Non-alcoholic fatty liver disease (NAFLD) is the most common liver disorder in western countries. It is often related to metabolic syndrome, presenting an increased risk of advanced liver disease and cardiovascular-related death. In some etiologies of chronic liver disease, thrombocytopenia has been associated not only with advanced stages of fibrosis but also with autoimmune disease. In NAFLD, however, its prevalence and related factors are still unknown. The aim of this study is to evaluate the prevalence of thrombocytopenia in NAFLD patients without cirrhosis and to investigate its related risk factors.
Patients and methodsThis was a retrospective study carried out in two tertiary hospitals in the South and Southeast regions of Brazil. Patients diagnosed with NAFLD by liver biopsy were included. Those with other causes of liver disease and/or cirrhosis were excluded. For analysis, patients were divided into two groups, with and without thrombocytopenia. Data was analyzed using a significance level of 5%.
Results441 non-cirrhotic patients with NAFLD (evaluated by liver biopsy) were included in the study. The prevalence of thrombocytopenia was 3.2% (14/441 patients). In the comparative analysis between groups, thrombocytopenia was associated with male sex (p=0.007) and level of hemoglobin (p=0.023).
ConclusionThrombocytopenia is an infrequent event in NAFLD patients without cirrhosis and is related with male sex and higher hemoglobin levels.
Non-alcoholic fatty liver disease (NAFLD) is currently the most common liver disorder in western countries, affecting 17–46% of adults [1,2]. It ranges from simple steatosis and steatohepatitis to liver cirrhosis and its complications, such as hepatocellular carcinoma [1–4]. NAFLD is often associated with metabolic syndrome and its components, with an increased risk of advanced liver disease and cardiovascular-related death [1,2].
In high-risk groups, the prevalence of NAFLD is higher. In morbid obesity candidates for bariatric surgery, it may reach 90% of patients, 69% in type 2 diabetics and 50% in dyslipidemic patients [2,3]. In our setting, amongst 250 morbidly obese patients undergoing bariatric surgery, the prevalence of NAFLD was 90% [5]. It is also important to emphasize that it may be present in non-obese individuals (7%) [1].
The diagnosis of NAFLD is of exclusion, in which it is necessary to rule out secondary causes of liver disease, significant consumption of alcohol and drugs that may cause steatosis. In addition, the definitive diagnosis of steatohepatitis still requires a liver biopsy [1]. Considering that liver biopsy is an invasive procedure that involves risks of sample errors, non-invasive markers and imaging have also been considered as diagnostic methods [2].
In hepatitis C virus chronic liver disease, thrombocytopenia has been related to the infection of platelets by HCV or to advanced stage of fibrosis. Low platelets count has been described in some NAFLD patients without cirrhosis, but its prevalence and related factors are unknown [4,6,7].
The objective of the present study is to evaluate the prevalence and associated factors of thrombocytopenia in a cohort of patients with NAFLD without cirrhosis submitted to liver biopsy.
2Materials and methodsThis was a retrospective study, conducted in the Gastroenterology/Hepatology Outpatient Clinic of Santa Casa de Misericordia, Porto Alegre, and in the Hepatology Outpatients Clinic at Clementino Fraga Filho University Hospital in Federal University of Rio de Janeiro, two leading tertiary hospitals in Brazil. A convenience sample including all patients presenting evidence of NAFLD by liver biopsy from January 2016 to January 2018 was investigated.
Inclusion criteria was being at least 18 years old and having NAFLD documented by liver biopsy. Patients who had platelet count performed close to the liver biopsy (at maximum 3 months) were included. Cirrhotic patients, those without histological documentation of NAFLD, those with another cause of hepatic disease (hepatitis B or C virus, cholestatic diseases, autoimmune disease, amongst others), alcohol abuse (>20g alcohol/day) and drugs that could potentially cause steatosis or thrombocytopenia were excluded.
Initially, 493 patients were included. Six (1.2%) were later excluded, due to an inadequate evaluation of the fibrosis stage, 27 (5.5%) due to the absence of steatosis and 19 (3.8%) due to cirrhosis.
Patients were then divided into two groups: NAFLD with normal platelets (above 150,000/μL) and NAFLD with thrombocytopenia in at least two consecutive determinations.
