Introduction: We sought to describe: 1) The influence of orthotopic liver transplantation (OLT) on exercise capacity, pulmonary function and respiratory muscle strength after surgery, 2) The relationship between exercise capacity and symptoms of anxiety and depression.
Material and methods. This is a prospective follow up study conducted with patients submitted to OLT. All patients were assessed before and 1 month after surgery through measurements: six minute walk test (6MWT), 6 min step test (6MST) and HADS (Hospital Anxiety and Depression Scale). FEV1% (forced expiratory volume), maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) were measured in the pre-operative and on 1st, 3rd, 5th day and 1 month after surgery.
Results. In 77 patients, 6MWD improved 20.2 m (95%CI 8.1-32.3) and 6MST improved 7.8 steps after surgery (95%CI 3.9-11.6). Change in 6 MWD and 6 MST did not correlated with change HADS. The FEV1% at each time point were 88.8 ± 21.3 before surgery, 32.9 ± 9.9 on 1st day, 39.6 ± 11.5 on 3rd day, 46 ± 12.1 on 5th day and 86.6 ± 21.1 one month after surgery. MIP and MEP values at each time point were -67.4 ± 23.2 and 79.7 ± 26 before surgery, −30.8 ± 12.3 and 36.4 ± 15.4 on 1st day, −38.6 ± 14.1 and 43.8 ± 17 on 3rd day, −45.8 ± 15.9 and 49.7 ± 18.7 on 5th day and −67.1 ± 29.4 and 80.9 ± 23.9 one month after surgery.
Conclusion. Exercise capacity was modestly increased after OLT without any correlation with symptoms of anxiety and depression. Pulmonary function and respiratory muscle strength decreased immediately after liver transplantation, and progressively recovered, returning to baseline values after 1 month.
In end stage liver disease (ESLD), functional capacity becomes progressively impaired.1,2 Measurement of exercise capacity is an important element to assess patients after surgery. Although the 6-min walk test (6-MWT) provides useful information regarding functional capacity, response to therapy, and prognosis across a range of conditions, its applicability for orthotopic liver transplantation (OLT) remains to be established.3
The six-min walk test (6MWT) and the 6-min step test (6MST) are simple and low-cost tests to measure exercise capacity. The 6MST has been used to assess exercise capacity in patients with chronic obstructive lung disease and interstitial lung disease,4,5 but to the best of our knowledge, has not been previously evaluated in ESLD subjects.
Liver transplantation is an upper abdominal surgery that leads to changes in pulmonary function and respiratory mechanics, including decreased diaphragm mobility that may result in a reduction in lung volumes and airflow limitation.6–7
One of the main characteristics of ESLD patients is muscle mass loss which may affect both peripheral and respiratory muscles. These patients also are characterized by chronic fatigue and protein wasting.8 According to van den Berg-Emons, et al.9 muscle fatigue may continue for up to one year after liver transplantation.
Anxiety and depression are more present in patients with ESLD and they would improve after transplantation.10 The relationship between changes in anxiety and depression with changes in measurements of exercise capacity (6MWT and 6 MST) after liver transplantation has not been studied.
Evaluation of fitness among ESLD patients is relevant because it can potentially be improved by exercise training and may be a modifiable factor to improve the outcomes of patients after liver transplant.
Material and MethodsThis prospective study was conducted at a teaching hospital in Fortaleza, Brazil. The initial cohort consisted of 100 consecutive patients who underwent orthotopic liver transplantation (OLT), from March 2013 to March 2015. Twenty three patients were later excluded either because they declined to perform the tests, or had neurological (moderate to severe hepatic encephalopathy), vascular or musculoskeletal conditions limiting their ability to perform the functional tests therefore the final sample consisted of seventy seven consecutive patients.
All patients listed for LT with priority for graft allocation performed the functional tests, on average, 7 days before surgery. In all cases, demographic and clinical characteristics, including sex, age, comorbidities, history of pulmonary or liver disease, Child-Pugh classification, model for end-stage liver disease score (MELD), were assessed at this period. All subjects included in the study gave their written informed consent prior to enrollment and the study was previously approved by the institutional review board of Federal University of Ceará (protocol No. 052.07.12).
