A 72-year-old female with a history of autoimmune hepatitis-related cirrhosis, osteoporosis, and hypertension was admitted with recurrent episodes of confusion and drowsiness over the course of two years. On each occasion, the patient demonstrated fluctuating confusion with drowsiness and was disorientated to time and place. A marked liver flap was present on examination with no other features of hepatic decompensation. These episodes were associated with raised serum ammonia levels, normal neuroimaging findings and no features to suggest a precipitating illness. They became more frequent, severe and longer in duration in early 2014, prompting three hospital admissions in 2 months despite being on optimal medical therapy of rifaximin, twicedaily enemas and maximally tolerated lactulose.
Most recently she was admitted with a two-day history of increasing confusion, wandering around the house, and drowsiness. There were no features of jaundice, ascites, gastro-intestinal bleeding or sepsis. She was opening her bowels two to three times per day. Examination demonstrated marked confusion (abbreviated mental test score 4/10), drowsiness with a Glasgow Coma Score of 13/15 and a marked liver flap. There was no focal neurology, and the remainder of the examination was unremarkable except for 2cm splenomegaly. Initial blood tests demonstrated bilirubin: 19 μmol/L, ALT 54 IU/L, AST 50 IU/L, ALP 90 IU/L, albumin 33g/L, creatinine 63 umol/L, sodium 139 mmol/L, PT 12.8, CRP 2 mg/L and serum ammonia of 93 μmol/L. Oesophagoduodenoscopy (OGD) showed one small varix (grade 1) with no evidence of red signs or recent bleeding, while an electroencephalogram demonstrated slow waves suggestive of cerebral dysfunction, but no epileptiform activity. Despite an increase in laxatives, the patient’s confusion persisted with no appreciable change in her liver function tests, or her ammonia level. Given this patient’s otherwise good liver function, with a MELD score of 8 and unexplained, recurrent encephalopathy, a triple phase computed tomography (CT) of her liver liver was conducted to investigate for a large spontaneous porto-systemic shunt (SPSS)1 which could account for her symptoms.
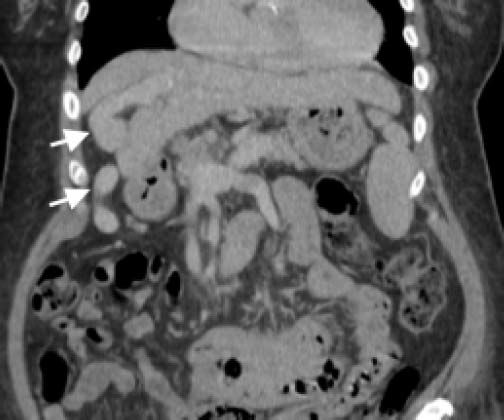
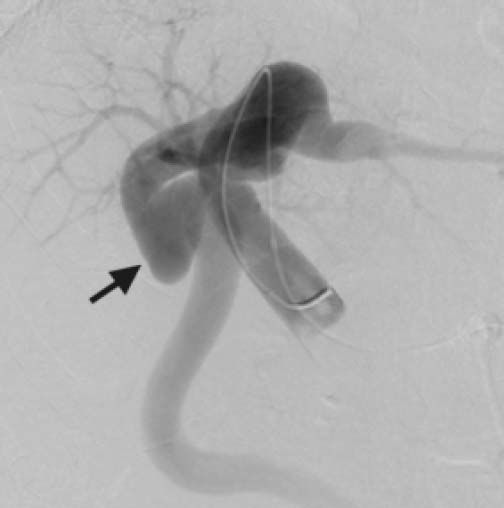
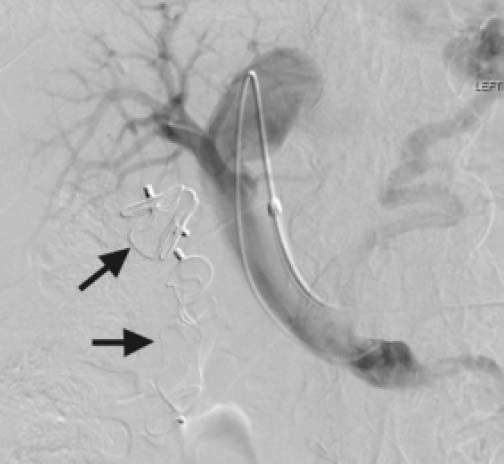
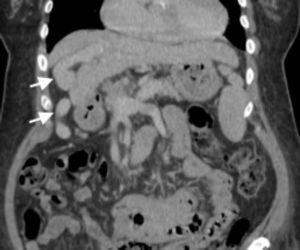
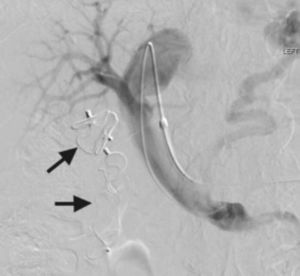
ImagesThe CT demonstrated a large left portosystemic shunt. Since she was not a transplant candidate due to her age, she subsequently underwent embolisation of the shunt via a trans-jugular approach. A venogram performed from the main portal vein during the procedure confirmed the presence of a large recanalised umbilical vein, which was subsequently embolised. Portal venous pressure before embolisation was 26 mmHg, rising to 31 mmHg following embolisation. Details are shown in figures 1–3.
