The Child-Turcotte-Pugh (CTP) and the MELD (Model for End-Stage Liver Disease) scores were designed to predict the outcome of decompressive therapy for portal hypertension. They were prospectively validated to predict mortality risk in patients with a wide spectrum of liver disease etiology and severity. Unlike the CTP score, the MELD score was derived from prospectively gathered data. Its calculation was based on serum bilirubin, serum creatinine, international normalized ratio (INR) and etiology of liver disease. Instituting a continuous disease severity score that de-emphasizes waiting time resulted in better categorization of waiting patients and enhanced transparency. The US instituted the MELD system in 2002 and soon thereafter, MELD-based liver allocation was adopted throughout the world including Latin America. The most significant impact of MELD-based policies has been the reduction of waiting-list mortality. In the years after implementation of the MELD system, several options have been proposed to improve the MELD score's accuracy. Adding serum sodium (MELD-Na) increased the accuracy of the score in predicting waiting list mortality, thus completing the original MELD score as a prognostic model in liver allocation. On the 20th anniversary of the creation of MELD score we present a brief account of its development, its use to stratify patients on the waiting list for liver transplantation as well as its adoption as liver allocation system .
Every hepatology fellow learns about the Model for End-Stage Liver Disease (MELD) and MELD-Sodium (MELD-Na) scores at the beginning of their training. These tools are the most widely used models to measure disease severity and predict short term outcomes in patients with liver disease. Now, having just observed the 20th anniversary of the original publication by Patrick Kamath et al in Hepatology [1] that described the MELD Score and its usefulness in predicting mortality in end-stage liver disease, we will review the path that led to these landmark developments. This history highlights an exciting era in hepatology, and beyond that, ushered in an entirely new field aimed at improving predictive modeling for severely ill patients.
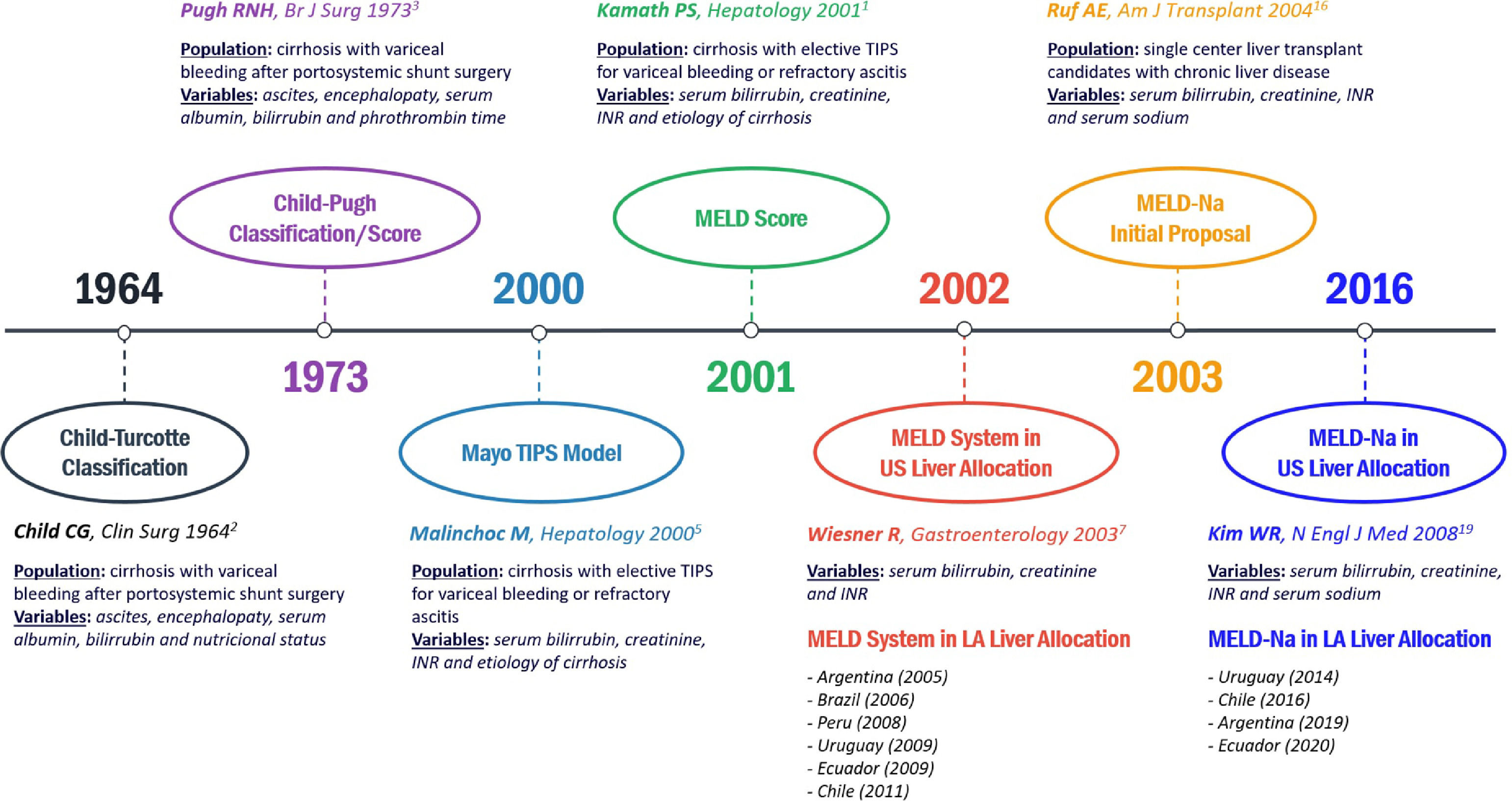
The initial attempts to predict outcome in end-stage liver diseaseAlthough Child and Turcotte were not the first to risk stratify patients undergoing shunt surgery to relieve portal hypertension, their classification system published in 1964 became the predominant method to assess prognosis in patients with cirrhosis [2]. They selected empirically five parameters (serum albumin, serum bilirubin, ascites, encephalopathy, and nutritional status) to which they attributed one of three risk levels each, and constructed a three stage “A”, “B”, or “C” classification. In 1972, Pugh modified the Child-Turcotte classification by substituting prothrombin time for nutritional status, thereby eliminating the most subjective element [3]. Several prospective studies assessing short and long-term prognosis in patients with cirrhosis and using appropriate statistical methods have confirmed the Child-Turcotte-Pugh (CTP) criteria as a useful clinical tool. However, the CTP classification had room for improvement [4]. Since its description, several efforts have been made to develop other prognostic models for cirrhosis by considering prospectively gathered data sets and proper statistical strategies.
