Thoracic involvement (TIHE) is one of the evolutionary complications of hepatic echinococcosis (HE).
AimThe aim of this study was to describe the clinical characteristics and postoperative morbidity (POM) of a series of patients with TIHE treated surgically.
Material and methodsSeries of cases of patients treated for TIHE between 2000 and 2014 in the Hospital Regional and Clínica Mayor in Temuco, Chile, with a minimum 12-month follow-up. The outcome variable was “development of POM”. Descriptive statistics were used.
ResultsThe series was composed of 37 patients with a mean age of 53.2 ± 47.4 years (51.4% female). Mean cyst diameter was 19.4 ± 15.5 cm, and 75.7% of the lesions were located in the right hepatic lobe. The most frequent surgical technique used for the cyst was subtotal pericystectomy (56.8%); the residual cavity was treated by capitonnage (27.0%) or omentoplasty (21.6%), and a phrenoplasty with or without prosthetic material was performed for the TIHE. Mean hospital stay was 6.0 ± 5.7 days and follow-up was 61.4 ± 79.9 months; a mortality rate of 2.7% (one patient) and a POM of 24.3% (9 patients) were verified.
ConclusionTIHE is an uncommon evolutionary complication of HE associated with significant POM rate.
One of the evolutionary complications of hepatic echinococcosis (HE) is thoracic involvement (TIHE). It is an uncommon condition, which simultaneously involves the liver, diaphragm and lung secondary to the migration of a hepatic hydatid cyst. Its estimated prevalence is between 2% and 11%.1,2
It is a difficult clinical condition to treat due to, among other things, the cyst in transit sometimes being infected, producing a secondary hepatic abscess,3,4 or it is in direct communication with the bronchial tree, which manifests as a cough, dyspnea, thoracic pain and possibly biliptysis. There may also be coexistent cholangiohydatidosis.4,5 All these situations can exacerbate the risk of postoperative morbidity (POM).4,6 The controversy surrounding the ideal surgical access to treat TIHE -thoracic, abdominal or thoracoabdominal1,7,8 must also be mentioned; however, it seems logical to suggest that the technique should depend on the location of the lesion, the condition and size of the cyst, and the experience of the surgical team. In this respect, evidence from a systematic review proposes that when common bile duct drainage is required, and it may be sufficient to treat a direct rupture into the bronchi, an abdominal approach is mandatory.9
Diagnosis is usually made through the presence of clinical manifestations, thorax x-rays, computerized axial tomography and fibrobronchoscopy;10,11 nevertheless, in some cases it may be an intraoperative finding in oligosymptomatic patients.
Surgery continues to be the treatment of choice, with a reported surgical mortality of up to 9.6%;1,7,bib0045, 12-16 the prognosis worsens with a second and third surgery, which is associated with an increase in these numbers of up to 20%.7
The aim of this study was to describe the clinical characteristics and POM of a series of patients with TIHE treated surgically.
This manuscript was written according to the guidelines of the MInCir initiative for the reporting of out-comes of descriptive observational studies.17
Material and Methods- •
Study design. Prospective case series with follow-up.
- •
Setting. The study was conducted in the Emergency Services of the Hospital Regional and the Clínica Mayor in Temuco, Chile between January 2000 and October 2014.
- •
Participants. Non-probabilistic sample of consecu-tive cases of patients operated on for TIHE by the first author (CM) in the study period. No patients were ex-cluded.
- •
Study protocol. All patients underwent general diag-nostic tests, liver function, immunodiagnostics, abdominal ultrasonography (according to the WHO classification)18 and thorax x-ray or thoracic CT-Scan to determine coexistent pulmonary disease. After hospital discharge patients were followed up on at least at months 1, 6, 12, 24, 36, 48 and 60 with clinical monitoring, lab tests, immunodiagnostics, abdominal ultra-sonography and thorax x-ray.
- •
Variables. The outcome variable was “development of POM”, dichotomously (yes/no), and applying the Clavien & Dindo proposal, measured at least 12 months after surgery.
