Objective. To identify changes in hepatitis B epidemiology after the implementation of the nationwide vaccination program in Turkey, hepatitis B virus (HBV) and related tests performed over a period of 11 years (2000-2010) at a reference centre were retrospectively overviewed and statistically analysed for trends.
Results. Assay results for Hepatitis B surface antigen (HBsAg) and e antigen (HBeAg), Anti-HBs, Anti-HBe, Anti-HBc immunoglobulins and HBV DNA as well as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gama-glutamyl transpeptidase (GGT) and alkaline phosphatase (AP) levels, obtained via standardized commercial assays were included in the analysis. Overall, a stable anti-HBs incidence (43.6%) and male predominance in infected individuals were noted. Total Anti-HBc was detected in 43.3% of the Anti-HBs reactive population, demonstrating that the immunity against HBV has still been acquired through virus exposure. An intermediate HBsAg seroprevalence of 6.0% was observed with a significant decrease from 12.3% to 5.0% from 2000 to 2010. Anti-HBe positive infections were more frequent than those with HBe antigenemia (77.1% vs. 18.5%) with a notable increase from 2000 to 2003. HBV DNA was detected in 23.6-25.6% with serological markers of viral replication and was more prevalent in HBeAg positive individuals in parallel with AST, ALT and GGT levels. Evidence for horizontal transfer as the major transmission route was revealed with a reduction of childhood HBV infections, attributable to the ongoing vaccination efforts.
Hepatitis B virus (HBV) infection is a global public health problem affecting a significant portion of the global population.1 More than 2 billion people worldwide have been infected with HBV and an estimated 1 million people die each year from acute and chronic sequelae secondary to HBV infection, including cirrhosis, fulminant hepatic failure, hepatocellular carcinoma.1,2 The global prevalence of HBV infection varies widely. Regions are divided into areas of low, intermediate, and high prevalence.3,4 About 45% of the world's population lives in regions of high prevalence where at least 8% of the population is currently infected. In such regions, perinatal transmission of the virus is frequent and early childhood infections are common. HBs seroprevalence rates between 2-7% define the zones of intermediate prevalence, where infections occur in all age groups. An infection rate < 2% is called as low prevalence and represents only 12% of the global population.3-6 HBs seroprevalence in Turkey is reported to be around 4%, which is in line with other Mediterranean and Middle Eastern countries and fulfills the criteria for intermediate endemicity level.5-9 HBV genotype D has been consistently identified in Turkey, with most prevalent subgenotype D1 and serotype ayw2.10-13
Hepatitis B vaccination is the most effective measure to prevent HBV infection and its consequences.14 HBV vaccines have displayed long-term and stable efficacy.15 Widespread immunization programmes against HBV have been implemented in more than 100 countries and have effectively reduced the acute and chronic infection rates in recent years.15,16 In Turkey, vaccines have been available since the early 1990s, and a nationwide HBV vaccination program has been implemented since 1998 and the vaccines have been provided free of charge for healthcare workers, neonates and family members of the individuals with chronic HBV infection.7 This study was aimed to identify trend changes in HBV epidemiology after the implementation of the nationwide vaccination program by the evaluation of HBV and related laboratory results over a period of 11 years at a reference centre in Turkey.
Material and MethodsStudy designThe study was carried out at the Hacettepe University Hospital, a tertiary care and a major reference centre, located in Ankara, Central Anatolia, Turkey. Ankara (39°56,N-32°52,E) is the capital and second most densely-populated city in Turkey with a population over 4,600,000.17
For the study, Hacettepe University Hospital Central Laboratory records between January 2000 and December 2010 were retrospectively overviewed. Assay result entries for Hepatitis B s antigen (HB-sAg), Anti-HBs, Hepatitis B e antigen (HBeAg), Anti-HBe, Anti-HBc and HBV DNA were sorted individually as well as in combinations. All entries were filtered according to name and birth date so that only the initial record originating from the same individual was accepted for the analyses and results from repeat assays were excluded. If additional HBV assays were performed and recorded as positive within 7 days of the initial assay, the results were considered as simultaneously reactive. The individuals included in the study were further investigated for the results of liver function tests including aspartate aminotransferase (AST), alanine aminotransferase (ALT), gama-glutamyl transpeptidase (GGT), and alkaline phosphatase (AP) levels which were interpreted as described. The study was approved by the local authorities.