The Mayo TIPS model, the origin of the MELD scoreIn their original article published in the year 2000, Malinchoc et al. [5] used a Cox proportional-hazards regression model to identify four variables (serum bilirubin, serum creatinine, international normalized ratio (INR) for prothrombin time, and the cause of the underlying liver disease) to calculate a risk score to assess the short-term prognosis of patients with liver cirrhosis undergoing an elective transjugular intrahepatic porto-systemic shunt (TIPS) procedure, which was called “Mayo TIPS model”. This model was derived from a heterogeneous group of 231 patients at 4 medical centers in the United States and validated against an independent data set of 71 patients in the Netherlands. The main finding of this study was that the Mayo TIPS model was superior to CTP score in predicting survival in this subset of patients [5]. Again, like the CTP score in its origins, the Mayo TIPS model was built to stratify patients undergoing surgical porto systemic shunts to relieve portal hypertension.
Validation of the Mayo TIPS model in advanced chronic liver diseaseBecause survival following portosystemic shunts was found to be predominantly determined by the severity of the underlying liver disease, hepatologists and surgeons hypothesized that the same model could be used as a prognostic indicator for survival for patients with advanced chronic liver disease. Thus, Kamath et al. subsequently validated MELD as a predictor of short term survival in diverse cohorts of patients with varying levels of liver disease severity, from liver units around the world [1]. The survival model was initially termed the “Mayo End-Stage Liver Disease” to acknowledge the affiliation of the investigators who created the model. However, during discussions leading to the establishment of MELD as the basis for prioritization of organs for liver transplantation, the name was changed to “Model for End-Stage Liver Disease''. Thus, the acronym “MELD” was kept, but association with a particular institution was removed, a decision that was thought would lead to wider acceptance of the model. To make it easier to interpret, policymakers modified the original MELD score by multiplying the score by 10 and rounding the result to the nearest integer.
Essentially, Kamath and colleagues found that: 1) the MELD score was highly predictive of death within 3 months in several cohorts of patients with varying degrees of liver disease severity, measured at different times, from different geographic locations; 2) inclusion of the more subjectively measured complications of portal hypertension (e.g. ascites, encephalopathy, or variceal bleeding) did not affect the accuracy of the MELD score and could be omitted from the formula and, 3) etiology of liver disease contributed very little to MELD's predictive power [1]. These three findings together validated an entirely objective new method of assessing liver disease severity.
The significant impact of this article was to validate that MELD score represented a more objective and accurate patient-specific method for stratifying patients based on clinical need and removed reliance on observer-biased assessments. The MELD model relies on objective and standardized laboratory tests, readily available, and reproducible worldwide. None of the parameters in the model were subjective or had political overtones, such as age or race, that might make its implementation controversial [6]. Moreover, its objective and patient-specific attributes made it possible to compare systems and centers across regions and countries that greatly enhanced overall transparency.