OutcomesThe primary outcomes was exercise capacity, measured by the six minute walking distance (6MWD) and the number of steps climbed during the 6 minute step test (6MST). The secondary outcomes were: maximal inspiratory mouth pressure (MIP) and maximal expiratory mouth pressure (MEP), forced expiratory volume in one second (FEV1) and symptoms of anxiety and depression, measured by the Hospital Anxiety and Depression Scale (HADS).
Data collectionIn all cases, demographic and clinical characteristics, including sex, age, comorbidities, history of pulmonary or liver disease, Child-Pugh classification, model for end-stage liver disease score (MELD), were assessed at baseline.
Exercise capacitySix-minute walking distance (6MWD) and the 6-minute step test (6MST) were performed concomitantly before surgery. Patients with ascite and functional capacity impairment were drained and after that the tests were performed.
All patients were followed after LT and received standard respiratory therapy sessions (breathing exercises and ambulation) daily until hospital discharge. After that, the patients came home and returned 1 month later for new functional evaluation.
To measure the 6MWD, patients were instructed to walk over a 30 m corridor from end to end as far as they could, during 6 min.11 The 6MST consists of a self-paced test performed on a step (20 cm high with non-slip rubber surface), and the patients were instructed to climb the greatest number of steps during six minutes. The more steps a patient climbs, the better the exercise capacity.12
Respiratory function and respiratory muscle strength measurementsPulmonary function was assessed by spirometry which was performed according to international guidelines.13 Results were compared to reference values for the Brazilian population.14 Respiratory muscle strength was assessed by maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) which measure the highest proximal airway pressure reached during inspiration and expiration, respectively.15 Forced expiratory volume in one second (FEV1), MEP and MIP were measured, on average, 7 days before surgery and also on the first, third, fifth and 30th post-operative days. All 77 patients were off ventilator and extubated since the 1st post-operative after OLTx.
Anxiety and depressionLevels of anxiety and depression were determined before and 1 month after surgery by the Portuguese version of Hospital Anxiety and Depression Scale (HADS).16 This is a fourteen item scale, seven of the items relate to anxiety and seven relate to depression.17 All the tests were conducted by the same trained pulmonologist technician who was not aware of the research protocol.
Statistical methodsData analysis was performed using the Statistical Package for the Social Sciences (SPSS) 19.0. Kolmogorov-Smirnov test was used to test for normality. Data are presented as absolute and/or relative frequency, mean ± standard deviation for normally distributed data or median (interquartile interval) for non-normal data. The time course of the effect of liver transplantation on measurements of respiratory function, respiratory muscle strength, exercise capacity, anxiety and depression was investigated by repeated measures ANOVA. Additionally, pairwise comparisons (ANOVA) of respiratory function and respiratory muscle strength before surgery and after the first, third, fifth day and 1 month after liver transplantation were performed. Differences were considered to be significant at P < 0.05. Correlations between change in exercise capacity with other measures of the patients were calculated using Pearson correlations.
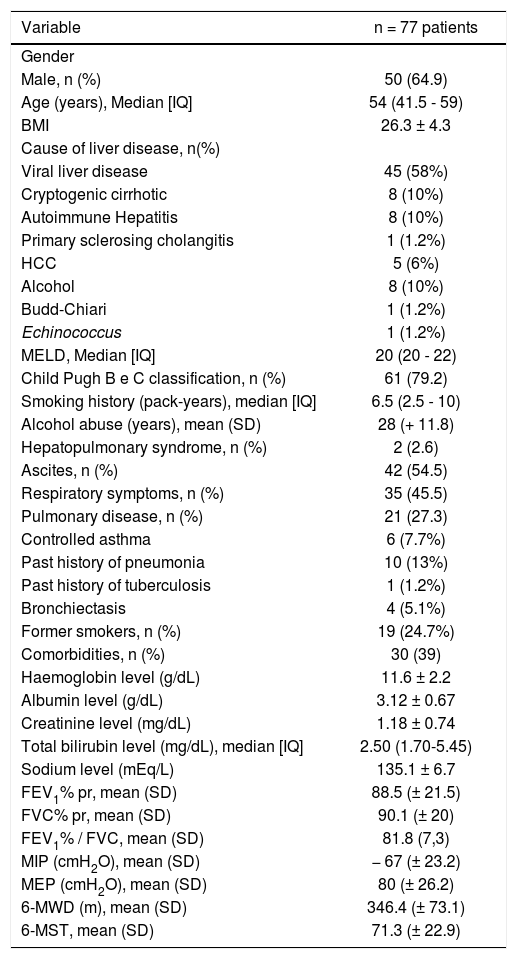
ResultsThe cohort of 77 patients was predominantly male (64.9%). The median age was 54 years (interquartile range: 41.5 - 59). The mean of 6MWD and 6MST values were 346.4 ± 73.1 m and 71.3 ± 22.9 steps, respectively, before surgery (Table 1). In the post-operative the hospital stay lasted from 8 to 14 days (median 10 days).
