The differential diagnosis of fever of unknown origin (FUO) includes infectious, neoplastic, rheumatic-inflammatory and miscellaneous diseases. We report the case of a 35-year-old man with FUO caused by Q fever. A liver biopsy showed the characteristic fibrin-ring lipogranulomas compatible with Q fever. The serologic tests confirmed the diagnosis of acute infection by Coxiella burnetii. The therapeutic response was excellent. In conclusion, we described a patient with acute Q fever and granulomatous hepatitis.
Fever of Unknown Origin (FUO) is defined as fever at/or above 38.3 °C (101 °F) for 3 weeks or more that remains undiagnosed after 3 days of in-hospital testing or during two or more outpatient visits. FUO may be divided into four general categories based on the etiology:1
- •
Infectious.
- •
Rheumatic-inflammatory.
- •
Neoplastic.
- •
Miscellaneous disorders.
A comprehensive history and physical examination is the key to establishing a diagnosis, but it can remain undetermined in up to 30% of cases of FUO.2 The aim of this case report is to present the diagnostic approach and histological characteristics of a patient with FUO due to granulomatous hepatitis caused by Q fever.
Clinical DataA 35 year-old man with no relevant medical history was admitted at the Medica Sur Hospital with a four weeks clinical picture encompassing moderate to severe abdominal pain, fever up to 40 oC, diaphoresis, weakness and fatigue. Two weeks prior to admission, he was hospitalized and diagnosed with urinary tract infection in another institution. He was treated with intravenous ciprofloxacin 400 mg BID during 5 days and discharged with oral cipro-floxacin for 5 days more. Because fever and diaphoresis persisted every day; he entered the emergency room at our Hospital. He was clinically stable, with fever and mild diffuse abdominal pain. The laboratory tests showed leukocytosis and neutrophilia (leukocytes 12,500 cells/mcL, neutrophils 9,200 cells/mcL), hyperazooemia (BUN 32.8 mg/dL, creatinine 2.29 mg/dL, BUN/creatinine ratio 14.9, fractional excretion of sodium 0.29%), hypertransaminasemia (ALT 92 U/L, AST 104 U/L), cholestasis (AF 319 U/L, GGT 352 U/L) and hyperbilirrubinemia (TB 2.43 mg/dL, IB 2.43 mg/dL). A complete abdomen ultrasound was performed but no alterations were found. The patient was hospitalized and started on intravenous hydration. During the hospitalization, evening fever persisted; consequently, a viral hepatitis panel, blood and urine cultures, ELISA test for HIV, PPD, serology for EBV, CMV and immunologic tests were performed. When renal function became normal, a neck, thorax, and abdominal CT-scans were performed. Image and laboratory tests were all found without alterations, therefore, an ultrasound-guided liver biopsy was carried out.
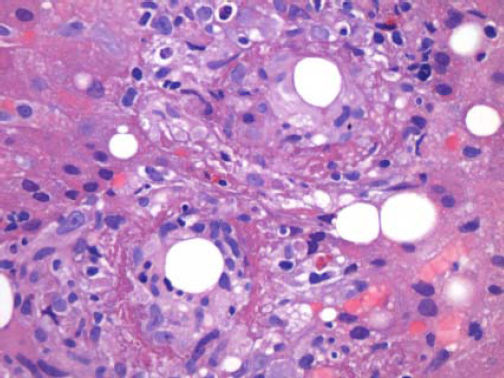
Histological findingsThe hematoxylin and eosin stained sections of the liver showed numerous granulomas, some of which were confluent (Figure 1). These granulomas were composed by a central lipid vacuole surrounded by abundant lymphocytes and histiocytes as well as occasional giant cells. Between these inflammatory cells a prominent fibrin-ring was seen (Figure 2). The fibrin-ring was fucsinophilic and Periodic Acid Schiff (PAS) positive (Figure 3). The Masson’s and the Phosphotungstic acid-haematoxylin (PTAH) stains were also positive (Figure 4). The remaining liver parenchyma showed a macro and microvesicular grade 1 steatosis without hepatic fibrosis. The Gram, PAS, Ziehl-Neelsen, Warthin-Starry and Auramina-Rodamina stains were negative. The morphologic diagnosis was compatible with Q fever.
Before the antimicrobial treatment, a serologic test for Coxiella Burnetti was performed. A treatment with Doxyciclin 100 mg orally BID was initiated immediately. The clinical course improved immediately and fever and other symptoms ceased completely after the treatment. After two weeks, the serologic tests for Coxiella Burnetti were positive with IgG phase 1 = 1:64, IgG phase 2 > 1:1024, IgM phase 1 > 1:1024, IgM phase 2 > 1:1024, IgA phase 1 < 1:16, and IgA phase 2 < 1:16. These results indicated acute Q fever. The patient is asymptomatic 6 weeks after diagnosis.
