0.577 | |||
CPH, cirrhotic portal hypertension; HBV, hepatitis B virus; HCV, hepatitis C virus.
Older patients had an increased risk for venous thrombosis.
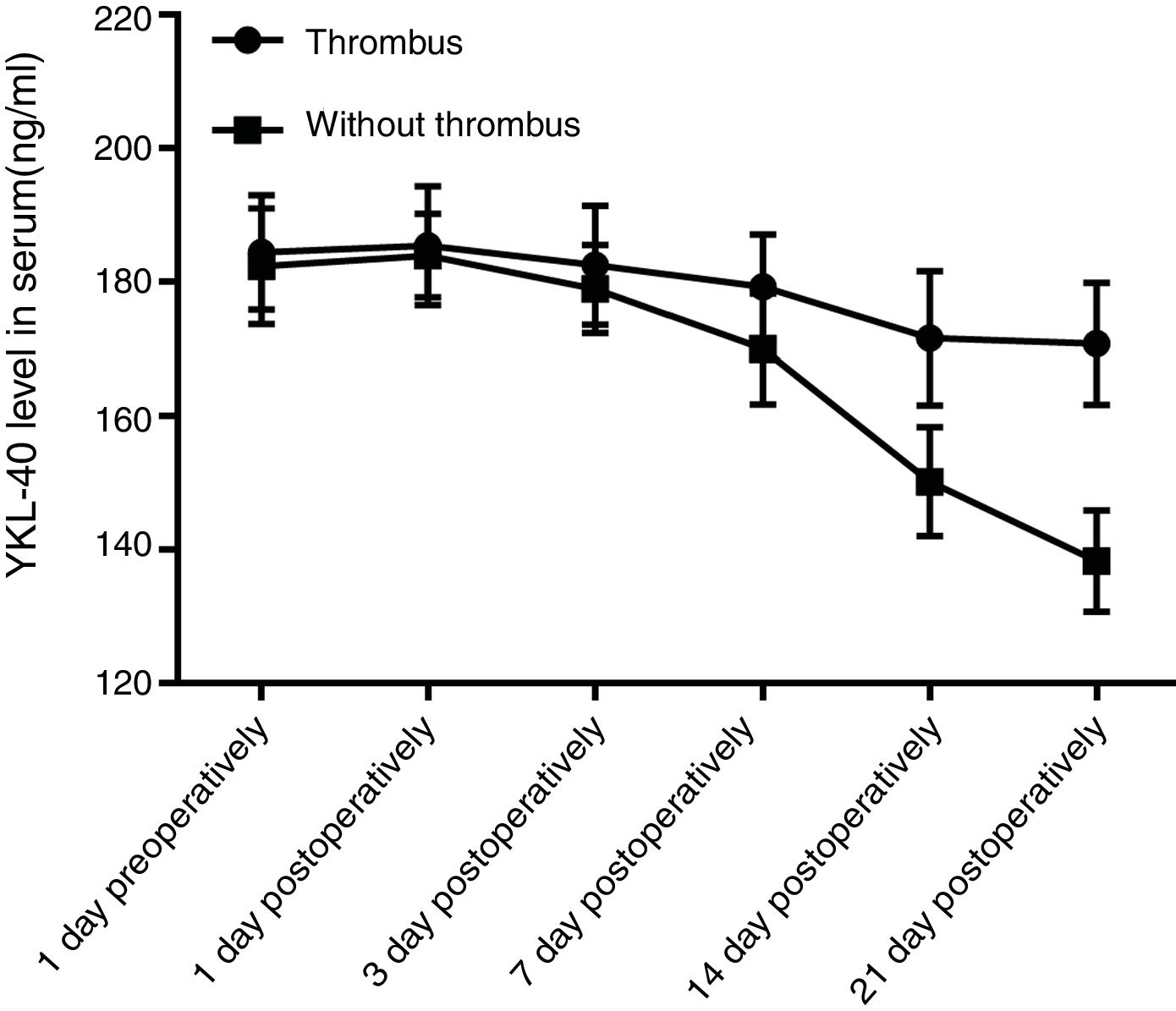
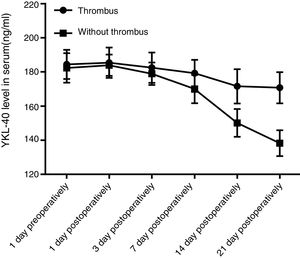
We further determined whether serum YKL-40 concentration was associated with the incidence of postoperative PVT. As shown in Fig. 2, there were no significant differences in YKL-40 expression between preoperative and postoperative in patients with thrombus, while patients without thrombus had the gradually decreased YKL-40 levels after the operation. More importantly, at 7, 14 and 21 days after surgery, serum YKL-40 expression levels in the thrombus group was significantly higher than that in the non-thrombus group (all, P<0.01).