Socio-demographic, clinical and laboratory characteristics of 77 patients submitted to liver transplantation.
| Variable | n = 77 patients |
|---|---|
| Gender | |
| Male, n (%) | 50 (64.9) |
| Age (years), Median [IQ] | 54 (41.5 - 59) |
| BMI | 26.3 ± 4.3 |
| Cause of liver disease, n(%) | |
| Viral liver disease | 45 (58%) |
| Cryptogenic cirrhotic | 8 (10%) |
| Autoimmune Hepatitis | 8 (10%) |
| Primary sclerosing cholangitis | 1 (1.2%) |
| HCC | 5 (6%) |
| Alcohol | 8 (10%) |
| Budd-Chiari | 1 (1.2%) |
| Echinococcus | 1 (1.2%) |
| MELD, Median [IQ] | 20 (20 - 22) |
| Child Pugh B e C classification, n (%) | 61 (79.2) |
| Smoking history (pack-years), median [IQ] | 6.5 (2.5 - 10) |
| Alcohol abuse (years), mean (SD) | 28 (+ 11.8) |
| Hepatopulmonary syndrome, n (%) | 2 (2.6) |
| Ascites, n (%) | 42 (54.5) |
| Respiratory symptoms, n (%) | 35 (45.5) |
| Pulmonary disease, n (%) | 21 (27.3) |
| Controlled asthma | 6 (7.7%) |
| Past history of pneumonia | 10 (13%) |
| Past history of tuberculosis | 1 (1.2%) |
| Bronchiectasis | 4 (5.1%) |
| Former smokers, n (%) | 19 (24.7%) |
| Comorbidities, n (%) | 30 (39) |
| Haemoglobin level (g/dL) | 11.6 ± 2.2 |
| Albumin level (g/dL) | 3.12 ± 0.67 |
| Creatinine level (mg/dL) | 1.18 ± 0.74 |
| Total bilirubin level (mg/dL), median [IQ] | 2.50 (1.70-5.45) |
| Sodium level (mEq/L) | 135.1 ± 6.7 |
| FEV1% pr, mean (SD) | 88.5 (± 21.5) |
| FVC% pr, mean (SD) | 90.1 (± 20) |
| FEV1% / FVC, mean (SD) | 81.8 (7,3) |
| MIP (cmH2O), mean (SD) | − 67 (± 23.2) |
| MEP (cmH2O), mean (SD) | 80 (± 26.2) |
| 6-MWD (m), mean (SD) | 346.4 (± 73.1) |
| 6-MST, mean (SD) | 71.3 (± 22.9) |
I: InterQuartil Range. MELD: Model for End-Stage Liver Disease. FEV1 %pr: percent predicted Forced Expiratory Volume in one second; FVC % pr: percent predicted Forced Vital Capacity. 6-MWD: 6-Minute Walking Distance. 6-MST: 6-Minute Step Test. MIP: Maximal Inspiratory Pressure. MEP: Maximal Expiratory Pressure. HCC: hepatocellular carcinoma. BMI: body mass index.