Serological-biochemical assays and nucleic acid testingSerological markers of HBV infection were determined by various commercially available immunoas-says throughout the study period. HBsAg, anti-HBs and anti-HBc IgG were determined by chemiluminescent microparticle immunoassays via the Axsym system (Abbott Laboratories, USA) between 20002007 and thereafter via the Architect system (Abbott Laboratories, USA). Anti-HBc IgM, HBeAg, and anti-HBe were determined by microparticle enzyme immunoassay Axsym (Abbott Laboratories, USA). All assays were performed according to the manufacturers, instructions.
HBV DNA was evaluated quantitatively by Digene Hybrid Capture assay (Digene Corporation, USA) during 2000-2004, by Cobas Amplicor realtime PCR (Roche Diagnostic Systems Inc, Germany) from 2005 to May 2008 and thereafter by Cobas AmpliPrep real-time PCR (Roche Diagnostic Systems Inc., Germany). HBV DNA levels expressed as copy mL-1 were converted to IU mL-1 for standardization according to the World Health Organization standards as directed by the manufacturer.
Levels of AST, ALT, GGT, AP, AFP and total bilirubin were determined by using Roche Modular Analyzer Diagnostic kits (Roche Diagnostic Systems Inc, Germany) and thrombocyte counts by Coulter LH 750 and LH 780 (Beckman Coulter, USA).
Statistical analysisRecords between 2000-2010 were retrieved from Hacettepe University Hospital database. R codes were written to filter the data according to name and birth date to identify initial visits to the hospital. Descriptive data are expressed as mean ± standard deviation. Group comparisons were done with independent sample t-test. A chi-square test for trend can be obtained by organizing the observed data into a contingency table with one row for each time period and two columns: the first for the number of individuals with the positive results; the second for the number of individuals with negative results.18 Results were considered statistically significant at p < 0.05. ModelMap, foreign package was used for data manipulation. All statistical analyses were implemented using R-2.13.1 software.19
ResultsParticipant characteristicsGender distribution was noted as 107,941 (51.59%) males and 101,248 (48.41%) females out of 209,189 records sorted for HBV infections. Female to male ratio was 1.11-1.17 and stable throughout the study period except for 2010, where 61.4% of the individuals were males, resulting in a decreased ratio of 0.62. A total of 208,895 records were analysed for age where a stable distribution of individuals among decades were observed (data not shown). The distribution of individuals in first (ages 0-9) and second decades (ages 10-19) were also stable (13.1-16.7% and 9.3-11.3%, respectively) except for a decrease to in 2010, where frequencies of 7.5 and 7.3% were noted for these age groups. A total of 215,855 entries were sorted for the hospital departments where 92.1% (198,673) and 7.9% (17,182) of the samples were noted to originate from adult and pediatric clinics, respectively. For the pediatric samples, 77.6% were from outpatient clinics, 14.8% were from surgery wards and the remaining (7.6%) originated from internal medicine wards and Intensive Care Units (ICUs). Seventy-three point eight percent of the adult individuals (146,620) enlisted for the study were registered at the adult outpatient clinics of the Internal Medicine (including the emergency ward) and Surgery Departments whereas 25.1% and 1.1% were from various hospital wards and ICUs respectively, belonging to the internal medicine and surgery clinics.