DiscussionQ fever is a worldwide zoonosis, caused by Coxiella burnetii,3 which is an obligate intracellular Gram-negative bacterium. The genus Coxiella is morphologically similar to Rickettsia, but with a variety of genetic and physiological differences.4
The incidence of Q fever is unknown but it could be greater than generally estimated owing to a nonspecific clinical presentation. The Center for Disease Control and Prevention reports an average of approximately 50–60 cases of Q fever in the United States each year, and the average annual reported incidence is 0.28 cases per million. In Mexico, there are few reported cases of Q fever, despite the adequate environmental conditions for its existence and dissemination.5 Inhalation of aerosols contaminated with the bacterium can infect humans, but transmission through ingestion of contaminated milk and cheese, getting ticks bites, or sexual intercourse with an infected person has also been reported.6 The disease is characterized by many nonspecific acute and chronic manifestations.7 Acute infection results in either subclinical seroconversion or a flu-like syndrome with fever, headache, fatigue, malaise, pneumonia or granulomatous hepatitis.6,8 Chronic Q fever occurs in approximately 1% to 5% of patients. The most frequent presentations are endocarditis, osteomyelitis, aneurysms or hepatitis.7
Because Q fever has a broad-spectrum of clinical and laboratory data, the diagnosis represents a great challenge for clinicians. In the presence of FUO plus a compatible clinical profile, serologic tests for Coxiella burnetii must be considered for diagnosis.
In regards to the diagnostic methods through serum antibodies, it is important to consider that C. burnetii presents a phenomenon called phase variation. Analogous to the lipopolysaccharide phases of Enterobacteriaceae organisms, in C. burnetii this phenomenon has 2 phases in which membrane antigens change and several types of antibodies are generated. In the phase I (smooth), bacterial isolates from naturally infected and laboratory-infected eukaryotic cell hosts are virulent and present lipopolysaccharides that protect the microorganism from the host’s defense mechanisms. In the phase II (rough), isolates obtained after repeated passages through embryonated hens’ eggs are purified into an avirulent variant characterized by truncated lipopolysaccharides and absence of protein cell surface determinants. Phase II antibodies are positive in acute Q fever, whereas phase I antibodies remain elevated in chronic disease.9
In regard to the histopathological findings in Q fever, it is interesting to highlight that the development of a local inflammatory response and the inability to degrade the infectious agent, induces the accumulation of epithelioid cells, including macrophages and mononuclear cells. The result is a granulomatous inflammatory reaction that in the liver can be seen as “doughnut granulomas”, characteristic of Q fever. Fibrin ring-granulomas in the liver are characteristic of Q fever, but they are not specific. In fact, they have also been described in viral infections (e.g., CMV, EBV, HAV, HCV), drugs (allopurinol consumption), parasites (leishmaniasis) and neoplastic diseases (Hodgkin’s lymphoma).10
With respect to the pharmacotherapy, the treatment of choice in acute and chronic cases is doxycycline for at least 14 days. In chronic cases serology must be followed during treatment administration.
In this case, the clinical and laboratory data were the intense febrile syndrome and the absence of an identifiable infection site; the aminotransferases elevation and negativity of autoantibodies tests and viral hepatitis profile suggested undetermined hepatic pathology that indicates liver biopsy. Hepatic fibrin-ring lipogranulomas are highly suggestive but not specific of Q fever; other possible causes of granulomas (other infections, drugs, cancer), were clinically and histopathologically excluded. Serologic test confirms C. burnetii infection. Favorable response to treatment and complete clinical improvement ruled out the possibility of associated comorbidities.
In conclusion, we described a patient with acute Q fever and granulomatous hepatitis. It is one of the few cases of this disease reported in Mexico. In our country, Q fever is probably an underdiagnosed cause of fever of unknown origin and it is important to consider a liver biopsy in patients with UFO and liver function abnormalities in the absence of viral or immunological causes.
Abbreviations- •
ALT: alanine aminotransferase.
- •
AST: aspartate aminotransferase.
- •
AF: alkaline phosphatase.
- •
GGT: gamma-glutamyl transpeptidase.
- •
TB: total bilirubin.
- •
IB: indirect bilirubin.
- •
HIV: human immunodeficiency virus.
- •
PPD: purified protein derivative.
- •
EBV: Epstein-Barr virus.
- •
CMV: cytomegalovirus.
- •
BID: twice a day.
- •
HAV: hepatitis A virus.