Over the following 3 days there was marked improvement in the patient’s confusion, with resolution of her asterixis. An OGD was performed prior to discharge, which demonstrated no aggravation of her oesophageal varix or new gastric varices. The patient remains well 2 months after the procedure, with minimal confusion and no complications.
DiscussionHepatic encephalopathy (HE) is a complex neuropsychiatric syndrome seen frequently in patients with advanced cirrhosis and is usually triggered by a precipitating event such as gastro-intestinal bleeding or sepsis. In some patients, HE can present and persist in the absence of such events. In this latter group of patients, large SPSS are found at a high rate2 and are believed to contribute to the encephalopathic process by the portal flow steal mechanism.3,4 Recurrent or persistent encephalopathy in the setting of early cirrhosis and no clear precipitant should prompt investigation for such shunts. Embolization of these shunts has been explored as a therapeutic intervention to manage encephalopathy in selected patients with persistent HE which is resistant to maximal medical therapy.3 Concerns have been raised regarding the aggravation of portal hypertension and subsequent increased risk of variceal haemorrhages following this procedure.5 In a multicentre retrospective cohort study of 37 patients undergoing SPSS embolization with mean follow-up of 697 ± 157 days, 48.6% of patients had no further episodes of HE, while the frequency and severity of HE was significantly reduced in the remainder.6 Regarding the safety of the procedure, one patient had capsular bleeding requiring surgical intervention and two patients developed de novo oesophageal varices during follow up. The authors concluded that a MELD cut-off of 11 was safe for embolization of porto-systemic shunts. A recent retrospective case-control study of 34 patients compared SPSS embolization against best medical therapy.7 This demonstrated significant improvements in both patient survival (100% vs. 60%) and HE-free survival (19% vs. 70%) at 2 years of follow-up in patients with MELD < 15 without hepatocellular carcinoma. Post-procedure, three patients developed de novo, or had progression of their oesophageal varices with no subsequent bleeds.
ConclusionIn patients with Child A or early B cirrhosis who are otherwise stable, unexplained recurrent encephalopathy should prompt investigations for porto-systemic shunts. In selected patients with no options for liver transplantation and preserved liver function, embolization of such shunts is safe and effective. Patients should be followed up and screened post-embolization for development of portal hypertension, more specifically for oesophageal and gastric varices.
Abbreviations- •
ALP: alkaline phosphatise.
- •
ALT: alanine aminotransferase.
- •
AST: aspartate aminotransferase.
- •
CRP: C-reactive protein.
- •
CT: computed tomography
- •
HE: hepatic encephalopathy.
- •
MELD: Model for End-stage Liver Disease
- •
OGD: oesophagoduodenoscopy.
- •
PT: prothrombin time
- •
SPSS: spontaneous portosystemic shunt
- •
UKELD: United Kingdom Model for End-stage Liver Disease
No financial support was received for this manuscript