4DiscussionLiver cirrhosis is a common chronic disease characterized by irreversible distortion of liver architecture, regenerative nodules formation and hepatic necrosis caused by diffuse inflammation in the liver and gallbladder [13]. In general, liver cirrhosis occurs simultaneously with hepatic regeneration, inflammation, necrosis, and degeneration induced by the activation of hepatic satellite cells. Liver cirrhosis might be complicated by the retardation of portal venous blood flow (PVBF), leading to portal hypertension featured with splenomegaly and hypersplenism, esophagogastric varices, hematemesis and ascites [14]. Abnormal liver function, coagulation dysfunction and megalosplenia are frequent events in patients with CPH.
A large quantity of evidence has revealed that multiple biomarkers are involved in the occurrence and progression of CPH [15]. Measuring serum biomarker levels facilitates the diagnosis and prognosis of CPH. YKL-40, a member of family 18 glycosyl hydrolases was initially identified in human MG63 osteosarcoma cells [16]. In recent years, YKL-40 has been found to be expressed in human embryonic stem (ES) cells [17], tumor-associated macrophages (TAM) [18], osteoarthritis chondrocytes [19], and differentiated vascular smooth muscle cells (VSMCs) [20]. In a randomized study of 86,258 individuals, elevated YKL-40 levels were observed in patients with alcoholic liver cirrhosis [21]. Huang et al. demonstrated that YKL-40 was a serum biomarker of liver fibrosis, in identifying HBV-related liver fibrosis [22]. In our study, the increased YKL-40 concentration was also observed in CPH patients compared to the healthy controls. Moreover, patients with severe liver cirrhosis (Child–Pugh classes B and C) and HBV infection exhibited higher levels of serum YKL-40 relative to those with moderate liver cirrhosis (Child–Pugh classes A) and HCV infection, respectively.
The treatment technologies for CPH are becoming increasingly mature and innovative through the long-term clinical practices. Unfortunately, the current surgical outcomes have not been satisfactory. In the recent years, the improvement of liver transplantation has broadened the range of options for treatment of patients with portal hypertension. For patients with portal hypertension accompanied by gastrointestinal bleeding and severe liver dysfunction, liver transplantation is a radical approach [23]. However, liver transplantation is not a necessary choice due to its high risk, high technical requirements, and postoperative immune rejection [24]. The objective of surgical treatment of portal hypertension is to reduce the pressure on the portal vein system and eliminate hypersplenism. Based on this principle, plenectomy has been widely accepted. Splenectomy could not only inhibit the development of hepatic fibrosis and reduce PVBF, but also ameliorate hypersplenism and improve immune function. With the continuous improvements of surgical techniques and laparoscopic surgical instruments, compelling evidence has delineated the safety and feasibility of LS in patients with portal hypertension due to its advantages of less trauma, bleeding, and pain, faster recovery, and lower operative mortality. Although LS has the advantage of minimally invasive surgery, the high incidence of postoperative complications including fever, pleural effusion, subphrenic abscess, incision infection, abdominal bleeding, gastric perforation and PVT is a major challenge for surgeons [25]. PVT is one of the serious complications of LS, which further increases the risk of liver damage, gastrointestinal bleeding, and intestinal necrosis. Our data suggested that thrombus patients were older than non-thrombus patients after LS, indicating that age was an independent predictor for postoperative PVT. In this study, we provided the first demonstration that the serum YKL-40 was closely correlated with the incidence of PVT. However, there are still flaws in our study. For example, the samples are too small and lacking the research about pathological mechanisms by which YKL-40 affected postoperative PVT formation. In our future study, we will enlarge our samples and further investigate the role of YKL-40 in vivo.
Here, we concluded that highly expressed YKL-40 in patients with CPH was significantly associated with the severity of liver cirrhosis and HBV infection. Furthermore, LS was shown to strongly affect the serum concentration of YKL-40 to further influence postoperative PVT formation. These findings will provide some clues that LS is an alternative to open splenectomy for reducing PVT formation and serum YKL-40 concentration for cirrhotic patients.
Author contributionRuizhao Qi conducted most of the experiments and wrote the manuscript; Xin Jin, Haida Shi, Chengfang Wang and Huixing Li conducted the experiments and analyzed the data; Xianjie Shi designed the study and revised the manuscript.
FundingNone.
Conflict of interestThe authors have no conflicts of interest to declare.