Viral hepatitis has been shown to be associated with various extrahepatic manifestations. These can be seen in both acute and chronic liver disease, may precede or follow overt liver disease. Aims and objects: To study the prevalence of extrahepatic manifestations of viral hepatitis and follow the course of the disease in response to antiviral therapy whenever indicated. Methods: Prospectively 448 patients of viral hepatitis were evaluated for extrahepatic manifestations and patients of glomerulonephritis (GN), polyarteritis nodosa (PAN) and cryoglobulinemia were tested for viral markers. All patients were investigated for liver and kidney function tests, hematological workup and viral markers such as HBsAg, HBeAg, Anti HBeAg, HCV RNA, IgM anti HAV and IgM anti HEV. Serum electrophoresis and kidney biopsies were done whenever indicated. In 10 cases of hepatitis B glomerulonephritis immunohistochemistry was done on kidney biopsies for demonstration of hepatitis B surface and core antigen. Results: Of total 448 cases 181 (40.4%) had hepatitis B infection, 142 (31.6%) had hepatitis C infection, 86 (19.1%) hepatitis E and 39 (8.7%) had hepatitis A infection. Extrahepatic manifestations were seen in 29 (6.4%) cases and these were cases of GN, PAN, cryoglobulinemia, thrombocytopenia, agranulocytosis, aplastic anemia and pancreatitis. Patients with hepatitis A with extrahepatic manifestations showed complete recovery in both hepatitis and extrahepatic manifestations. Six patients with PAN were treated with interferon of which 4 showed excellent response. Three patients of hepatitis B and hepatitis C related GN were given interferon and 4/6 responded well to treatment. Conclusion: Prevalence of extrahepatic manifestations with viral hepatitis was found to be 6.4%. These manifestations recover completely with recovery from viral hepatitis.
BYL Nair Hospital, TN Medical College, Mumbai, India.
Financial assistance was given by Medical research society, Bombay Hospital for purchasing kits for immunohistochemistry for hepatitis B surface and core antigen.
IntroductionAcute and chronic viral hepatitis may be complicated by multiorgan involvement by immune complex deposition at various sites.1-3 The demonstration of circulating immune complexes in patients of viral hepatitis B or C allows us to speculate that they are responsible for extrahepatic manifestations. 4-6 Glomerulonephritis, mixed cryoglobulinemia, polyarteritis nodosa and polyneuritis are some of the established extrahepatic manifestations of hepatitis B or C virus infection.6 These may contribute at times to significant mortality and morbidity in persistent viral infection.
AimsTo study the prevalence of extrahepatic manifestations of viral hepatitis and follow the course of disease in response to antiviral therapy whenever indicated.
Material and methodsTotal 448 patients of viral hepatitis were included in study prospectively over the period of 3 years. The patients presenting with viral hepatitis were assessed for extrahepatic manifestations. Patients of glomerulonephritis, polyarteritis nodosa and cryoglobulinemia were tested for viral markers. All patients were investigated for liver function tests, viral markers such as HBsAg, HBeAg, Anti HBeAg, HCV RNA, IgM anti HAV and IgM anti HEV as indicated. Kidney function tests and hematological workup was carried out with biopsy whenever required. Serum electrophoresis was done in suspected cases of cryoglobulinemia.
Kidney biopsies were available in 10 cases of glomerulonephritis, which were associated with hepatitis B infection. In these cases, kidney tissue was processed routinely. Immunohistochemistry was carried out for demonstration of hepatitis B surface and core antigen (Dako Corp dilution 1:4000 & 1:2000 respectively). Patients of GN without hepatitis B infection were taken as negative control.