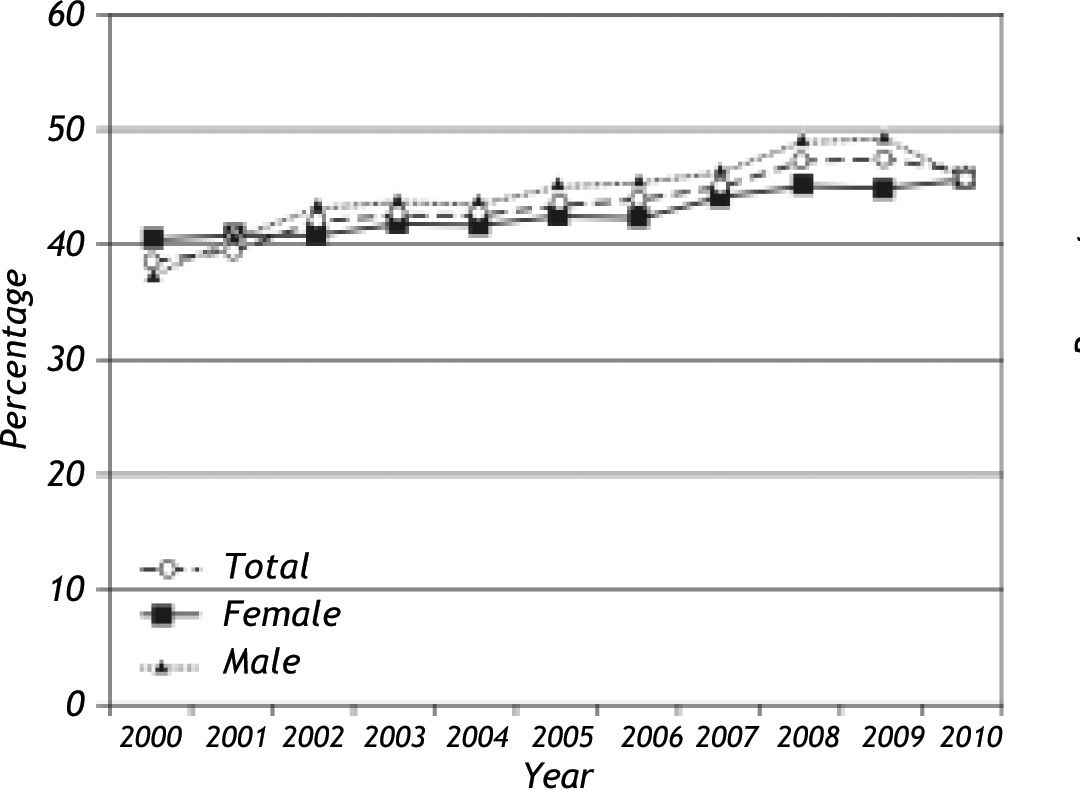
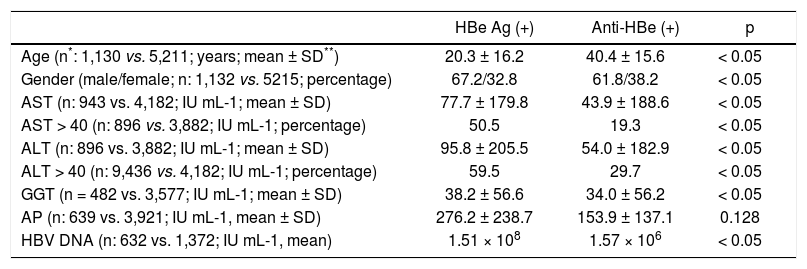
Anti-HBs and Anti-HBc resultsOut of 200518 individuals tested for Anti-HBs, 87,431 (43.6%) were positive. Overall, Anti-HBs incidence was stable through the years (p:0.001) and no significant variation for gender could be observed (Figure 1). The mean age of Anti-HBs reactive individuals was calculated as 32.4 ± 22.3 years and was significantly lower in men than women (31.5 ± 23.5 vs. 33.2 ± 21.1 years; p:0.001). The total Anti-HBc immunoglobulins were further tested in 38.1% (33,339/87,431) of the Anti-HBs reactive population and 43.3% (14,452/33,339) were positive. Anti-HBc IgM was sought in 37,718 anti-HBs reactive individuals where 40 (0.1%) were observed as reactive. Increased ALT levels were noted in 17.1% of the Anti-HBs + Anti-HBc reactive population (data not shown). HBV DNA could be detected in 539 (539/ 2,215, 24.3%) and 414 (414/1,753, 23.6%) of the total anti-HBc and anti-HBc IgM reactive individuals, respectively and significantly more frequent in these groups (p values < 0.05).