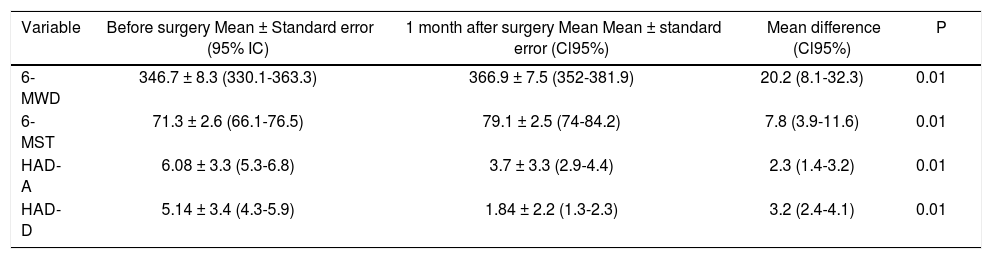
Improvement in exercise capacity and symptoms of anxiety and depression 1 month after surgery, as compared to baseline, are shown in table 2.
Effects of liver transplantation on exercise capacity and symptoms of anxiety and depression in 77 patients.
| Variable | Before surgery Mean ± Standard error (95% IC) | 1 month after surgery Mean Mean ± standard error (Cl95%) | Mean difference (Cl95%) | P |
|---|---|---|---|---|
| 6-MWD | 346.7 ± 8.3 (330.1-363.3) | 366.9 ± 7.5 (352-381.9) | 20.2 (8.1-32.3) | 0.01 |
| 6-MST | 71.3 ± 2.6 (66.1-76.5) | 79.1 ± 2.5 (74-84.2) | 7.8 (3.9-11.6) | 0.01 |
| HAD-A | 6.08 ± 3.3 (5.3-6.8) | 3.7 ± 3.3 (2.9-4.4) | 2.3 (1.4-3.2) | 0.01 |
| HAD-D | 5.14 ± 3.4 (4.3-5.9) | 1.84 ± 2.2 (1.3-2.3) | 3.2 (2.4-4.1) | 0.01 |
6-MWD: 6-minute walking distance. 6-MST= 6-minute step test. HAD-D: Hospital anxiety and depression scale-depression. HAD-A: Hospital anxiety and depression scale-anxiety.
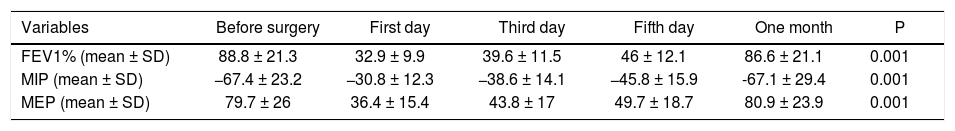
A significant decrease in percent predicted FEV1, MIP and MEP was observed in the immediate post-transplant period among the 77 patients. A progressive recovery of those parameters, confirmed by longitudinal analysis (repeated measures ANOVA) was observed and after 1 month they returned to baseline, as shown in table 3.
Repeated Measures Analysis of Variance (ANOVA) of respiratory parameters at different observation periods in 77 patients submitted to liver transplantation.
| Variables | Before surgery | First day | Third day | Fifth day | One month | P |
|---|---|---|---|---|---|---|
| FEV1% (mean ± SD) | 88.8 ± 21.3 | 32.9 ± 9.9 | 39.6 ± 11.5 | 46 ± 12.1 | 86.6 ± 21.1 | 0.001 |
| MIP (mean ± SD) | −67.4 ± 23.2 | −30.8 ± 12.3 | −38.6 ± 14.1 | −45.8 ± 15.9 | -67.1 ± 29.4 | 0.001 |
| MEP (mean ± SD) | 79.7 ± 26 | 36.4 ± 15.4 | 43.8 ± 17 | 49.7 ± 18.7 | 80.9 ± 23.9 | 0.001 |
FEV1: Forced Expiratory Volume in one second. MIP: Maximal inspiratory pressure. MEP: Maximal expiratory pressure.