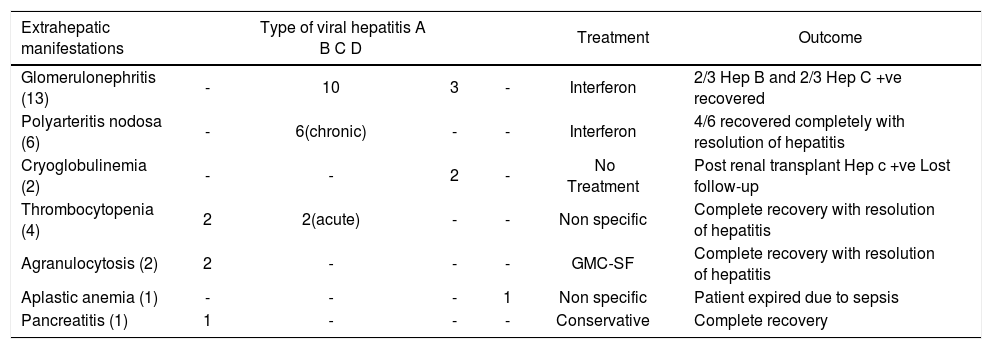
ResultsThe patients were between age group 4 to 62 years with the male: female ratio of 13:2. Hepatitis B infection (acute and chronic) was found in 181 (40.4%), hepatitis C (chronic) 142 (31.6%), hepatitis E 86 (19.1%), hepatitis A 39 (8.7%) cases (Table I). Extrahepatic manifestations were seen in 29 (6.4%) cases. These were cases of glomerulonephritis, PAN, cryoglobulinemia, thrombocytopenia, agranulocytosis, aplastic anemia and pancreatitis (Table II). Patients of hepatitis A with extrahepatic manifestations showed complete recovery. Six patients of PAN were treated with interferon of which 4 showed excellent response. Three each of hepatitis B and hepatitis C related GN were treated with interferon and 4 of then responded to treatment (Table III).
Profile of extrahepatic manifestations in viral hepatitis.
| N | Hep A | Hep B Acute | Hep B Chronic | Hep C Chronic | Hep E | |
|---|---|---|---|---|---|---|
| Glomerulonephritis | 13 | - | - | 10 | 3 | - |
| Polyarteritis nodosa | 6 | - | - | 6 | - | - |
| Cryoglobulinemia | 2 | - | - | - | 2 | - |
| Thrombocytopenia | 4 | 2 | 2 | - | - | - |
| Agranulocytosis | 2 | - | - | - | - | - |
| Aplastic anemia | 1 | - | - | - | - | 1 |
| Pancreatitis | 1 | 1 | - | - | - | - |
Outcome of extrahepatic manifestations.
| Extrahepatic manifestations | Type of viral hepatitis A B C D | Treatment | Outcome | |||
|---|---|---|---|---|---|---|
| Glomerulonephritis (13) | - | 10 | 3 | - | Interferon | 2/3 Hep B and 2/3 Hep C +ve recovered |
| Polyarteritis nodosa (6) | - | 6(chronic) | - | - | Interferon | 4/6 recovered completely with resolution of hepatitis |
| Cryoglobulinemia (2) | - | - | 2 | - | No Treatment | Post renal transplant Hep c +ve Lost follow-up |
| Thrombocytopenia (4) | 2 | 2(acute) | - | - | Non specific | Complete recovery with resolution of hepatitis |
| Agranulocytosis (2) | 2 | - | - | - | GMC-SF | Complete recovery with resolution of hepatitis |
| Aplastic anemia (1) | - | - | - | 1 | Non specific | Patient expired due to sepsis |
| Pancreatitis (1) | 1 | - | - | - | Conservative | Complete recovery |
Over a period of time, several extrahepatic manifestations of chronic HBV infection have been described and now few of them are well-established.6 As HCV serology testing improved in sensitivity and specificity, the existence and magnitude of extrahepatic associations with HCV were also clarified. Glomerulonephritis is one of those manifestations well documented in literature.7-9 The diagnosis of HBV associated GN is usually established by serologic evidence of HBV antigen or antibody, the presence on kidney biopsy of an immune complex GN and by demonstrating glomerular deposits containing one or more HBV related antigens (HBsAg, HBcAg or HBeAg) by immunohistochemical means.6 The incidence of HBV GN ranges from 0.1 to 25%.10-12 Brazosko et al were the first to suggest that HBV might be involved in the pathogenesis of high percentage of GN and found the incidence 34.6% with various types of glomerular diseases.13 Subsequently incidences reported were Lagrue14 et al (5.5%), Guardia15 et al (8.5%), Nagy16 et al (34.6%). In our study 13 patients presented with glomerulonephritis, of which 10 were HBV positive and 3 HCV positive patients. From 10 cases of HBV positive GN, 8 showed hepatitis B surface and core antigen on the basement membrane and mesengium of glomeruli.17 Liver histology in all of them were chronic hepatitis (active or persistent). Three patients each of hepatitis B and C received interferon therapy, of which 2 cases of hepatitis B and 2 of hepatitis C showed disappearance of proteinuria and recovery from hepatitis. Most of the patients of HBV associated GN who receive corticosteroids have either no beneficial effect or experience transient or incomplete remission. Hence most direct approach is to eliminate chronic viral infection by antiviral therapy. Evidence of reversibility of renal disease concomitant with spontaneous clearance of detectable HBsAg provides the rationale for interferon therapy. 6,18 Lisker-Melman M19 et al, evaluated 7 Caucasian adults with HBV related GN and the nephrotic syndrome. These patients were treated with interferon alpha, daily 5 194 Annals of Hepato million units for 4 months. In 5 of them serum markers of HBV replication disappeared with marked improvement in nephrotic syndrome. This report has been updated by Conjeevaran HS20 et al in 1995. A study from Taiwan have shown favorable treatment of HBV associated MGN in oriental children.21 In their study 40 patients with HBV-MGN were evaluated of which 20 were treated with interferon alpha remaining 20 received supportive therapy only. All those treated with interferon were free of proteinuria and 40% of them were seroconverted their HBeAg to antibody as against none seroconverted and only 50% had improvement in proteinuria from the second group receiving supportive therapy.