Wiesner et al, performed the last step in the journey to implement a MELD based system for liver allocation by validating that MELD score as an accurate predictor of mortality risk for patients waiting on the US liver transplant list at that time [7]. An additional modification in the MELD equation was added, so that all laboratory values <1 were rounded up to 1.0 to prevent coefficients with negative values, and based on data cited above, the etiology of liver disease variable was removed. Wiesner's team studied MELD values for 3437 adult liver transplant candidates entered on the US list at 2A or 2B status between November 1999 and December 2001. Of this cohort, 412 (12%) died during the initial 3 months of follow-up. Waiting list mortality increased proportionally with the MELD score at listing. The MELD score's ability to discern 3-month mortality from survivors was significantly better than the CTP score (C = 0.83 for MELD, compared with 0.76 for the CTP score, p < 0.001). These data confirmed that the MELD score at listing could accurately predict 3-month mortality among patients on the liver waiting list with chronic liver disease, and therefore could be used to prioritize waiting patients for allocation of donor livers.
The MELD liver allocation system: moving towards an evidence-based transplantation policyBefore 2002, the liver allocation policy in the US was based on CTP scores, considering only three defined categories for patients with chronic liver disease (status 2A, 2B and 3). Under this system, waiting time became a dominant factor in organ allocation. Furthermore, although CTP was undoubtedly appreciated by clinicians for many decades, it did not have much statistical basis in its development, nor did it undergo the rigorous validation across levels of disease severity or patient types that were applied in MELD development. In 2002, Freeman et al published that waiting time was not associated with increased death on the waiting list, lending further evidence that the allocation system in effect at the time was flawed [8]. At the time, observers noted that since waiting time was not reflective of the medical urgency for transplantation, and the CTP score had subjective elements that could be manipulated and were never validated for predicting mortality on a waiting list, there was a good opportunity to improve the system for prioritizing candidates waiting for donor livers.
In 2002, based on the preliminary work by Kamath, Wiesner, Freeman and others, the US's United Network for Organ Sharing/Organ Procurement and Transplantation Network (UNOS/OPTN) adopted a new liver allocation policy based on the MELD score with the elimination of waiting time as a major factor. The inherent advantages of the MELD score such as its ease of use, statistical validation, and the incorporation of objective and widely available laboratory tests facilitated its acceptance. Ongoing studies continued to support the fact that the MELD score is a significantly more accurate survival model in comparison to other models/scores used in patients with liver disease [9]. The fact that MELD was based on objective variables only was one of the factors that made it more attractive as a standard for organ allocation, since it minimizes the possibility of “gaming” the system. Another advantage of employing the MELD is that it is a continuous score allowing for much more granular stratification of waiting candidates’ mortality risk compared to the CTP's “A”, “B” or “C” ordinal categorization method.
One year after the implementation of the MELD based system, policymakers reported a reduction in waiting-list registration, waiting list mortality, and median waiting times and an increase in the number of patients transplanted within 30 days of listing compared with the previous year [10]. The investigators hypothesized that elimination of waiting time as a major criterion reduced the incentive to put patients on the list early in their disease. Because patients with the highest mortality risk received the highest priority, waiting list mortality was reduced and more patients were transplanted sooner after registration. Importantly, these improvements were not associated with any reduction in post-transplant patient or graft survival. Stimulated by these early results in the US, MELD-based liver allocation systems were widely adopted throughout the world including the Latin America region [11], (Fig. 1).
Evolution from original Child-Turcotte Classification to current MELD-Na score for prognosis assessment in chronic liver disease. References numbers are those of the reference list. MELD: Model for End-Stage Liver Disease. TIPS: transjugular intrahepatic porto-systemic shunt. LA: Latin America.
In the years after the initial description of the MELD score, many options were proposed to improve its accuracy. As was advocated by the early investigators, using a well-defined, well-publicized mathematical model that employs objective variables allows for transparency and invites new analysis, innovations, and interpretation of its results. Furthermore, as noted in earlier studies, the MELD score is not completely accurate for every patient with an indication for liver transplantation. Consequently, identification of patients who may not be well served by the MELD-driven allocation system is necessary, and delineation of objective, widely reproducible variables that help to better define these groups was and is essential for further refining the system.
In an elegant analysis by Merion et al., patients with an increasing MELD score were observed to have an increased risk of mortality, whereas those with a decreasing MELD score had lower risk of mortality, even if their MELD scores were identical at a single point in time [12]. Thus, the change in MELD score (called “delta-MELD”) was proposed to add prognostic information to the MELD score, but it failed to achieve significance in the multivariable analysis, especially when acute increases in MELD score in the last few days of life were excluded [12].