- •
Treatment protocol. Cyst surgical techniques applied were total or subtotal pericystectomy and right hepatic lobectomy, phrenoplasty with or without mesh and lung repair as needed. Surgical access was gained in all cases via a J laparotomy.19
- •
Biases. At the time of recruitment as well as at the time of the clinical check-ups, biases were reduced with a complete follow-up of the patients comprising this series for at least 12 months (the last patient re-cruited), and data collection was blinded.
- •
Sample size. As this was an observational and de-scriptive study, sample size was not considered.
- •
Statistical methods. Data collection was done by an independent researcher (TO) and analyzed with the Stata 11.0/SE® program. Descriptive statistics were used, applying measures of central tendency and dispersion (means and standard deviation, medians and extreme values). The prevalence of TIHE in patients that had HE was calculated and the projected incidence rate for the period in general population was also cal-culated.
- •
Ethical aspects. The ethical guidelines for research involving human beings defined by the Helsinki Dec-laration were observed.20 All patients gave their in-formed written consent.
- •
Funding. This study had no formal sources of funding.
- •
Definitions. TIHE was defined as the involvement of liver, diaphragm and the pleura (parietal or visceral) by a hepatic hydatid cyst.1,21 We endeavored to categorize cysts according to the proposal by Gómez, et al.,14 in Grades I to V (Figure 1); however, in some cases, this proposal did not adequately represent the findings. Cysts were therefore grouped according to the concept of “anatomic-surgical lesions of TIHE”, defined as:
- a)
Adherent cyst (strong adhesions between the cyst surface and the diaphragm, but without rupture of him).
- b)
Hydatid transit (cyst perforates the diaphragm in-vading the thoracic cavity).
- c)
Hydatid pleura without bronchial rupture (vesicu-lation inside the thoracic pleura).
- d)
Hydatid pleura with rupture a bronchus (cyst is connected to the bronchial tree).
- e)
Hydatid pleura with rupture of the biliary tract (cyst perforates the diaphragm and grows inside the thoracic cavity and communication with the bile duct).
- f)
Pleural-cystic-biliary fistula (cyst is connected to the bronchial tree and the bile duct as a chronic bronchial fistula)12 (Figure 2.
- a)
In the study period there was a total of 351 patients with HE operated on by the first author, of which 37 had TIHE, representing a prevalence of TIHE in the total series of 10.5%, and a projected incidence rate for the general population of 0.82 per 100,000 inhabitants per year.
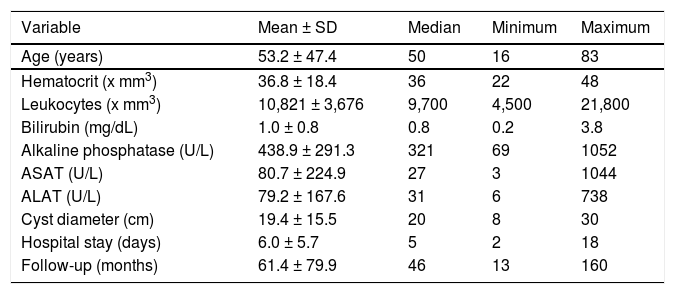
The patients had a mean age of 53.2 ± 47.4 years (16 to 83 years) and 51.4% were female. Eight (21.6%) had a history of surgery for lung and hepatic echinococcosis (4 cases of each) and 14 (37.8%) had comorbidity, including coronary heart disease in 6 cases (Tables 1 and 2). Only 5 patients (13.5%) were asymptomatic and of the others 7 (18.9%) had vomica, 4 (10.8%) developed hemoptysis, and 3 (8.1%) had bile-stained sputum (Table 1).
TIHE. Distribution of continuous variables (n = 37).