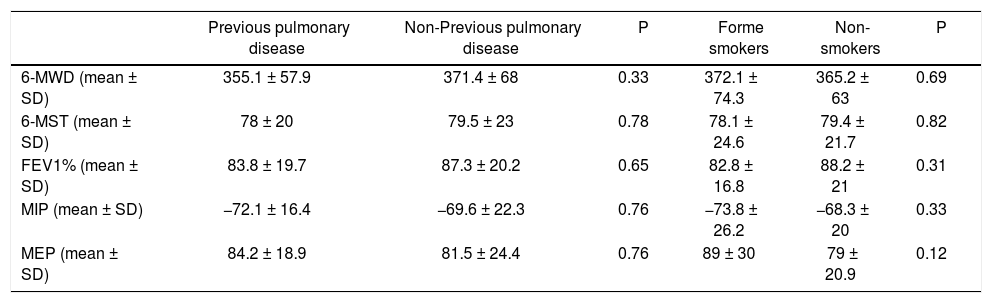
Table 4 shows the results of the comparisons of exercise capacity and respiratory profile 1 month after transplantation between different subgroups of patients. Patients with previous pulmonary disease and former smokers presented similar levels of exercise and respiratory parameters compared with their counterparts.
Results of comparisons of exercise and respiratory parameters 1 month after transplantation among different subgroups of patients.
| Previous pulmonary disease | Non-Previous pulmonary disease | P | Forme smokers | Non-smokers | P | |
|---|---|---|---|---|---|---|
| 6-MWD (mean ± SD) | 355.1 ± 57.9 | 371.4 ± 68 | 0.33 | 372.1 ± 74.3 | 365.2 ± 63 | 0.69 |
| 6-MST (mean ± SD) | 78 ± 20 | 79.5 ± 23 | 0.78 | 78.1 ± 24.6 | 79.4 ± 21.7 | 0.82 |
| FEV1% (mean ± SD) | 83.8 ± 19.7 | 87.3 ± 20.2 | 0.65 | 82.8 ± 16.8 | 88.2 ± 21 | 0.31 |
| MIP (mean ± SD) | −72.1 ± 16.4 | −69.6 ± 22.3 | 0.76 | −73.8 ± 26.2 | −68.3 ± 20 | 0.33 |
| MEP (mean ± SD) | 84.2 ± 18.9 | 81.5 ± 24.4 | 0.76 | 89 ± 30 | 79 ± 20.9 | 0.12 |
6-MWD: 6-minute walking distance. 6-MST: 6-minute step. FEV1: Forced Expiratory Volume in one second. MIP: Maximal inspiratory pressure. MEP: Maximal expiratory pressure.
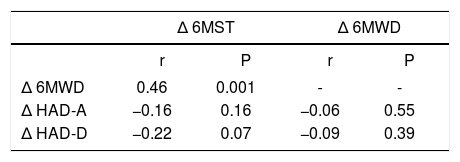
Table 5 shows that the changes in 6 MWD and 6 MST did not correlated with change in HAD scale.
Univariate correlates of change in 6 MWD and 6 MST.
| Δ 6MST | Δ 6MWD | |||
|---|---|---|---|---|
| r | P | r | P | |
| Δ 6MWD | 0.46 | 0.001 | - | - |
| Δ HAD-A | −0.16 | 0.16 | −0.06 | 0.55 |
| Δ HAD-D | −0.22 | 0.07 | −0.09 | 0.39 |
6MWD: 6-minute walking distance. 6MST: 6-minute step test. HAD-D: Hospital Anxiety and Depression Scale-depression. HAD-A: Hospital Anxiety and Depression Scale-anxiety.
In the present study, it was observed that exercise capacity and anxiety and depression improved 1 month after liver transplantation. Change in exercise capacity did not correlated with change in symptoms of anxiety and depression. Pulmonary function and respiratory muscle strength decreased immediately after liver transplantation, after that there was a progressive recovery and after 1 month they returned to the baseline.
It has been previously reported that patients with cirrhosis have significantly poorer 6MWT results than individuals with stable chronic viral hepatitis and healthy volunteers.1 In our sample the mean preoperative 6MWT and 6 MST were 346.4 ± 73.1 meters and 71.3 ± 22.9 steps, respectively. These are significantly reduced in comparison with reference values in healthy Brazilian adults (P < 0.0001).18,19 This could be explained by the fact that these patients usually suffer from fatigue, severe muscle wasting, malnutrition and weakness.20,21 Sarcopenia is part of the frailty complex present in cirrhotic patients, resulting in impaired functional capacity, decreased reserve, negative response to stressor and predisposition to pre-trans-plant mortality.22
After transplantation both 6MWT and 6 MST improved, a possible justification for the increase may be due to the learning factor. But even that, the tests remained below reference values, suggesting a low level of fitness after 1 month of surgery. This may be explained by chronic fatigue following surgery, according to van den BergEmons, et al.23 muscle fatigue may continue for up to one year after liver transplantation. Furthermore, those investigators found that severe complaints of fatigue in liver transplant recipients are associated with low levels of everyday physical activity. VanWagner, et al.24 observed that the 6MWT performance in 62 patients with chronic liver disease improved post-LT but was lower than expected.