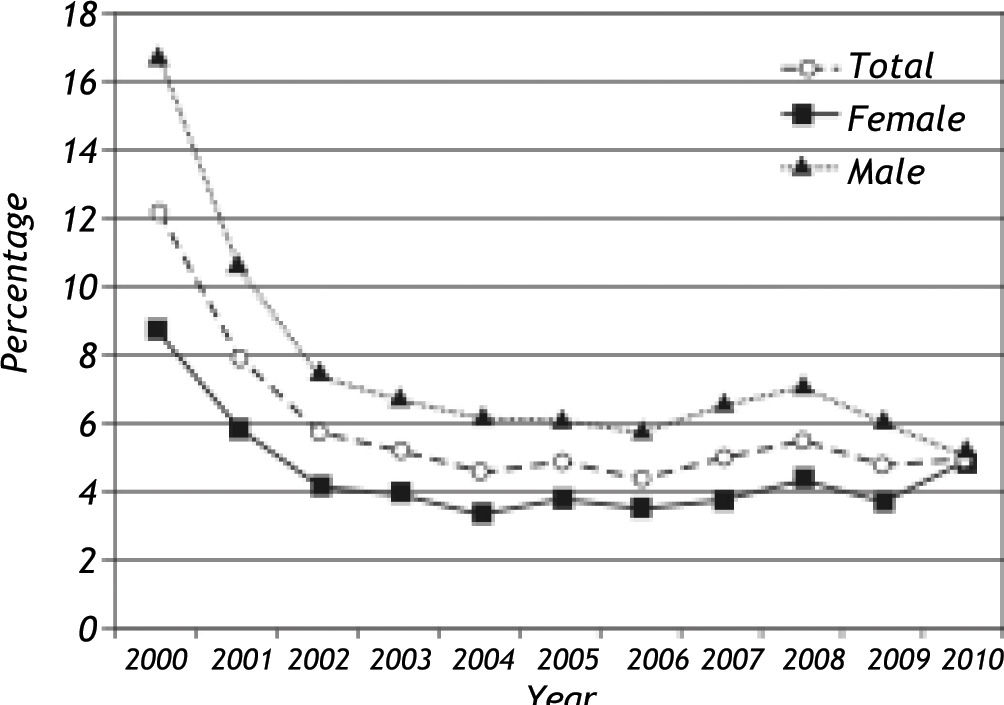
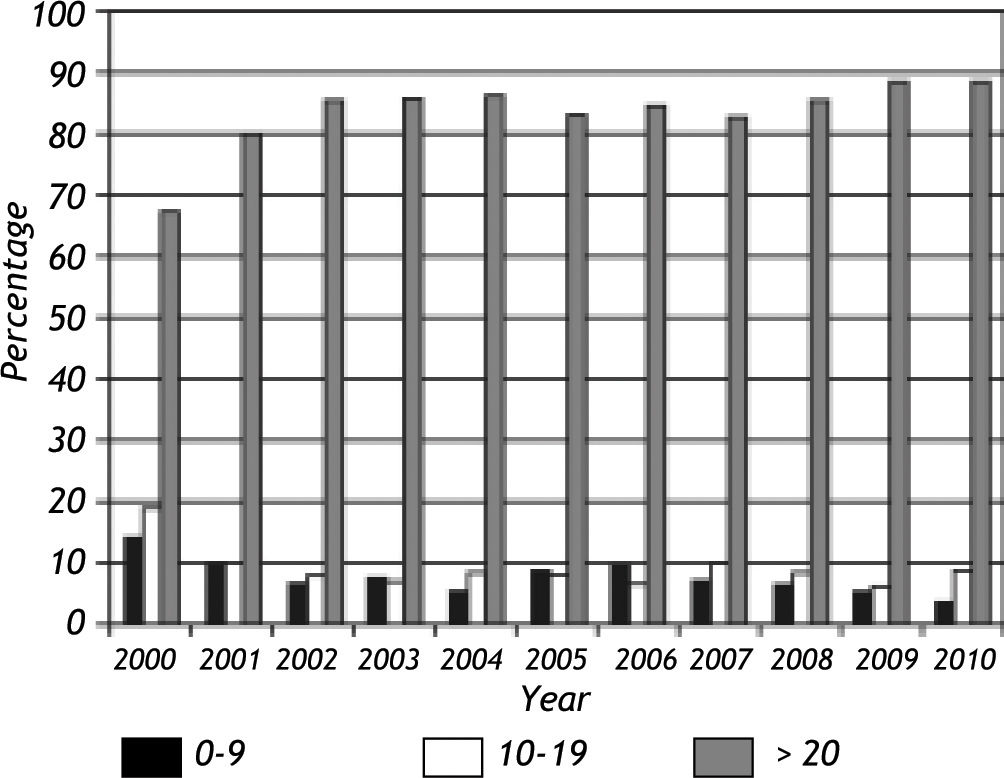
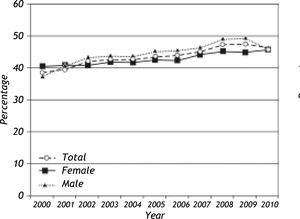
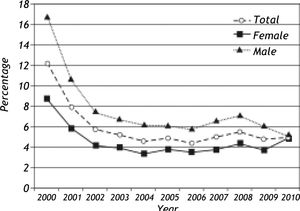
HBs Ag, HBe Ag and Anti-HBe resultsA total of 13,210 HBsAg positive persons were identified out of 221,380 individual tests (6.0%) during the study period. HBsAg reactivity rates according to year are given in Figure 2. Overall, a statistically significant decrease from 12.3% to 5.0% has been noted from 2000 to 2010 (p:0.001) while seroreactivity rate was stable after 2003 (Figure 2). HBsAg detection was more frequent in men than in women (7.3% vs. 4.5%, p:0.001) throughout the study period. The trend for decrease in HBsAg seroreactivity between 2000-2010 were also observed in both genders (16.9% to 5.1% in men and from 8.8% vs. 4.9% in women) (Figure 2). The mean age was consistently lower in individuals with HBsAg reactivity throughout the study period (35.4 ± 27.4 years vs. 38.2 ± 18.2 years, p:0.001, ANOVA p:0.001, data not shown). HBsAg detection in individuals younger