| Variable | Mean ± SD | Median | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 53.2 ± 47.4 | 50 | 16 | 83 |
| Hematocrit (x mm3) | 36.8 ± 18.4 | 36 | 22 | 48 |
| Leukocytes (x mm3) | 10,821 ± 3,676 | 9,700 | 4,500 | 21,800 |
| Bilirubin (mg/dL) | 1.0 ± 0.8 | 0.8 | 0.2 | 3.8 |
| Alkaline phosphatase (U/L) | 438.9 ± 291.3 | 321 | 69 | 1052 |
| ASAT (U/L) | 80.7 ± 224.9 | 27 | 3 | 1044 |
| ALAT (U/L) | 79.2 ± 167.6 | 31 | 6 | 738 |
| Cyst diameter (cm) | 19.4 ± 15.5 | 20 | 8 | 30 |
| Hospital stay (days) | 6.0 ± 5.7 | 5 | 2 | 18 |
| Follow-up (months) | 61.4 ± 79.9 | 46 | 13 | 160 |
Preoperative studies revealed in particular an alteration of the liver tests (Table 1). Imaging showed the lesions were solitary in 59.5% of the cases, and located mainly in the right lobe (75.5%) with a mean cyst diameter of 19.4 ± 15.5 cm (8 to 30 cm). Most cysts found were CE3 (29.7%) and CE4 (24.4%). Related to radiological findings, in 3 cases the x-ray was normal, and the other cyst images and diaphragmatic ascent were verified (Table 1).
Concomitance was found with other evolutionary complications of HE, including in particular the coexistence of liver abscess of hepatic origin (Table 2). Biliary communications were verified in 26 patients (70.3%) (Tables 1 and 2).
TIHE. Distribution of clinical variables (n = 37).
| Variable | Cases, n (%) |
|---|---|
| Symptoms and signs* | |
| Asymptomatic | 5 (13.5) |
| Pleural effusion | 11 (29.7) |
| Cough and sputum | 11 (29.7) |
| Dyspnea | 8 (21.6) |
| Vomica | 7 (18.9) |
| Hemoptysis | 4 (10.8) |
| Bile-stained sputum | 3 (8.1) |
| Jaundice | 1 (2.7) |
| Concomitant morbidity | |
| None | 23 (62.2) |
| Coronary heart disease | 6 (16.2) |
| Coronary heart disease + Diabetes mellitus | 2 (5.4) |
| Pregnancy | 2 (5.4) |
| Cholelithiasis | 2 (5.4) |
| Other location of echinococcosis | |
| None | 27 (72.9) |
| Pulmonary | 5 (13.5) |
| Peritoneal | 3 (8.1) |
| Peritoneal and pelvic | 1 (2.7) |
| Splenic | 1 (2.7) |
| Number of cysts | |
| One | 22 (59.5) |
| Two | 5 (13.5) |
| Three or more | 10 (27) |
| Location of the main lesion | |
| Right lobe | 28 (75.7) |
| Left lobe | 2 (5.4) |
| Bilateral | 7 (18.9) |
| Radiologic findings | |
| Normal | 3 (8.1) |
| Cyst image | 16 (43.2) |
| Diaphragmatic ascent | 18 (48.6) |
| Ultrasonography findings | |
| CE1 | 5 (13.5) |
| CE2 | 7 (18.9) |
| CE3 | 11 (29.7) |
| CE4 | 9 (24.4) |
| CE5 | 5 (13.5) |
| Concomitant evolutionary complications | |
| None | 23 (62.2) |
| Liver abscess of hydatid origin | 12 (32.4) |
| Cholangiohydatidosis + Liver abscess | 1 (2.7) |
| Cystogastric fistula and anaphylaxis | 1 (2.7) |
| Biliary communications | |
| None | 11 (29.7) |
| One | 20 (54.1) |
| Two or more | 6 (16.2) |
With respect to the type of lesions verified in this series, although a higher percentage (23 cases, 62.2%) of the lesions were consistent with the proposal by Gómez, et al., others were only partially consistent or were “non-classifiable” (14 cases, 37.8%). Based on these find-ings, we grouped the cases according to the type of anatomic-surgical lesion of TIHE (Figure 2), according to which the most frequent manifestations were what we call “adhered cyst” and (11 cases, 29.7%) and “hydatid transit” (12 cases, 32.4%).