Age, sex, comorbidities (systemic arterial hypertension, diabetes mellitus type 2 [DM2]), body mass index [BMI], degree of steatosis and fibrosis in histology, aminotransferases (alanine aminotransferases – ALT and aspartate aminotransferases – AST), total bilirubin (TB), albumin, hemoglobin, glucose, insulin for calculating the homeostasis model assessment-estimated insulin resistance (HOMA-IR) [8], lipid profile, ferritin and C-reactive protein (CRP) were evaluated.
The study was submitted and approved by the local Ethics Committee. For statistical analysis, the Chi-square test was used to verify if there was any association between categorical variables (and, when necessary, Fisher's exact test). Student's t-test was performed for independent variables. The Mann Whitney test was used to compare medians for variables that were not normally distributed (also performed by Kolmogorov–Smirnov test). SPSS 23.0 software was used, and the significance level adopted was 5%.
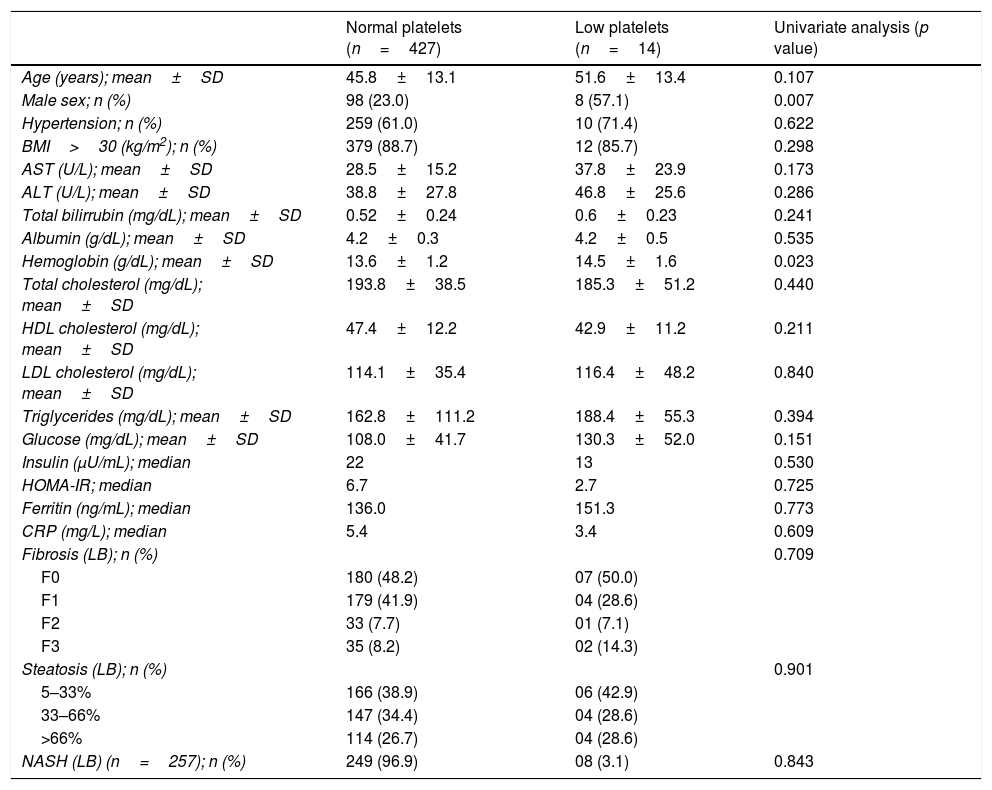
3ResultsA total of 441 patients were included in the study. The prevalence of thrombocytopenia was 3.2% (14/441 patients). The patient's demographic characteristics as well as the presence of comorbidities, laboratory tests and histological evaluation are described in Table 1. When the two-groups with and without thrombocytopenia were compared, it was observed that the group with thrombocytopenia had a higher proportion of male gender (p=0.007) and higher hemoglobin levels (p=0.023) in the univariate analysis. Furthermore, each additional unit of hemoglobin increases by 1.5 the chance of having thrombocytopenia [RP=1.5; 95% CI (1.09–2.09); p=0.01].