than 10 years displayed a statistically-significant tendency to decrease during the study period (p:0.001) (Figure 3) while it was constant for other age groups. HBV DNA could be detected in 1,185 of the 4,636 (25.6%) HBsAg positive individuals and was observed to be significantly more frequent in this group (p:0.0001).
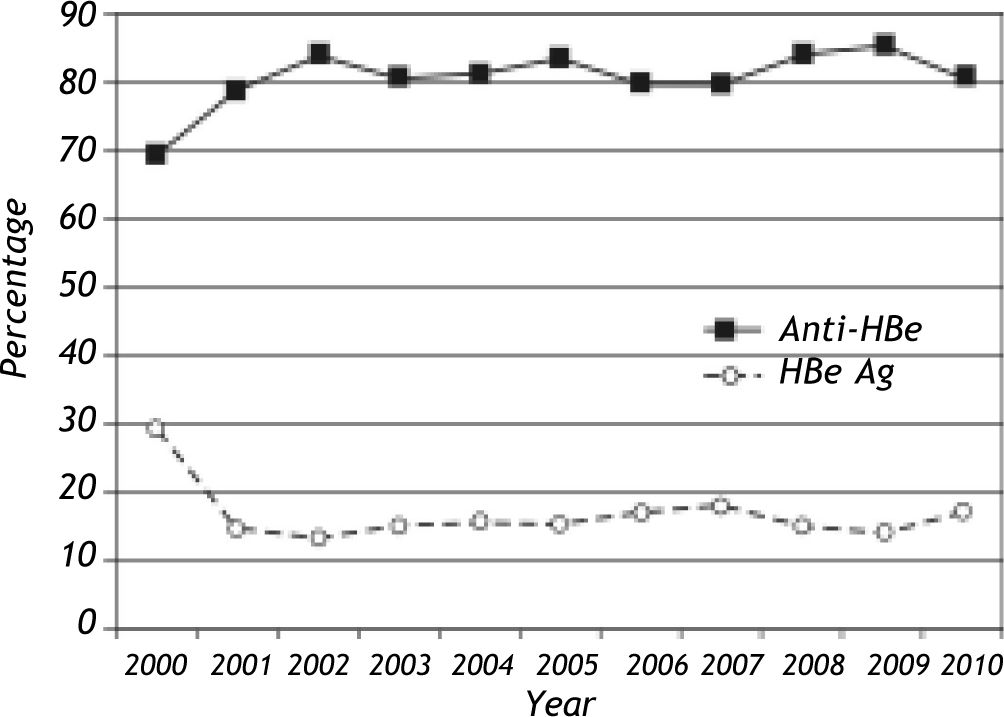
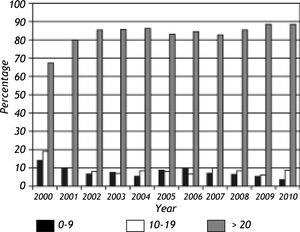
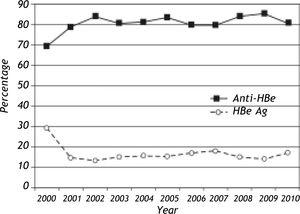
During the study period, HBeAg and Anti-HBe were tested in 7,254 individuals with reactive HBsAg and both were negative in 244 (3.4%). Overall, Anti-HBe positive infections were more frequent than HBeAg positive infections in the study group (5,595/ 7,254; 77.1% vs. 1339/7254; 18.5%). The yearly incidences of HBe and Anti-HBe positive infections are given in figure 4. A notable increase in Anti-HBe positive infections with a parallel decrease in HBe positive infections were observed from 2000 to 2003. The mean age of HBeAg positive individuals were significantly lower than that of Anti-HBe positive individuals (20.3 ± 16.2 years vs. 40.4 ± 15.6 years, p:0.001). The male predominance was also apparent in HBeAg positive infections (67.2% vs. 61.8%, p:0.001). No variations in age distribution in individuals with HBeAg or Anti-HBe reactivity were identified throughout the study period (data not shown). HBV DNA was positive in 1,097 (1,097/4,153, 26.4%) and 1,055 (1,055/3,991, 26.4%) of the HBeAg and anti-HBe antibody reactive individuals, respectively. Detection of HBV DNA was significantly more frequent in persons with HBeAg or Anti-HBe reactivity (p values < 0.05). Concominant HBeAg and Anti-HBe reactivity was observed in 40 samples (40/7254, 0.56%) where 16 (16/40, 40%) were positive for HBV DNA. The mean serum levels of AST and ALT were higher in HBeAg than Anti-HBe positive individuals (p:0.001). Descriptive features and certain laboratory assay results of HBeAg and anti-HBe positive infections are given in table 1.
Certain demographic and laboratory results observed in HBe antigen and anti-HBe immunoglobulin positive infections.