Anatomic-surgical lesions of TIHE. A. Adhered cyst (n = 11). There are strong adhesions between the cyst surface and the diaphragm, but without rupture of him. Equivalent to Grade I of the proposal by Gómez, et al. B. Hydatid transit (n = 12). Cyst perforates the diaphragm invading the thoracic cavity. The diaphragmatic defect needs repair. Equivalent to Grade I of the proposal by Gómez, et al. C. Hydatid pleura without bronchial rupture (n = 4). Vesiculation inside the thoracic pleura. Cyst perforates the diaphragm and grows inside the chest, with or without implant of daughter vesicles. Equivalent to Grade III of the proposal by Gómez, et al. D. Hydatid pleura with rupture a bronchus (n = 4). Parenchymal lung disease occurs (e.g. atelectasis). Cyst is connected to the bronchial tree. Partially equivalent to Grade IV of proposal by Gómez, et al. E. Hydatid pleura with rupture of the biliary tract (n = 3). Cyst perforates the diaphragm and grows inside the thoracic cavity, with or without implant of daughter vesicles. Furthermore, the cyst communicates with the bile duct, causing or not cholangiohydatidosis, with or without secondary cholangitis. F. Pleural-cystic-biliary fistula (n = 3). There is parenchymal lung disease. Cyst is connected to the bronchial tree (as a chronic bronchial fistula) and the bile duct. Partially equivalent to grade V of the proposal by Gómez, et al.
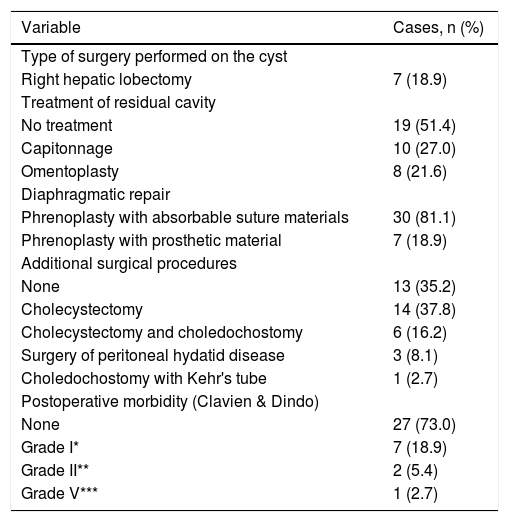
The surgical procedure performed most frequently on the cysts was the subtotal pericystectomy (56.8%), and the residual cavity (what remained) was treated by capitonnage (27.0%) or omentoplasty (21.6%).
To this was added a phrenoplasty with continuous sutures of absorbable material in 30 cases (81.1%). In the rest it was necessary to install prosthetic material made of polypropylene that adhered to the edges of the remaining diaphragm with loose sutures of the same material (Table 3). In no case was a pulmonary resection necessary. Treatment of the biliobronchial fistula with the subsequent cessation of symptoms was associated solely with the elimination of the hepatic cyst and the diaphragmatic repair, which was applied only in patients with continuous polyglycolic acid suture. In addition, a cholecystectomy (with or without choledochostomy) was performed on 54.0% of the patients (Table 3).
TIHE. Distribution of surgical variables (n = 37).
| Variable | Cases, n (%) |
|---|---|
| Type of surgery performed on the cyst | |
| Right hepatic lobectomy | 7 (18.9) |
| Treatment of residual cavity | |
| No treatment | 19 (51.4) |
| Capitonnage | 10 (27.0) |
| Omentoplasty | 8 (21.6) |
| Diaphragmatic repair | |
| Phrenoplasty with absorbable suture materials | 30 (81.1) |
| Phrenoplasty with prosthetic material | 7 (18.9) |
| Additional surgical procedures | |
| None | 13 (35.2) |
| Cholecystectomy | 14 (37.8) |
| Cholecystectomy and choledochostomy | 6 (16.2) |
| Surgery of peritoneal hydatid disease | 3 (8.1) |
| Choledochostomy with Kehr's tube | 1 (2.7) |
| Postoperative morbidity (Clavien & Dindo) | |
| None | 27 (73.0) |
| Grade I* | 7 (18.9) |
| Grade II** | 2 (5.4) |
| Grade V*** | 1 (2.7) |
No patients were previously treated with percutaneous drainage.
A total of 12 cases required a chest tube. Reasons for chest tube insertion included: adhered cyst (1), hydatid transit (2), hydatid pleura without bronchial rupture (3), hydatid pleura with rupture a bronchus (2), hydatid pleura with rupture of the biliary tract (2), and pleural-cystic-biliary fistula (2).
Patients with pulmonary echinococcosis (n = 5) were treated for TIHE between 1 and 3 months after discharge. Those with more than one hepatic cyst (15 cases, 40.5%) and with other abdominal locations (5 cases, 13.5%) were treated for the TIHE during the same surgery.