Demographic characteristics (n=441).
| Normal platelets (n=427) | Low platelets (n=14) | Univariate analysis (p value) | |
|---|---|---|---|
| Age (years); mean±SD | 45.8±13.1 | 51.6±13.4 | 0.107 |
| Male sex; n (%) | 98 (23.0) | 8 (57.1) | 0.007 |
| Hypertension; n (%) | 259 (61.0) | 10 (71.4) | 0.622 |
| BMI>30 (kg/m2); n (%) | 379 (88.7) | 12 (85.7) | 0.298 |
| AST (U/L); mean±SD | 28.5±15.2 | 37.8±23.9 | 0.173 |
| ALT (U/L); mean±SD | 38.8±27.8 | 46.8±25.6 | 0.286 |
| Total bilirrubin (mg/dL); mean±SD | 0.52±0.24 | 0.6±0.23 | 0.241 |
| Albumin (g/dL); mean±SD | 4.2±0.3 | 4.2±0.5 | 0.535 |
| Hemoglobin (g/dL); mean±SD | 13.6±1.2 | 14.5±1.6 | 0.023 |
| Total cholesterol (mg/dL); mean±SD | 193.8±38.5 | 185.3±51.2 | 0.440 |
| HDL cholesterol (mg/dL); mean±SD | 47.4±12.2 | 42.9±11.2 | 0.211 |
| LDL cholesterol (mg/dL); mean±SD | 114.1±35.4 | 116.4±48.2 | 0.840 |
| Triglycerides (mg/dL); mean±SD | 162.8±111.2 | 188.4±55.3 | 0.394 |
| Glucose (mg/dL); mean±SD | 108.0±41.7 | 130.3±52.0 | 0.151 |
| Insulin (μU/mL); median | 22 | 13 | 0.530 |
| HOMA-IR; median | 6.7 | 2.7 | 0.725 |
| Ferritin (ng/mL); median | 136.0 | 151.3 | 0.773 |
| CRP (mg/L); median | 5.4 | 3.4 | 0.609 |
| Fibrosis (LB); n (%) | 0.709 | ||
| F0 | 180 (48.2) | 07 (50.0) | |
| F1 | 179 (41.9) | 04 (28.6) | |
| F2 | 33 (7.7) | 01 (7.1) | |
| F3 | 35 (8.2) | 02 (14.3) | |
| Steatosis (LB); n (%) | 0.901 | ||
| 5–33% | 166 (38.9) | 06 (42.9) | |
| 33–66% | 147 (34.4) | 04 (28.6) | |
| >66% | 114 (26.7) | 04 (28.6) | |
| NASH (LB) (n=257); n (%) | 249 (96.9) | 08 (3.1) | 0.843 |
DM2, diabetes mellitus type 2; BMI, body mass index; ALT, alanine aminotransferase; AST, aspartate aminotransferase; IR, insulin resistance; CRP, C-reactive protein; LB, liver biopsy; NASH, nonalcoholic steatohepatitis.
NAFLD comprises a wide spectrum of clinical conditions, currently representing an emerging disease of great clinical interest. It is the hepatic expression of the metabolic syndrome and its prevalence has been growing worldwide [4].
There are few studies in the literature that approaches the association of thrombocytopenia and NAFLD in patients without cirrhosis [6,7,9,10], and in all of these studies, the patients were evaluated by non-invasive methods. As far as we are concerned, this is the first study to evaluate the association of thrombocytopenia in patients without cirrhosis, with histological diagnosis of NAFLD.
In the present study, the prevalence of thrombocytopenia was 3.2% and an inverse association between male sex, hemoglobin and thrombocytopenia in individuals with NAFLD without cirrhosis was demonstrated.