| HBe Ag (+) | Anti-HBe (+) | p | |
|---|---|---|---|
| Age (n*: 1,130 vs. 5,211; years; mean ± SD**) | 20.3 ± 16.2 | 40.4 ± 15.6 | < 0.05 |
| Gender (male/female; n: 1,132 vs. 5215; percentage) | 67.2/32.8 | 61.8/38.2 | < 0.05 |
| AST (n: 943 vs. 4,182; IU mL-1; mean ± SD) | 77.7 ± 179.8 | 43.9 ± 188.6 | < 0.05 |
| AST > 40 (n: 896 vs. 3,882; IU mL-1; percentage) | 50.5 | 19.3 | < 0.05 |
| ALT (n: 896 vs. 3,882; IU mL-1; mean ± SD) | 95.8 ± 205.5 | 54.0 ± 182.9 | < 0.05 |
| ALT > 40 (n: 9,436 vs. 4,182; IU mL-1; percentage) | 59.5 | 29.7 | < 0.05 |
| GGT (n = 482 vs. 3,577; IU mL-1; mean ± SD) | 38.2 ± 56.6 | 34.0 ± 56.2 | < 0.05 |
| AP (n: 639 vs. 3,921; IU mL-1, mean ± SD) | 276.2 ± 238.7 | 153.9 ± 137.1 | 0.128 |
| HBV DNA (n: 632 vs. 1,372; IU mL-1, mean) | 1.51 × 108 | 1.57 × 106 | < 0.05 |
The epidemiological studies revealed that the HBV infection incidence has been decreasing both in the world as well as in Turkey.6,9 Despite this apparent downward trend observed in cross-sectional studies, Turkey is still a member of intermediate endemic areas for HBV infection.7,9 Moreover, the differences in HBV prevalence between western and eastern provinces of Turkey further challenges the estimations.7 This study was conducted in order to assess the changes in HBV epidemiology at a reference centre in Turkey over the period of 11 years via evaluation of yearly trends in the prevalence of serological markers of HBV infection. To the best of our knowledge, this is the most comprehensive single-centre study investigating the HBV epidemiology in Turkey.
An overall anti-HBs seroprevalence of 43.6% (87,431/200,518) was observed in the study, which was stable through the years with no significant variation for gender (Figure 1). The total Anti-HBc immunoglobulins could further be detected in 43.3% of the Anti-HBs reactive population, demonstrating that the immunity against HBV has still been acquired through virus exposure in a considerable portion of the enrolled individuals. These findings also imply that the impact of the national vaccination program on HBV epidemiology has not yet fully come into effect, at least for the study population. This is not surprising since the priority groups targeted for immunization is high risk groups and newborns.7 Furthermore, this observation is indirectly supported by the lack of variations among age groups for anti-HBs reactivity. The mean age of anti-HBs seroconversion was observed to be lower in men (31.5 vs. 33.2 years). Anti-HBc IgM, which is frequently requested by the clinics as a marker of acute infection, was positive in 0.1% (40/37,718) of the anti-HBs reactive population. HBV DNA was detected in 23.6% and was significantly more frequent in individuals with anti-HBc IgM reactivity, suggesting that only a portion of the acute HBV cases display active viral replication.
HBsAg detection is commonly used as the serological marker for the surveillance of persistant HBV infections, either with active hepatitis or in carrier states.2,3 We have observed an overall rate of 5.96% (13,210/221,380) for HBsAg positivity during the study period that displayed a statistically-significant decrease from 12.3% to 5.0% from 2000 to 2010, which was observed in both genders, although seroreactivity rate was stable after 2003 (Figure 2). We consider the decrease in HBsAg seroprevalence to represent a true reduction in HBV transmission due to vaccination and/or public awareness. However, it may also be due to a bias in the selection method employed in the study. All cases, whether newly identified (incident cases) or diagnosed previously (prevalent cases) appeared as new case entries for the first years of data collection, which may lead to cumulative high rates from 2000 to 2003 in HBsAg prevalence. Additionally, HBsAg detection in individuals younger than 10 years also displayed a statistically significant tendency to decrease during the study period, while it was constant for other age groups (Figure 3). This observation has important implications. First of all, this group is more likely to be directly influenced by the vaccination program and may provide further data for a reduction of HBV by vaccination in Turkish population. On the other hand, stable HBsAg seroprevalences among older age groups indicate horizontal rather than vertical route of transmission of HBV infection in our population. This observation confirmes the previous reports where the major HBV transmission route in Turkey was suggested to be horizontal, based on the data from blood donors and general public, which is also in line with other zones of intermediate HBV prevalence around the globe.7-9,20,21
The general public incidence of HBsAg positivity in Turkey has ranged between 1.7-21.0%, depending on the screened region.7,8 According to studies conducted by several blood banks, HBsAg positivity amongst blood donors was 5.2% during the period between 1985 and 1999, which then decreased to 2.97% between 2000 and 2003.8 During the study period (2000-2010) we have observed an overall HBs seroprevalence of 5.96%. It should be noted that the study was performed at a university hospital and a referral centre, so that infection rates may be higher compared to general public or blood donors. This trend has already been identified during comparison of various centres in Turkey.7,8 In consistence with the previous reports, adult males were observed to be more frequently infected with HBV with an HBsAg seroprevalence of 7.3% (4.5% in adult women).7,8,21 HBV DNA detection was significantly more frequent in HBsAg positive individuals with a rate of 25.6%, compared to HBsAg negatives.