Hospital stay was 6.0 ± 5.7 days (Table 1). POM was 24.3% (9 patients), most of which was Clavien & Dindo 1 or 2 (Table 3). The etiology of POM was: pulmonary complications (5 cases of atelectasis and 1 of pneumonia, 16.2%), surgical site infection (2 cases, 5.4%) and cardiac arrhythmia (1 case, 2.7%). There was no need for reoperations and the mortality rate was 2.7% (one patient).
The death was secondary to a septic respiratory distress syndrome, which occurred in the immediate postoperative period in a patient with concomitant liver abscess of hydatid origin, which progressed to severe pneumonia (there was no evidence of spillage of cyst contents).
With a mean and median follow-up of 61.4 ± 79.9 and 46 months respectively, no recurrence was verified.
DiscussionTemuco is the capital of a region of 700,000 inhabitants, an area endemic for HE; and it Regional Hospital is the referral center for all the hospitals in the region, and therefore attends not only a considerable number of patients, but also most of the patients with complicated HE.
Evolutionary complications of HE are defined as the development of complications associated to the evolution of a HE. These can be related to infection of the cyst (liver abscess of hydatid origin); or rupture and migration to other organs or spaces, such as the bile duct (cholan-giohidatidosis with or without cholangitis), to the thorax (thoracic involvement), or to the peritoneum with peritoneal seeding with or without anaphylaxis.4,21
After searching for primary studies in the Clinical Evidence, PubMed, SCOPUS, and WoS databases, the EM-BASE, Google Scholar and TRIPdatabase search engines, as well as the BIREME and SciELO libraries, we determined that there are very few studies concerning TIHE. These deal with a report of isolated cases,2,10,22-37 a retro-spective series of cases and a few treated patients,38-44 or they allude to the subject indirectly, i.e., a series of patients treated for HE, among which some of the cases reported were TIHE.31,45-50 In addition, the literature review found only 11 case series with more than 20 patients1,7,8,12,13-16,15-53 (one of these only 19 cases, which we included in this subgroup for its contribution to the subject, which is the proposal for a classification of the lesions14) (Table 4). Based on these data, it may be concluded that the number of patients with TIHE reported in the literature in the databases consulted is about 535 cases (including those series in which patients with HE and TIHE are mixed).31,45-51
TIHE. Published series with over 20 patients treated (n = 11).
| Author, year | Cases (n) | Study period | Surgical access d | Cyst iameter (cm)* | Hospital stay | POM (%) | Mortality (%) | Recurrence (%) | Follow-up (years)† |
|---|---|---|---|---|---|---|---|---|---|
| Yacoubian, 197652 | 20 | NR | Thoracophreno-Laparotomy | NR | NR | 55.0 | NR | NR | 2.4 |
| Yuste, et al., 198453 | 21 | NR | Diverse accesses§ | NR | NR | 71.4 | 14.3 | NR | NR |
| Pinna, et al., 199016 | 25 | 1983-1988 | Thoracophreno-Laparotomy | NR | 20 | 20.0 | 0.0 | NR | NR |
| Castillo, et al., 199512 | 42 | 1984-1994 | Thoracophreno-Laparotomy | 8.6 | NR | 38.0 | 2.4 | 9.5 | NR |
| Gómez, et al., 199514 | 19 | 1974-1994 | Laparotomy | 11.6 | NR | 38.1 | 0.0 | 5.3 | 8.3 |
| Baquerizo, et al., 199851 | 95 | 1964-1996 | Thoracotomy | NR | NR | 8.7 | 1.8 | NR | NR |
| Kabiri, et al., 200115 | 123 | 1990-1999 | Thoracotomy‡ | NR | 20 | 14.6 | 8.9 | 0.8 | 8.5 |
| Kilani, et al., 20011 | 40 | 1984-1997 | Thoracotomy‡ | NR | NR | 35.0 | 7.5 | NR | NR |
| Gerazounis, et al., 200213 | 21 | 1979-1999 | Thoracotomy | NR | NR | 9.5 | 9.5 | NR | 9.5 |
| Tocchi, et al., 20077 | 31 | 1969-1999 | Diverse accesses§ | 8.4 | 17.6 | 58.1 | 9.6 | NR | 4.0 |
| Manterola, et al., 20098 | 23 | 1997-2007 | Laparotomy | 20 | 5 | 26.0 | 4.3 | 0.0 | 5.9 |
The incidence found in this study is similar to others previously reported.1,12,14 Consistent with the literature, the greatest frequency of location was the right hepatic lobe,7,13,14 and it is worth noting that the median of the diameter corresponds to large cysts (20 cm), a variable with smaller values in other series.7,14 In terms of the type of cysts found, in most of the series Gharbi's classification was used, rather than the World Health Organization proposal,18 which is why it is not so simple to comment on this variable.