In 1970, generalized necrotizing vasculitis was first reported in association with hepatitis B antigenemia.22,23 Although the exact incidence of hepatitis B associated necrotizing vasculitis is not known; it ranges between 30 to 70 %.24,25 Sergent JS26 et al have reported 9 cases of PAN associated with hepatitis B infection and have shown that there is no difference in the prognosis as compared to PAN, not associated with HBV infection. We have come across 6 cases of PAN associated with hepatitis B infection. These cases were diagnosed on renal angiography and biopsy. All 6 cases were given interferon therapy. Four out of 6 patients showed recovery with resolution of hepatitis and disappearance of lesions on angiography. There is no relationship reported between severity of vasculitis and hepatic disease and liver disease is often quiescent. Treatment of PAN associated with HBV infection is limited in the literature; antiviral therapy may be of some use.27
A characteristic clinical syndrome of cryoglobulinemia has been described in hepatitis A, B and C infection.28-30 In general the overall prevalence of mixed cryoglobulinemia is as high as 40-50 % in chronic liver disease with the higher incidence in hepatitis C as compared to hepatitis B infection. 6,28,31 In our study there were only 2 cases of cryoglobulinemia, both were HCV-RNA positive. We could not offer any treatment because one patient acquired hepatitis C infection post renal transplant and in another there was no follow up available. Gorevic et al28 have followed up 40 patients of mixed cryoglobulinemia of which more than 60% showed serological evidence of hepatitis B infection. Reports on therapy of mixed cryoglobulinemia associated with hepatitis B infection are limited and more experience is necessary before the role of antiviral therapy for mixed cryoglobulinemia syndrome associated with chronic hepatitis B or C infection.
Hematological manifestations found in our study were 4 cases of thrombocytopenia, 2 agranulocytosis and a case of aplastic anemia. These 7 cases presented first with liver disease and then developed hematological manifestations subsequently. All of them were found to be patients of acute viral hepatitis either A, B or E. Leucopoenia and thrombocytopenia are commonly found in patients with chronic liver disease or cirrhosis.32 This is largely due to hypersplenism but their presence in acute viral hepatitis may be due to its extrahepatic manifestations. Subsequently bone marrow failure results from immunologically mediated, tissue specific organ destruction. Aplastic anemia has also been reported to be associated with hepatitis A, B or non-A non-B hepatitis.32-35 It occurs several weeks to months after an episode of acute viral hepatitis. Zeldis et al36 have studied 229 patients of aplastic anemia of which 16 were positive for viral markers. From these, 13 were found to be associated with nonA non-B hepatitis, 1 case was positive for HBsAg and remaining two were hepatitis A positive. We have come across a case of acute hepatitis E infection, developing aplastic anemia and expired due to sepsis before giving any specific therapy. Two patients of agranulocytosis were treated with GMC-SF showed complete recovery with resolution of hepatitis. For patients of thrombocytopenia no any specific treatment was given. Thrombocytopenia disappeared with recovery from viral hepatitis.
Acute hemorrhagic and necrotising pancreatitis is a frequent finding in patients with fulminant hepatic failure at autopsy.37 Association of hepatitis A and acute pancreatitis is very rare.38-40 From our study, a young boy admitted with acute hepatitis A developed acute pancreatitis during hospital stay. His IgM anti HAV antibodies were found to be positive. Acute pancreatitis developing in acute viral hepatitis may be due to a direct cytopathic effect of the viruses or through the patient’s immune response.
In conclusion, extrahepatic manifestations of viral hepatitis are not very uncommon. They should be diagnosed with suspicion and antiviral therapy may be of great help in majority of them.
AcknowledgementWe are thankful to Medical research society, Bombay hospital for grant in aid for published study.