The frequences of anti-HBe and HBeAg positive infections were 77.1% (5,595/7,254) and 18.5% (1,339/7,254), among HBsAg reactive individuals, respectively. A notable elevation in the number of anti-HBe positive infections with a parallel reduction in HBeAg positive infections were observed in yearly incidences from 2000 to 2003 (Figure 4). However, it remains to be determined if this is a real trend associated with factors such as better clinical follow-up and anti-viral drug therapy or represents the bias in the initial years of data collection, as discussed above. As previously noted for HBsAg, a male dominance was also observed in HBeAg positive individuals, suggesting that persistant HBV infections are more frequent in males in the study population. The age distribution of HBeAg or anti-HBe positive individuals were observed to be stable throughout the study period. The seroconversion phase detected by concomitantly positive anti-HBe and HBeAg were present in 0.56% (40/7,254) of the HBsAg reactive individuals.
It is known that during the natural history of HBV infections, HBeAg positive stage represents early phase of infection with higher levels of virus activity (elevated hepatic enzymes and HBV DNA) than anti-HBe positive stage.2,3 The comparison of HBeAg and anti-HBe positive individuals demonstrated that the mean AST, ALT, ALP and HBV DNA levels were higher and the number of individuals with high AST or ALT levels (exceeding 40 IU mL-1) were more frequent in HBeAg infections, thus confirming the aforementioned trend. Furthermore, elevated ALT levels were noted in 17.1% of the Anti-HBs + Anti-HBc reactive individuals, demonstrating the rate of ongoing viral replication in persons with reactive markers for virus exposure. In addition to the previously noted male predominance in infected individuals, HBeAg reactive cases were significantly younger than anti-HBe positive individuals with mean age of 20.3 vs. 40.4 years. The rates of HBV detection were similar in HBeAg and anti-HBe antibody reactive persons and significantly more frequent in individuals with HBeAg or anti-HBe reactivity compared to seronegative persons. Taken together, the results of this study confirmed the changes in HBV infection dynamics observed in previous studies from various cohorts, which indirectly confirm the validity of our data collection and interpretation methods applied.
In conclusion, the changes of epidemiologic trends of HBV infection after millennium were evaluated by retrospective analysis of 11 years, HBV tests results at a major referral hospital in Turkey. The data confirmed the intermediate prevalence of HBV infection, a male predominance in infected individuals and implied mainly horizontal route of virus transmission in Turkish population. The recognition of established HBV dynamics and patterns in persistently infected individuals is the evidence for reliability of method used and data obtained at this study. The reduction of childhood HBV infections can be attributable to the effectiveness of ongoing nationwide vaccination program.
Abbreviations- •
HBV: hepatitis B virus.
- •
HBsAg: hepatitis B surface antigen.
- •
HBeAg: hepatitis B e antigen.
- •
Anti-HBs: antibodies against hepatitis B surface antigen.
- •
Anti-HBe: antibodies against hepatitis B e antigen.
- •
Anti-HBc: antibodies against hepatitis B core antigen.
- •
AST: aspartate aminotransferase.
- •
ALT: alanine aminotransferase.
- •
GGT: gama-glutamyl transpeptidase.
- •
AP: alkaline phosphatase.
The authors declare that no competing interests exist. No funding or support was received for the completion of the study. The preliminary results have been presented as a poster (P003, ref. no. 59) in the 8th National Congress for Hepatology during June 1st-5th, 2011 in Ankara, Turkey.