Step tests are widely employed to measure exercise capacity, and their use in the assessment of patients with chronic respiratory conditions is well established,4,5 however it has never been used in patients with ESLD. Change in 6MWT 1 month after surgery correlated with change in 6MST, this is remarkable and underscores the potential usefulness of 6MST to measure exercise capacity. in our cohort of patients with ESLD.
There are few data on changes in respiratory muscle strength after liver trasnplantation.9,21 Baseline values of MIP and MEP were significantly reduced in our sample, in comparison with reference values for healthy Brazilian adults (p < 0.001).25 This is in agreement with previous report by Galant, et al.26 A possible explanation for this reduced respiratory muscle strength could be the loss of muscle mass that may affect both peripheral and respiratory muscles in patients with ESLD.8
Immediately after surgery, there was a reduction in respiratory muscle strength, with a return to pre-operative levels after a one month period, although still remaining below reference values.25 It is known that surgical procedures in the upper abdominal area promote changes in pulmonary function and respiratory muscle strength in the first days after surgery, Paisani, et al.27 observed a decrease in MIP and MEP after gastroplasty on the first and third postoperative days. On the fifth postoperative day, the variables analyzed were higher than on the first day, indicating a linear increase, We observed a linear increase of respiratory muscle strengh in the presente study.
After liver transplantation, the removal of the liver results in a denervation and impaired diaphragm compliance, leading to changes in respiratory mechanics.28 In addition, fatigue can persist after surgery.9 Together, impairment of respiratory mechanics and fatigue, may be a possible explanation for the fact that the functional improvement observed in the step tests was not accompanied by improvements in lung capacities.
No significant differences were noted in exercise and respiratory parameters 1 month after transplantation among patients with a history of smoking or lung disease. One of the reason could be explained by the fact that patients were not heavy smokers and presented mild lung disease (Table 1).
Symptoms of anxiety and depression improved one month after surgery but did not show a significant correlation with improvement of exercise capacity. Previous studies have observed an association between anxiety and depression with impaired physical performance.29 The reasons why our study did not show this association could be our patients presented only mildly altered anxiety and depression scores and the improvement of exercise capacity was modest, thus lacking sufficient statistical power to address this issue adequately.
This study has potential limitations. First, it was conducted in only one center with a relatively small sample. The second limitation is one common to most of the follow-up analyses and concerns the dropped-out cases. Patients who were not included in the final analysis could have been those with the worst status. A third limitation is that the follow up period was too short. A longer follow up of at least 6 months post transplantation would likely show whether there is a relationship between physical capacity 1 month after surgery and longer term mortality.
In conclusion, after liver transplantation, there was a modest improvement in exercise capacity persisting 1 month after surgery. The use of simple tests to measure exercise capacity such as 6MWT and 6MST and tests to measure respiratory muscle strength such as MIP and MEP are important to assess the preoperative and 1 month postoperative level of fitness in liver transplantation candidates. These measurements should, in our view, be systematically used to provide patients with a reliable estimate of their fitness status and possibly plan an intervention (rehabilitation program).
Abbreviations- •
6 MST: 6 minute step test.
- •
6 MWD: six minute walking distance.
- •
6 MWT: six minute walk test.
- •
ESLD: end stage liver disease.
- •
FEV1%: Forced expiratory volume.
- •
HADS: Hospital Anxiety and Depression Scale.
- •
MELD: model for end-stage liver disease score.
- •
MEP: maximal expiratory pressure.
- •
MIP: maximal inspiratory pressure.
- •
OLT: orthotopic liver transplantation.
- •
SPSS: Statistical Package for the Social Sciences.