The low frequency of biliobronchial fistula is also interesting. This is a rare entity which is usually only reported as isolated cases;10,25,27,28,33,34,42 however, in some series it appears as a frequent complication in patients with TIHE.15
The surgical access is controversial, because there are series in which a thoracotomy was used,1,13,15 others a laparotomy,8,14 and others with mixed surgical access, i.e., thoraco-phreno-laparotomy12,16,52 or depending on the patient, surgical access via thorax or abdomen.7,16 We preferred the abdominal route given the high prevalence of evolutionary complications of HE concomitant to TIHE (hepatic abscess of hydatid origin [9 cases, 39.1%], cholangiohydatidosis [1 case, 4.3%], cystogastric fistula and anaphylaxis [1 case, 4.3%]). A J laparotomy was used for this, because the surgical access obtained is suitable for the adequate treatment of patients with hepatobiliary pathology, and because it is a laparotomy with none of the major morbidity reported for other surgical access types (subcostal laparotomy, midline laparotomy, etc.).19
The type of surgery performed on the cyst was similar to other subtotal and total pericystectomy series (21.1% to 100.0%).1,7,8
Cholecystectomy was performed in 54.0% of patients. However, this figure should be ungrouped as follows: In 6 cases (16.2%), cholecystectomy was part of the treatment of cholangiohydatidosis and biliary communications (when there were two or more of them). In the remaining 14 cases (37.8%), cholecystectomy was performed due to the coexistence of cholelithiasis (two patients, 5.4%), gallbladder cholesterolosis diagnosed in the intraoperative (four patients, 10.8%) and in those patients in whom the gallbladder was closely related to the cyst, even forming part of the pericystic (eight cases, 21.6%).
Both the reported POM (9.5% to 58.1%) and the published mortality (0.0% to 12.5%)1,7,8,12-16,42 have a wide range, which could be influenced by many variables, e.g., date of publication, number of cases treated, heterogeneity of the published series, experience of the surgical team, surgical access route (for example: the series of thoracotomy,1,12,13,15,53 which reported POM figures on average higher than those of the laparotomy;8,14 the same for those cases where it was necessary to perform a concomitant pulmonary resection due to parenchymal affectation and biliobronchial fistula, etc. (in which a higher POM was reported).
The etiology of POM revealed septic phenomena and postoperative intrathoracic collections, the reported frequency of which is between 2.5% and 25.8%.1,7,8,15,16 With regard to infection of the surgical site, figures have been reported between 3.3% and 17.5%.1,8,15 It is known that close adhesion between the cyst and the diaphragm some-times cause iatrogenic diaphragmatic openings during surgery (usually during the detachment of the cyst dome from the diaphragm), which determines an increase in surgical time and a potential increase in the development of POM.
The causes of mortality in these patients are also related to sepsis, acute respiratory failure and pulmonary thromboembolism.1,8,15
Finally, we can say that the described treatment protocol constitutes a valid surgical alternative in patients with TIHE because it can offer satisfactory results in terms of POM, hospital stance and recurrence. Nevertheless we think these results have to observe cautiously, because they correspond to a reference center for the treatment of HE, so they are not necessarily reproducible by any surgical group.
ConclusionTIHE is an uncommon evolutionary complication of HE associated with significant POM rate respect the results observed in patients with non-complicated HE.
AbbreviationsHE: hepatic echinococcosis.
POM: post-operative morbidity.
TIHE: thoracic involvement of HE.
None.
Potential Conflicts of InterestNone.