Although thrombocytopenia represents a marked feature of end stage liver disease, its prevalence, features and significance in NAFLD is not very clear. The causes are unknown, but a possible explanation for the occurrence of thrombocytopenia in NAFLD patients is the inadequate thrombopoietin production by the liver [4], considering that thrombopoietin is implicated in the platelet production and is highly dependent on the functional liver cells. Some authors have suggested that the function and the morphology of platelets are altered in patients with diabetes mellitus and metabolic syndrome and thus low platelets could, in the scenario of NAFLD, act as an indirect marker of extra hepatic metabolic disease [9,11–13]. Another suggestion is that in NAFLD, fibrosis begins around the central veins; therefore, the manifestations of portal hypertension may appear first as a result of central vein occlusion [14]. These hypotheses were not evaluated in the present study, but have been postulated in the scenario of low platelets in patients with NAFLD without cirrhosis. Thus, many of our patients presented diabetes mellitus and metabolic syndrome, and presented some degree of fibrosis that could justify the findings.
Regarding thrombocytopenia some considerations could still be made. Thus, Yoneda et al. [15] investigated the platelet count as a predictive factor of the severity of liver fibrosis in 1048 patients with liver biopsy proven NAFLD (including patients with cirrhosis) and found a significant difference in the platelet count depending on the fibrosis degree. The authors suggest that NAFLD patients with platelet counts of less than 19.2×109/L should be closely followed up, because they could progress to NAFLD with severe fibrosis.
Dasanu et al. [10] analyzed a series of 18 patients with metabolic syndrome and thrombocytopenia without cirrhosis (evaluated by ultrasonography) and found that persistent thrombocytopenia, even mild or moderate, can be a potentially useful marker for NAFLD in patients with metabolic syndrome, although this could be a controversial hypothesis.
Also Alempijevic et al. [16] found an inverse correlation between platelet count and liver fibrosis in patients with NAFLD (evaluated by a non-invasive method).
In the study by Olivares-Gazca et al. [6], 8/33 (24%) patients with NAFLD without cirrhosis (evaluated by transient hepatic elastography – Fibroscan) presented thrombocytopenia, which was associated with weight gain. Thrombocytopenia was usually mild, presented no association with bleeding and no need for specific treatment.
As previously stated, in the present study, the prevalence of thrombocytopenia was 3.2%, which was lower than in the study of Olivares-Gazca et al. [6].
The differences between the results of the studies can possibly be explained by the fact that these studies used different inclusion criteria, various etiologies and degrees of liver disease, small number of evaluated patients and/or differences in laboratory techniques [17]. Some studies evaluated the diagnostic accuracy of platelet count in the assessment of fibrosis in NAFLD patients, but in these studies, patients were not submitted to liver biopsy [7,11–13,16], which is still the gold standard for the diagnosis of NAFLD, nor excluded patients with cirrhosis [7,12,17].
The high level of serum hemoglobin has recently been associated with NAFLD and NASH [18,19], suggesting that hematological parameters may be introduced in algorithms for predicting NASH risk and that hemoglobin could emerge as a serum marker for an early and accurate NAFLD detection. Also, it his been previously demonstrated that the oxidative stress upregulates the hemoglobin expression in NASH [20]. However, no study had ever evaluated the association between hemoglobin and thrombocytopenia before.
As potential limitations of the present study, we can highlight being developed in tertiary hospitals, being a retrospective study and also having a small number of patients with thrombocytopenia evaluated. However, the other studies that analyzed this finding also presented smaller casuistic, emphasizing the need of more studies in this field. On the other hand, the present study has the advantage of having evaluated all the patients through liver biopsy.
In conclusion, thrombocytopenia is an infrequent event in NAFLD patients without cirrhosis and is related to male gender and higher hemoglobin. Further prospective studies, with a specific methodological design, are necessary to confirm the results of this study.
Authors’ contributionsCristiane V. Tovo conceptualized the study. Carine L. Panke, Cristiane A. Vilella-Noqueira, Claudia Claudia M. Cravo, Frederico C. Ferreira, Guilherme F.M. Rezende, Fernanda L. Calçado, Ana C.C. Figueiredo-Mendes, Nathalie C. Leite and Gabriela P. Coral collected the data. Carine L. Panke, Cristiane V. Tovo, Cristiane A. Villela-Nogueira and Nathalie C. Leite analyzed the data. Carine L. Panke, Cristiane V. Tovo, Cristiane A. Villela-Nogueira, Nathalie C. Leite and Angelo A. de Mattos wrote the manuscript. All the authors revised and approved the final version.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors have no conflicts of interest to declare.