Other studies showed that serum creatinine was not always an accurate marker of renal function in cirrhosis, since it is influenced by muscle mass, protein dietary intake, age, ethnicity, and gender [13]. In addition, previous data from Arroyo and colleagues showed that serum sodium is an earlier and more sensitive test than creatinine to detect circulatory dysfunction resulting in renal failure and/or death during the course of chronic liver disease. Their study, published in 1976, found that patients with hyponatremia had significantly higher plasma concentrations of epinephrine, higher aldosterone and renin activity, significantly reduced mean arterial pressure, and elevated resistance of renal arteries when compared to patients without hyponatremia [14].
In 2003, a consensus conference was held to analyze MELD/PELD liver allocation. At this conference, work by Ruf et al. was presented suggesting that hyponatremia could serve as a surrogate marker for severity of ascites and renal dysfunction in patients with chronic liver disease [15,16]. This study described 194 adults with cirrhosis listed for liver transplantation at a single center in Argentina. All patients with hyponatremia (serum sodium ≤ 130) had ascites. Both hyponatremia (as a binary, yes/no variable) and serum sodium (as a continuous variable) were significant predictors of 3-month waiting list mortality. In addition, these investigators showed that adding sodium to the MELD calculation (coined as the MELD-Na score) significantly increased the accuracy of the score in predicting waiting list mortality [17].
Similar to the three MELD score blood tests (bilirubin, creatinine, INR), serum sodium is an objective, quantitative, and easily obtainable laboratory test, and therefore attractive for incorporation into a mathematical formula such as the MELD. Honoring the established philosophy of validating models proposed for liver allocation, UNOS/OPTN policymakers prospectively collected serum sodium values on registered patients and incorporated these into the existing MELD score system to confirm that inclusion of sodium would improve the efficiency of the MELD score for allocating donor livers [15]. In the following years, numerous multicentric and national database studies confirmed that including sodium in the MELD score calculation does improve its predictive accuracy [18]. In a larger study, Kim et al in 2008, used the US national database of liver transplant candidates to build a prediction model based on data from 2005 and validated the model using 2006 data [19]. Consistent with previous work, these investigators confirmed that both the MELD score and the serum sodium concentration were predictive of death at 90 days among patients on the waiting list. In addition, they described a significant interaction between the MELD score and serum sodium concentration indicating that the mortality risk for patients with low MELD score and low sodium was higher than that predicted by the MELD score alone. Their analysis suggested that as many as 7% of waiting-list deaths could be averted if the MELD-sodium score was used for liver allocation [19]. As a result, in 2016 the OPTN introduced a new policy to add serum sodium to the MELD score equation for the allocation of liver donors in the US. Again, based on extensive validation and transparent sharing of the data relative to MELD-Na, the improved MELD-Na score was a change that has been adopted in Latin America and the rest of the world [11] (Fig.).
Application of MELD score beyond the end-stage liver diseaseMany other investigators have tested the ability of the MELD score to predict short-term survival for patients with acute liver failure, alcoholic hepatitis, acute on chronic liver failure and patients with cirrhosis undergoing surgery other than liver transplantation [20]. Additionally, since hepato-renal dysfunction is common in patients with acute heart failure, more recent studies have established that the MELD score and modified MELD versions, such as the MELD-XI (without INR), MELD-Na, and the new “cardiology” developed MELD-albumin score are relatively accurate for predicting all-cause mortality risk in patients with acute heart failure [21].
ConclusionsBased on its ability to stratify patients with end-stage liver disease according to their short-term mortality, the MELD score has been recognized as a major contribution to the daily practice of hepatology. Successful implementation of MELD-based liver allocation in the United States in 2002 has been followed by its worldwide adoption, attesting to its validity, thus earning its spot in hepatology history. Although various modifications have been proposed, through the well-established practice of prospective validation, the MELD-Na still meets the test of time and now is an international standard for liver transplant allocation systems. Nonetheless, MELD-Na is by no means a perfect system, and hepatologists are quite aware of its limitations in certain subsets of patients. Thus, efforts to further refine this score must continue as we constantly try to improve our ability to predict mortality in patients with end-stage liver disease.
AbbreviationsMELD Model for End-Stage Liver Disease MELD-Sodium Child-Turcotte-Pugh international normalized ratio transjugular intrahepatic porto-systemic shunt United State United Network for Organ Sharing/Organ Procurement and Transplantation Network Pediatric End-Stage Liver Disease
Thanks to Geraldine Ruf for her contributions in helping us maintain the excitement and love for hepatology and its history.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.